Epidemiology: The Cornerstone of Community Health Nursing Practice
Understanding the Science Behind Population Health and Disease Control
Table of Contents
- Introduction to Epidemiology in Community Health Nursing
- Time Trends and Fluctuations in Disease Occurrence
- Epidemiological Approaches: Descriptive, Analytical and Experimental
- Principles of Control Measures and Levels of Prevention
- Investigation of an Epidemic of Communicable Disease
- Basic Epidemiological Tools for Community Diagnosis
- Effective Planning and Intervention Strategies
- Global Best Practices in Epidemiology
Introduction to Epidemiology in Community Health Nursing
Epidemiology is the scientific backbone of public health practice and community health nursing. It serves as the foundational discipline that studies the distribution and determinants of health-related states or events in specified populations, and the application of this study to control health problems.
For community health nurses, epidemiology provides the methodological framework and tools needed to make evidence-based decisions, design targeted interventions, and evaluate the effectiveness of public health programs.
Why Epidemiology Matters to Nurses
- Identifies at-risk populations that require targeted nursing interventions
- Guides resource allocation in community health programs
- Provides evidence for nursing practice and policy development
- Informs health education and promotion strategies
- Enables evaluation of intervention effectiveness
The Evolution of Epidemiology
-
Circa 400 B.C.
Hippocrates attempts to explain disease from a rational viewpoint rather than supernatural -
1854
John Snow’s cholera investigation establishes principles of modern epidemiology -
Early 20th Century
Focus on infectious disease control and vaccination campaigns -
Mid-20th Century
Expanded to include chronic disease, environmental factors, and behavioral influences -
21st Century
Integration of molecular biology, genetics, data science, and global health security
The Epidemiological Triad
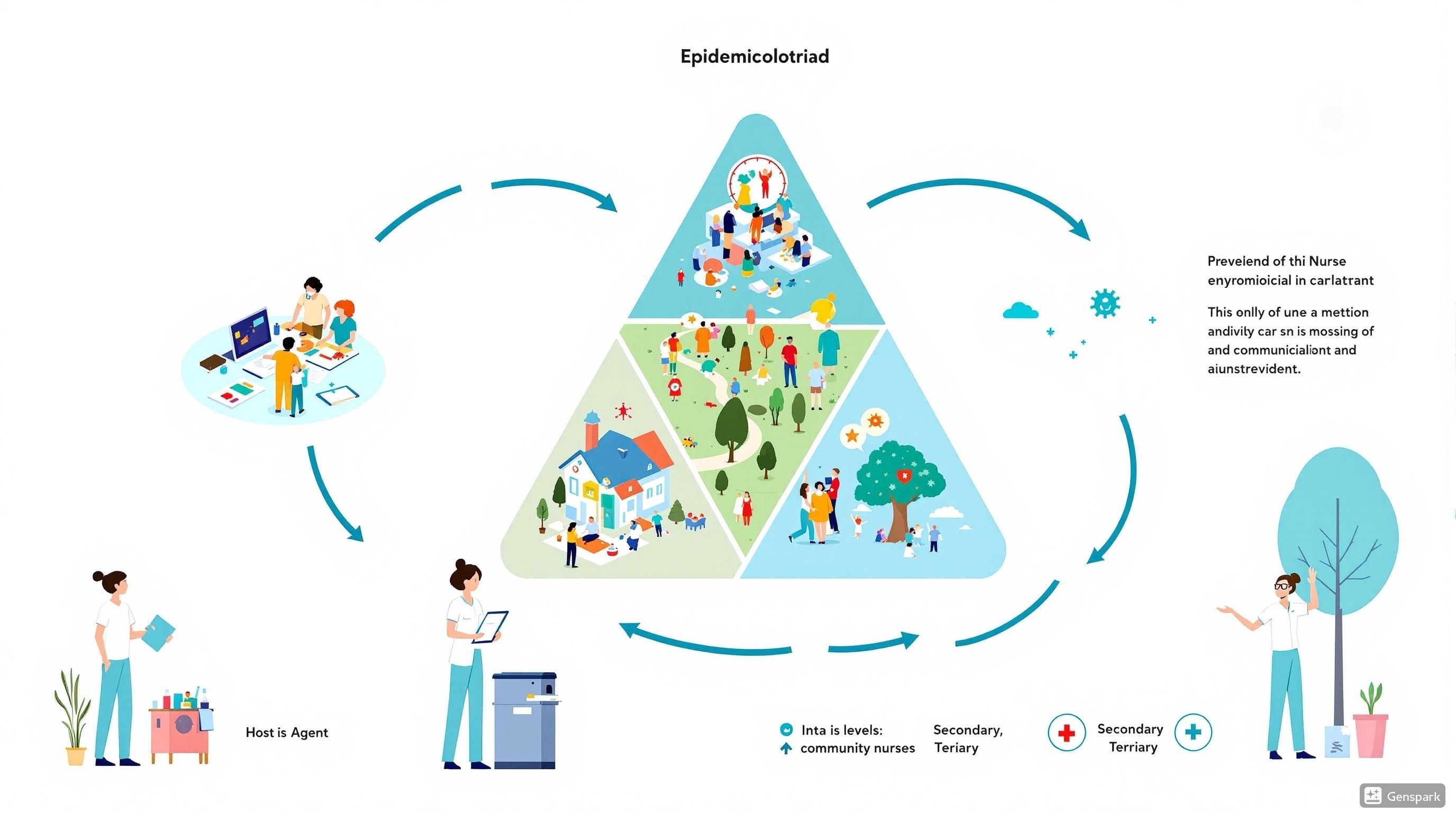
The epidemiological triad represents the three factors that influence disease occurrence:
- Agent: The causative factor that must be present for disease to occur (microbes, chemicals, physical forces)
- Host: The organism (usually human) that can get the disease
- Environment: External factors that influence agent and host interaction
Community health nurses work at all points of this triad to prevent disease and promote health through various levels of intervention.
Time Trends and Fluctuations in Disease Occurrence
Understanding how diseases occur and change over time helps community health nurses identify patterns, predict outbreaks, and develop appropriate preventive measures. Epidemiology provides the tools to analyze these temporal patterns and make informed decisions.
Types of Time Trends in Disease Occurrence
| Pattern | Description | Nursing Implications |
|---|---|---|
| Secular Trends | Long-term changes in disease occurrence over years or decades | Guide long-term health planning and policy development |
| Seasonal Variations | Cyclical patterns related to time of year | Prepare seasonal intervention strategies (e.g., flu vaccination campaigns) |
| Cyclical Patterns | Regular fluctuations over multi-year periods | Predict upcoming disease waves and prepare resources |
| Day-of-Week Effects | Variations based on day of the week | Optimize staffing and service availability |
| Diurnal Variations | Changes within a 24-hour period | Time interventions for maximum effectiveness |
Factors Influencing Disease Trends
- Pathogen Evolution: Changes in infectious agents
- Population Immunity: Herd immunity levels
- Demographic Changes: Aging populations, urbanization
- Human Mobility: Travel and migration patterns
- Climate and Weather: Seasonal factors, climate change
- Healthcare Interventions: Vaccination programs, treatments
- Socioeconomic Factors: Access to healthcare, living conditions
Mnemonic: “TIME TRENDS”
- T – Track data systematically
- I – Identify patterns (seasonal, cyclical)
- M – Measure baseline rates
- E – Evaluate contributing factors
- T – Test hypotheses about causes
- R – Recognize unusual clusters
- E – Examine historical context
- N – Note demographic variations
- D – Determine risk populations
- S – Share findings with stakeholders
Epidemic Patterns and Curves
Types of Epidemic Curves
- Point Source Epidemic: Single exposure, cases occur within one incubation period, sharp peak followed by rapid decline
- Continuous Common Source: Ongoing exposure source, plateaued epidemic curve
- Propagated Epidemic: Person-to-person transmission, multiple peaks separated by incubation periods
- Mixed Epidemic: Elements of both common source and propagated patterns
Interpreting Epidemic Curves
Epidemic curves help community health nurses to:
- Determine the type of outbreak and likely mode of transmission
- Estimate the time of exposure
- Predict the course of the outbreak
- Monitor the effectiveness of interventions
- Identify secondary waves of infection
Nursing Application: Using Time Trend Data
Community health nurses can use time trend data to:
- Plan staffing and resource allocation based on anticipated seasonal increases in disease
- Design and time health education campaigns before predicted disease peaks
- Implement preventive measures when environmental conditions favor disease spread
- Evaluate the impact of previous interventions by analyzing changes in trends
- Identify emerging health issues by recognizing unusual patterns or clusters
Epidemiological Approaches: Descriptive, Analytical and Experimental
Epidemiology employs three primary approaches to study disease occurrence and determinants. Each approach serves different purposes and uses specific methodologies to gather and analyze data. Community health nurses should understand these approaches to effectively interpret and apply epidemiological findings.
Descriptive Epidemiology
Purpose: To describe the distribution of health events by time, place, and person
Key Elements:
- Time: When did the disease occur?
- Place: Where did the disease occur?
- Person: Who was affected by the disease?
Methods:
- Case reports and case series
- Cross-sectional studies
- Ecological studies
- Surveillance data analysis
Analytical Epidemiology
Purpose: To examine associations between exposures and outcomes, test hypotheses about disease causation
Key Elements:
- Comparison groups
- Statistical measures of association
- Control of confounding factors
Methods:
- Case-control studies
- Cohort studies
- Cross-sectional analytical studies
- Ecological analytical studies
Experimental Epidemiology
Purpose: To evaluate interventions under controlled conditions
Key Elements:
- Researcher-controlled exposure
- Random allocation
- Control groups
- Outcome measurement
Methods:
- Randomized controlled trials
- Community trials
- Field trials
- Cluster randomized trials
Comparison of Epidemiological Approaches
| Feature | Descriptive | Analytical | Experimental |
|---|---|---|---|
| Main Question | What, who, where, when? | Why and how? | What works? |
| Study Design | Observational, no comparison groups | Observational with comparison groups | Controlled intervention |
| Evidence Strength | Low to moderate | Moderate to high | Highest |
| Timing | Often first approach | Follows descriptive | Often final step |
| Typical Use | Surveillance, hypothesis generation | Testing associations, risk factor identification | Evaluation of interventions |
| Nursing Application | Community assessment | Program planning, targeting high-risk groups | Evaluating nursing interventions |
Mnemonic: “D-A-E Approach”
Describe the pattern
Who, what, where, when?
Analyze the associations
Why and how?
Experiment with solutions
What works?
Application in Community Health Nursing
Community health nurses integrate all three epidemiological approaches in their practice:
- Descriptive Epidemiology: When conducting community assessments, identifying vulnerable populations, and participating in disease surveillance
- Analytical Epidemiology: When planning targeted interventions, allocating resources based on risk factors, and developing prevention strategies
- Experimental Epidemiology: When implementing and evaluating health promotion programs, educational interventions, and community-based initiatives
By understanding these approaches, nurses can better interpret epidemiological data and translate research findings into effective community health nursing practice.
Principles of Control Measures and Levels of Prevention
Prevention and control measures are central to epidemiology and community health nursing practice. These measures aim to reduce or eliminate factors contributing to health problems. Understanding the principles of control measures and the different levels of prevention is essential for effective community health interventions.
Control Measures: Breaking the Chain of Infection
Control measures target specific elements in the chain of infection to prevent or limit disease spread:
| Link in Chain | Control Measures | Examples |
|---|---|---|
| Infectious Agent | Elimination or reduction of the disease-causing pathogen | Antibiotic treatment, sanitization, sterilization |
| Reservoir | Identification and management of disease sources | Treatment of carriers, vector control, water treatment |
| Portal of Exit | Blocking the pathogen’s exit from the reservoir | Covering mouth when coughing, proper wound dressing, isolation |
| Mode of Transmission | Interrupting disease spread pathways | Hand hygiene, food safety practices, environmental controls |
| Portal of Entry | Protecting vulnerable entry points | Masks, gloves, protective eyewear, mosquito nets |
| Susceptible Host | Increasing resistance to infection | Immunization, prophylactic medications, nutrition support |
Primary Prevention
Goal: Prevent disease onset or injury occurrence
Target: Healthy individuals and communities
Timing: Before disease or injury occurs
Strategies:
- Immunization programs
- Health education
- Environmental sanitation
- Nutrition programs
- Safety regulations
- Vector control
Example: Community-wide vaccination campaigns to prevent measles outbreaks
Secondary Prevention
Goal: Early detection and prompt intervention
Target: Individuals with risk factors or in early disease stages
Timing: After disease begins but before symptoms appear
Strategies:
- Screening programs
- Case finding activities
- Periodic health examinations
- Prompt diagnosis and treatment
- Contact tracing
- Risk assessment
Example: Blood pressure screening followed by early treatment to prevent stroke
Tertiary Prevention
Goal: Limit disability and restore function
Target: Individuals with established disease
Timing: After disease or injury has occurred
Strategies:
- Rehabilitation programs
- Support groups
- Disease management
- Disability limitation
- Vocational training
- Long-term care
Example: Cardiac rehabilitation program for heart attack survivors
Mnemonic: “PREVENT”
To remember key principles of prevention in epidemiology:
- P – Primary targets healthy individuals
- R – Risk factors addressed at all levels
- E – Early intervention is crucial
- V – Various strategies for different populations
- E – Education essential at every level
- N – Nursing interventions span all levels
- T – Timing determines the level of prevention
Primordial Prevention: The Foundational Level
Some epidemiologists recognize primordial prevention as a distinct level that precedes primary prevention:
Goal: Prevent the emergence of risk factors in populations
Target: Social, economic, environmental conditions
Timing: Before risk factors develop
Strategies:
- Public policy development
- Community planning
- Environmental protection
- Poverty reduction strategies
- Urban design for healthy living
Case Example:
A community health nurse participates in urban planning to ensure neighborhoods have safe walking paths, parks, and access to healthy food options. This primordial prevention approach aims to prevent the development of obesity risk factors in the community before they emerge.
By addressing the fundamental social and environmental conditions, primordial prevention creates living conditions that promote health and make unhealthy behaviors less likely.
Nursing Application: Implementing Prevention Levels
Community health nurses play crucial roles in implementing all levels of prevention:
- Primary Prevention: Conducting health education sessions, organizing vaccination drives, promoting healthy lifestyles
- Secondary Prevention: Performing screenings, referring for diagnostic tests, conducting home visits for early detection
- Tertiary Prevention: Managing chronic diseases, coordinating rehabilitation services, providing supportive care
Effective community health nursing practice involves working at multiple prevention levels simultaneously, often tailoring approaches to meet the specific needs of different population groups within the community.
Investigation of an Epidemic of Communicable Disease
Investigating epidemics is a core function of applied epidemiology. The systematic investigation of disease outbreaks helps identify the source, mode of transmission, and population at risk, guiding the implementation of control measures. Community health nurses often participate in these investigations as part of interdisciplinary teams.
Steps in Epidemic Investigation
Prepare for fieldwork
Establish existence of outbreak
Verify diagnosis
Create case definition
Find cases systematically
Perform descriptive epidemiology
Develop hypotheses
Evaluate hypotheses
Refine hypotheses
Compare with lab findings
Implement control measures
Communicate findings
Key Components of Outbreak Investigation
1. Case Definition
A standardized set of criteria for classifying whether a person has a particular disease or health condition. Includes:
- Clinical criteria (symptoms, signs, test results)
- Time criteria (timeframe)
- Place criteria (geographic location)
- Person criteria (demographic characteristics)
2. Case Classification
- Confirmed: Meets all clinical and laboratory criteria
- Probable: Meets most criteria, laboratory unconfirmed
- Possible/Suspected: Some symptoms present, requires further investigation
3. Data Collection Tools
- Line listings (systematic case records)
- Questionnaires and interview forms
- Medical record abstraction forms
- Laboratory specimen collection protocols
- Environmental assessment checklists
Analytical Techniques in Outbreak Investigation
1. Descriptive Analysis
- Time: Epidemic curves showing case distribution over time
- Place: Spot maps showing geographic distribution
- Person: Demographic and clinical characteristics of cases
2. Analytical Studies
- Cohort Studies: Used when population is well-defined (e.g., outbreak in a nursing home)
- Case-Control Studies: Used when population is not clearly defined
3. Statistical Measures
- Attack rates (overall and group-specific)
- Relative risk or odds ratio
- Confidence intervals
- P-values for hypothesis testing
Attack Rate Formula:
Attack Rate = (Number of cases / Population at risk) × 100
Mnemonic: “OUTBREAK”
Observe the pattern
Understand the diagnosis
Track all cases
Build a case definition
Review time, place, person
Evaluate hypotheses
Apply control measures
Keep communicating findings
Types of Epidemics and Investigation Approaches
| Type of Epidemic | Characteristics | Investigation Focus |
|---|---|---|
| Point Source | Single exposure source, cases occur within one incubation period | Identify the common source (e.g., food, water) |
| Continuous Common Source | Ongoing exposure source, cases continue over longer period | Find and eliminate the persistent source |
| Propagated | Person-to-person spread, multiple incubation period waves | Break chains of transmission, isolate cases |
| Mixed | Initial common source followed by person-to-person spread | Eliminate source and prevent secondary spread |
| Pseudo-Epidemic | Apparent increase due to changes in reporting, detection, or diagnosis | Distinguish artificial from true increase in cases |
Nursing Role in Outbreak Investigation
Community health nurses play vital roles in outbreak investigations:
- Case Finding: Identifying and interviewing potential cases
- Data Collection: Gathering clinical and exposure information
- Specimen Collection: Obtaining appropriate samples for laboratory testing
- Contact Tracing: Identifying and following up with exposed individuals
- Implementation of Control Measures: Isolation, quarantine, vaccination, prophylaxis
- Health Education: Providing information to affected communities
- Surveillance: Monitoring for additional cases
The community health nurse’s combination of clinical knowledge, communication skills, and community trust makes them essential members of outbreak investigation teams.
Basic Epidemiological Tools for Community Diagnosis
Epidemiology provides community health nurses with essential tools to assess, diagnose, and address health problems at the population level. These tools help in understanding the health status of communities, identifying priorities, and planning effective interventions.
Core Epidemiological Tools
1. Descriptive Tools
- Surveys and Surveillance Systems: Collect data on disease incidence and prevalence
- Epidemiological Maps: Show geographic distribution of health events and identify clusters
- Graphs and Tables: Visualize trends over time and compare different population subgroups
2. Analytical Tools
- Case-Control Studies: Compare individuals with disease to those without to identify risk factors
- Cohort Studies: Follow groups over time to see who develops disease
- Cross-Sectional Studies: Examine data at a single point in time to find associations
- Statistical Analysis Software: Analyze data to determine relationships between exposures and outcomes
3. Screening and Diagnostic Tools
- Laboratory Testing: Confirm diagnosis and identify causative agents
- Sensitivity and Specificity Tests: Evaluate performance of screening methods
- Predictive Values: Determine accuracy of positive or negative test results
4. Outbreak Investigation Tools
- Epidemic Curves: Visualize onset and spread of cases over time
- Line Lists: Detailed case data to identify common exposures
- Hypothesis Generation and Testing: Develop and test theories about disease sources and spread
Community Health Assessment Tools
- Community Surveys: Collect data on health behaviors, access to care, and other factors affecting health
- Focus Groups and Interviews: Gain in-depth insights from community members about health needs and concerns
- Health Indicators: Standardized measures to assess community health status (e.g., mortality rates, morbidity statistics)
Risk Assessment and Communication Tools
- Quantitative Risk Assessment: Estimate the magnitude of health risks in numerical terms
- Qualitative Risk Assessment: Assess perceptions and concerns about health risks
- Risk Communication Plans: Develop strategies to inform communities about health risks and prevention measures
Emerging Tools:
- Geographic Information Systems (GIS)
- Mobile health technologies
- Big data analytics
- Molecular epidemiology tools
- Predictive modeling software
- Social network analysis
Key Measures in Epidemiology for Community Diagnosis
| Measure | Definition | Formula | Use in Community Diagnosis |
|---|---|---|---|
| Incidence Rate | Rate of new cases in a population over a specified period | (New cases / Population at risk) × 10n | Measures disease occurrence, evaluates effectiveness of preventive measures |
| Prevalence | Proportion of population with disease at a specific point in time | (All cases / Total population) × 10n | Assesses disease burden, plans health services and resources |
| Mortality Rate | Rate of death in a population | (Number of deaths / Total population) × 10n | Evaluates community health status, identifies priority health issues |
| Case Fatality Rate | Proportion of cases resulting in death | (Deaths from disease / Total cases of disease) × 100 | Measures disease severity, evaluates treatment effectiveness |
| Attack Rate | Cumulative incidence in a defined population during an outbreak | (Number affected / Total population at risk) × 100 | Investigates outbreaks, identifies risk factors |
| Relative Risk | Ratio of risk in exposed group to risk in unexposed group | Risk in exposed / Risk in unexposed | Identifies associations between exposures and outcomes |
| Odds Ratio | Ratio of odds of exposure in cases to odds of exposure in controls | (a/c) / (b/d) or (a×d) / (b×c) | Measures association strength in case-control studies |
Mnemonic: “COMMUNITY”
Remember essential epidemiological tools for community diagnosis:
- C – Collect data systematically (surveys, surveillance)
- O – Observe patterns (time, place, person analysis)
- M – Measure rates accurately (incidence, prevalence)
- M – Map the distribution (GIS, spot maps)
- U – Understand associations (analytical studies)
- N – Note trends over time (time series analysis)
- I – Investigate clusters (outbreak investigation)
- T – Test hypotheses (statistical analysis)
- Y – Yield recommendations (evidence-based interventions)
Steps in Community Diagnosis Using Epidemiological Tools
- Community Assessment: Collect demographic, socioeconomic, and health data
- Data Analysis: Calculate rates and measures, identify patterns and trends
- Problem Identification: Determine priority health issues based on magnitude, severity, and preventability
- Causal Analysis: Identify factors contributing to health problems
- Resource Assessment: Evaluate available resources and assets in the community
- Intervention Planning: Develop strategies based on evidence and community input
- Implementation: Execute planned interventions with community partners
- Evaluation: Measure outcomes and impact using epidemiological methods
Practical Application: Using Epidemiological Tools in Community Health Nursing
Case Finding and Screening
Use prevalence data to determine high-risk populations for targeted screening programs. Evaluate screening effectiveness using sensitivity, specificity, and predictive value calculations.
Program Planning
Identify priority health issues using comparative rates and trends. Design interventions based on risk factor analysis and evidence from analytical studies.
Resource Allocation
Direct resources to areas with highest need based on disease burden measures. Use cost-effectiveness data to maximize impact with available resources.
By effectively using epidemiological tools, community health nurses can move beyond intuition and anecdotal evidence to make data-driven decisions that improve population health outcomes.
Effective Planning and Intervention Strategies
After using epidemiological tools for community diagnosis, the next step is translating findings into effective plans and interventions. Community health nurses play a crucial role in this process, applying epidemiologic insights to design, implement, and evaluate health programs.
Evidence-Based Planning Process
- Define the Health Issue: Use epidemiological data to clearly define the scope and characteristics of the health problem
- Set Priorities: Rank health issues based on:
- Magnitude (how many affected)
- Severity (health impact)
- Preventability
- Community concern
- Resource availability
- Set SMART Objectives: Develop specific, measurable, achievable, relevant, and time-bound objectives
- Identify Target Population: Use epidemiological data to define at-risk groups for intervention
- Select Evidence-Based Strategies: Choose interventions with proven effectiveness for the identified problem
- Develop Action Plan: Detail specific activities, timeline, responsibilities, and resources
- Implement Plan: Execute activities with quality control measures
- Evaluate Outcomes: Use epidemiological methods to measure impact
Types of Intervention Strategies
| Strategy Type | Examples | Epidemiological Basis |
|---|---|---|
| Environmental | Vector control, water treatment, air quality improvements | Environmental risk factors identified in analytical studies |
| Educational | Health education campaigns, counseling, skill development | Knowledge gaps and behavioral risk factors identified in surveys |
| Policy/Regulatory | Health policies, regulations, guidelines | Population-level risk factors requiring systematic change |
| Clinical/Service | Screening programs, immunization campaigns, treatment services | Disease prevalence and risk factor distribution |
| Community Mobilization | Community coalitions, participatory approaches | Social determinants identified through community assessment |
Evaluation Framework
Epidemiological methods provide the foundation for evaluating interventions:
- Process Evaluation: Measures implementation fidelity and reach
- Impact Evaluation: Assesses short-term outcomes and immediate effects
- Outcome Evaluation: Determines long-term health changes and program effectiveness
Key Evaluation Indicators:
- Changes in disease incidence or prevalence
- Shifts in risk factor distribution
- Improvements in health behaviors
- Enhanced knowledge and attitudes
- Population health outcomes
Levels of Intervention Planning
Individual Level
Target: Personal behaviors, knowledge, skills
Examples: Health education, counseling, screening
Epidemiological Base: Risk factors at individual level
Community Level
Target: Community norms, resources, environment
Examples: Community campaigns, coalition building
Epidemiological Base: Community-level risk patterns
System Level
Target: Policies, systems, environments
Examples: Policy advocacy, infrastructure changes
Epidemiological Base: Structural determinants of health
Mnemonic: “EPIDPLAN”
A framework for using epidemiology in planning community health interventions:
- E – Examine the data (identify patterns and trends)
- P – Prioritize health issues (based on magnitude and severity)
- I – Identify target populations (most affected or at highest risk)
- D – Determine modifiable risk factors (from analytical studies)
- P – Plan evidence-based interventions (addressing identified factors)
- L – Link resources to needs (based on community assets)
- A – Activate implementation strategies (with stakeholder involvement)
- N – Note outcomes with evaluation (using epidemiological measures)
Case Study: From Epidemiological Data to Community Intervention
Community Diagnosis
Epidemiological data showed increasing rates of type 2 diabetes in a suburban community, with highest prevalence in low-income neighborhoods with limited access to healthy foods and physical activity opportunities.
Planning Process
Community health nurses worked with stakeholders to develop a multi-level intervention targeting modifiable risk factors identified through analytical epidemiology: diet, physical activity, and health education.
Implementation
Interventions included establishing community gardens, advocating for grocery store development, creating walking groups, and implementing diabetes prevention education programs at community centers.
Evaluation
Epidemiological methods were used to measure changes in diabetes incidence, risk behaviors, and health outcomes over time, documenting a 15% reduction in new diabetes cases after three years.
This case demonstrates how community health nurses can use epidemiological tools at every stage of the intervention process, from initial diagnosis to final evaluation, creating a continuous cycle of assessment, planning, implementation, and evaluation.
Global Best Practices in Epidemiology
Global best practices in epidemiology showcase innovative and effective approaches to addressing public health challenges. These examples provide valuable insights for community health nurses seeking to enhance their practice and improve health outcomes in their communities.
Participatory Epidemiology
Country Example: Kenya
Participatory epidemiology involves community members in the collection and interpretation of epidemiological data, combining scientific methods with local knowledge.
Key Features:
- Community involvement in all research phases
- Integration of traditional knowledge with scientific methods
- Use of accessible data collection tools
- Community ownership of findings
- Action-oriented approach
In Kenya, this approach has been successfully used for disease surveillance in remote communities, with community health workers trained to recognize and report unusual health events.
Digital Epidemiology
Country Example: Singapore
Digital epidemiology leverages technology and big data to enhance disease surveillance, outbreak detection, and response.
Key Features:
- Real-time data collection and analysis
- Use of mobile applications for reporting
- Integration of multiple data sources
- Predictive modeling and forecasting
- Rapid response capabilities
Singapore implemented a comprehensive digital epidemiology system for COVID-19, including contact tracing apps, digital check-ins, and centralized data analysis, enabling quick identification and containment of cases.
One Health Approach
Country Example: Thailand
The One Health approach recognizes that human health is connected to animal health and environmental health, integrating these disciplines in epidemiological work.
Key Features:
- Interdisciplinary collaboration
- Surveillance across human, animal, and environmental sectors
- Joint outbreak investigations
- Integrated data systems
- Coordinated interventions
Thailand’s One Health network brings together human health, veterinary, and environmental professionals to address zoonotic diseases like avian influenza, resulting in improved early detection and control.
Innovative Surveillance Systems
Syndromic Surveillance – United Kingdom
The UK’s syndromic surveillance system monitors patterns of symptoms before laboratory confirmation, enabling early outbreak detection.
Key Innovation: Integration of data from emergency departments, primary care, and telephone health helplines to detect unusual health patterns in real-time.
Community-Based Surveillance – Rwanda
Rwanda’s community-based surveillance system engages community health workers to report priority diseases from villages.
Key Innovation: Use of mobile phones for real-time reporting from remote areas, combined with regular feedback loops and training for community health workers.
Epidemiological Approaches to Non-Communicable Diseases
STEPwise Approach – Finland
Finland’s application of the WHO’s STEPwise approach has been successful in reducing cardiovascular disease through population-wide interventions.
Key Elements:
- Standardized data collection on risk factors
- Community-wide policy interventions
- Food industry partnerships
- Regular monitoring and evaluation
- Multi-sector collaboration
Risk Factor Surveillance – Brazil
Brazil’s telephone-based surveillance system for non-communicable disease risk factors provides timely data for intervention planning.
Key Elements:
- Cost-effective data collection method
- Regular, standardized monitoring
- Rapid data processing and feedback
- Direct link to policy development
- Adaptable to local contexts
Applications for Community Health Nursing Practice
Community health nurses can apply these global best practices in their local settings:
- Adapt Participatory Methods: Engage community members in identifying health priorities, collecting data, and developing culturally appropriate interventions
- Leverage Digital Tools: Utilize mobile applications, social media, and electronic health records to enhance surveillance and health communication
- Adopt One Health Thinking: Consider environmental and animal health factors when investigating disease patterns in the community
- Implement Syndromic Surveillance: Monitor patterns of symptoms in community settings to detect potential outbreaks early
- Focus on Risk Factor Surveillance: Regularly assess modifiable risk factors for non-communicable diseases to guide prevention efforts
By incorporating these global innovations while respecting local contexts and needs, community health nurses can enhance the effectiveness of epidemiological approaches in their practice.
Conclusion
Epidemiology serves as the cornerstone of community health nursing practice, providing the scientific foundation for understanding, preventing, and controlling health problems at the population level. Through the systematic application of epidemiological approaches, tools, and principles, community health nurses can:
- Analyze time trends and patterns in disease occurrence to anticipate health problems
- Apply descriptive, analytical, and experimental approaches to understand health issues comprehensively
- Implement control measures and prevention strategies at primary, secondary, and tertiary levels
- Systematically investigate outbreaks using established epidemiological methods
- Utilize epidemiological tools to make accurate community diagnoses
- Develop evidence-based plans and interventions that address community health needs
- Learn from global best practices and adapt them to local contexts
As healthcare continues to evolve, the role of epidemiology in community health nursing becomes increasingly important. By mastering epidemiological concepts and skills, community health nurses position themselves as essential members of public health teams, capable of leading efforts to improve population health outcomes.
The integration of traditional epidemiological methods with new technologies, participatory approaches, and interdisciplinary collaboration offers exciting opportunities for community health nurses to enhance their practice and make meaningful contributions to public health.
References
- Centers for Disease Control and Prevention. (2006). Principles of epidemiology in public health practice: An introduction to applied epidemiology and biostatistics (3rd ed.). U.S. Department of Health and Human Services.
- World Health Organization. (2020). Basic epidemiology (3rd ed.). WHO Press.
- Friis, R.H., & Sellers, T.A. (2020). Epidemiology for public health practice (6th ed.). Jones & Bartlett Learning.
- Whitehouse, E.R., & Mase, W.A. (2019). Epidemiology and nursing practice. In C.L. Savage (Ed.), Public/community health and nursing practice: Caring for populations (pp. 55-78). F.A. Davis.
- Pazzaglia, C., Camedda, C., Ugenti, N.V., Trentin, A., et al. (2023). Community health assessment tools adoptable in nursing practice: A scoping review. International Journal of Environmental Research and Public Health, 20(3), 1667.
- Yongu, W.T. (2021). A critical review of levels of disease development and prevention in epidemiology. International Journal of Human Kinetics, Health and Education.
- AbdulRaheem, Y. (2023). Unveiling the significance and challenges of integrating prevention levels in healthcare practice. Journal of Primary Care & Community Health.
- Sistrom, M.G., & Hale, P.J. (2006). Outbreak investigations: Community participation and role of community and public health nurses. Public Health Nursing, 23(3), 256-263.
- Fayram, E.S., & Anderko, L. (2009). Applied epidemiology for public health and community-based nurses. The Journal of Continuing Education in Nursing, 40(8), 361-366.
- White, F. (2020). Application of disease etiology and natural history to prevention in primary health care: A discourse. Medical Principles and Practice, 29(6), 501-513.
