Filariasis: Comprehensive Nursing Notes
A Community Health Nursing Perspective
Table of Contents
Introduction to Filariasis
Filariasis is a parasitic disease caused by thread-like filarial worms that live in the human lymphatic system or subcutaneous tissues. These parasites are transmitted to humans through the bites of infected mosquitoes. Lymphatic filariasis, caused primarily by Wuchereria bancrofti, Brugia malayi, and Brugia timori, is the most common form of filariasis and a leading cause of permanent disability worldwide.
As community health nurses, understanding filariasis is crucial for implementing effective prevention strategies, early detection, and managing affected individuals within communities. This comprehensive guide focuses on the epidemiology, prevention, screening, diagnosis, and management of filariasis from a community health nursing perspective.
Key Fact: Lymphatic filariasis affects more than 120 million people in 72 countries throughout the tropics and sub-tropics of Asia, Africa, the Western Pacific, and parts of the Caribbean and South America.
Epidemiology of Filariasis
Filariasis remains a significant public health challenge in tropical and subtropical regions. Understanding its epidemiology is essential for developing targeted community interventions.
Global Distribution
Lymphatic filariasis is endemic in 72 countries across:
- Sub-Saharan Africa (35 countries)
- Southeast Asia (including India, Bangladesh, Indonesia)
- Western Pacific regions
- Parts of South America and the Caribbean
Prevalence and Incidence
The World Health Organization (WHO) estimates that:
- Approximately 120 million people are currently infected with filariasis
- About 40 million people suffer from the stigmatizing and disabling clinical manifestations
- Nearly 1.4 billion people in 73 countries are at risk of infection
Risk Factors
| Category | Risk Factors |
|---|---|
| Environmental |
|
| Demographic |
|
| Social |
|
| Biological |
|
Transmission Dynamics
Filariasis is transmitted by various mosquito species that serve as vectors:
- Culex quinquefasciatus (most common vector in urban and semi-urban areas)
- Anopheles species (in rural areas of Africa and elsewhere)
- Aedes species (in Pacific islands)
- Mansonia species (in rural areas of Southeast Asia)
Community Health Impact: Filariasis not only affects individual health but also has significant socioeconomic impacts on communities. Disability from chronic filariasis reduces productivity, increases healthcare costs, and often leads to social stigma and isolation.
Pathophysiology and Life Cycle
Understanding the life cycle of filarial parasites is essential for comprehending the disease progression and implementing effective prevention strategies.
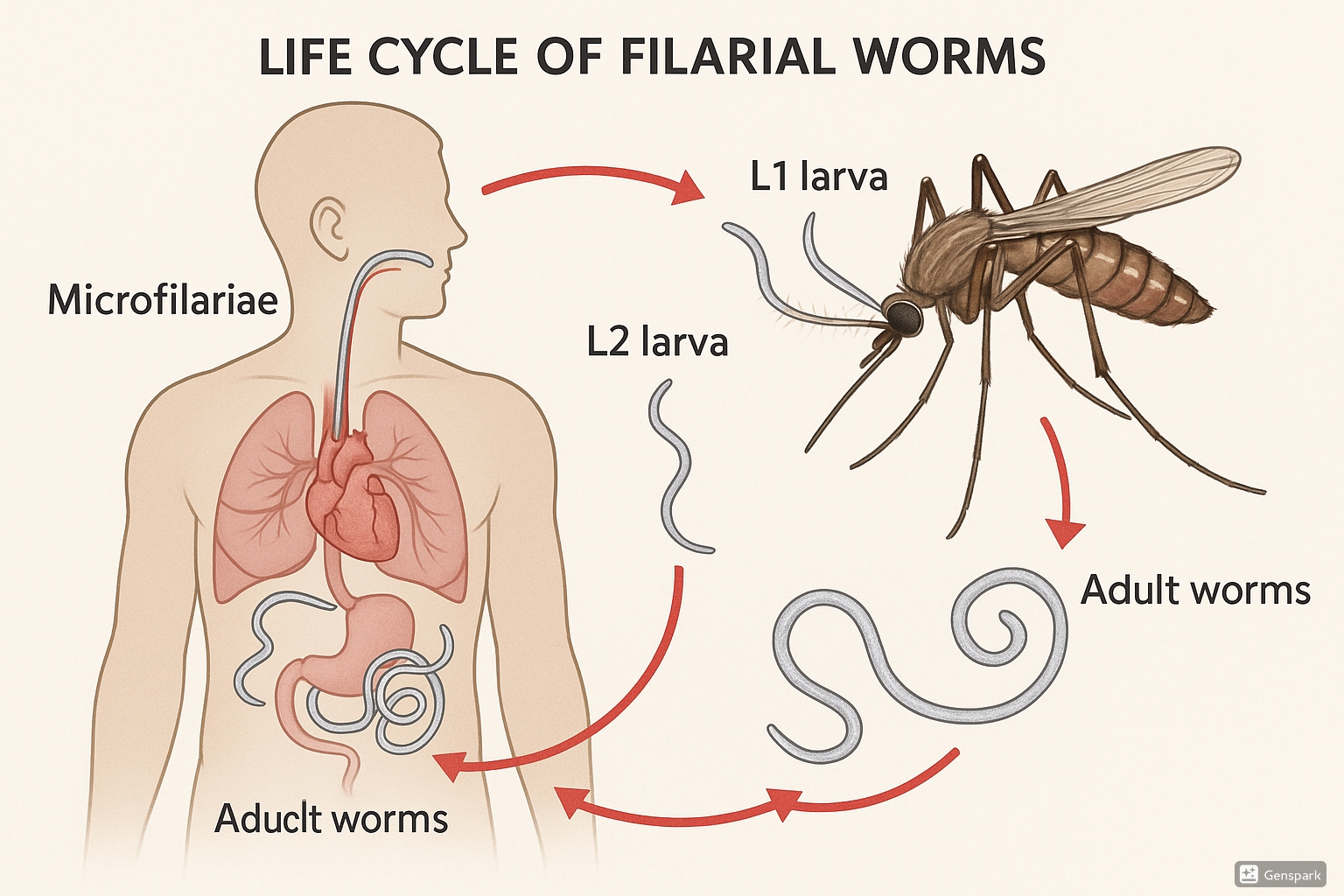
Life Cycle of Filariasis
- Transmission: Infected female mosquitoes deposit infective larvae (L3) onto human skin during a blood meal
- Entry and Migration: Larvae enter through the bite wound and migrate to lymphatic vessels
- Maturation: Over 6-12 months, larvae develop into adult worms in lymphatic vessels
- Reproduction: Adult female worms produce thousands of microfilariae that circulate in the bloodstream, typically with nocturnal periodicity
- Vector Uptake: Microfilariae are ingested by mosquitoes during blood meals
- Development in Vector: Inside the mosquito, microfilariae develop into infective larvae over 10-14 days
- Transmission: The cycle continues when infected mosquitoes bite humans
Pathophysiological Changes
The disease progression involves several mechanisms:
- Early phase: Asymptomatic microfilaremia with minimal pathological changes
- Acute phase: Inflammatory responses to adult worms and their antigens
- Chronic phase: Lymphatic damage from dead worms, resulting in:
- Lymphatic vessel dilation
- Valve dysfunction
- Lymph stasis
- Fibrosis of lymphatic channels
- Advanced stage: Secondary bacterial and fungal infections exacerbate lymphedema, leading to elephantiasis
Mnemonic: “FILARIAL” Pathophysiology
- F – Filarial worms invade lymphatics
- I – Inflammation triggered by adult worms
- L – Lymphatic vessel damage occurs
- A – Adult worm death causes greater inflammation
- R – Resulting lymphatic obstruction
- I – Impaired lymph flow leads to edema
- A – Accumulation of fluid in tissues
- L – Lasting fibrosis and irreversible changes
Clinical Manifestations
Filariasis presents with a spectrum of clinical manifestations, from asymptomatic infection to severe disfigurement. Recognizing these manifestations is crucial for early detection and intervention.
Stages of Lymphatic Filariasis
| Stage | Clinical Features | Nursing Considerations |
|---|---|---|
| Asymptomatic Microfilaremia |
|
|
| Acute Manifestations |
|
|
| Chronic Manifestations |
|
|
| Tropical Pulmonary Eosinophilia (TPE) |
|
|
Grading of Lymphedema
The WHO classification for lymphedema severity in filariasis:
- Grade I: Pitting edema that is reversible overnight
- Grade II: Non-pitting edema that doesn’t reverse overnight
- Grade III: Non-pitting edema with skin thickening
- Grade IV: Non-pitting edema with fibrotic changes and warty excrescences (elephantiasis)
Clinical Alert for Nurses
Acute episodes of adenolymphangitis (ADL) are often triggered by secondary bacterial infections in patients with chronic lymphedema. These episodes are characterized by high fever, chills, and increased swelling of affected areas. Immediate treatment with antibiotics and anti-inflammatory agents is essential to prevent progression of lymphedema.
Prevention and Control Measures
Prevention of filariasis focuses on breaking the transmission cycle through vector control, mass drug administration, and hygiene education. Community health nurses play a pivotal role in implementing these preventive strategies.
Primary Prevention Strategies
1. Vector Control
- Environmental management:
- Elimination of mosquito breeding sites (draining stagnant water)
- Improved sanitation and waste management
- Covering water storage containers
- Chemical control:
- Indoor residual spraying (IRS)
- Larvicides in breeding sites
- Space spraying during epidemics
- Biological control:
- Introduction of larvivorous fish
- Bacterial agents (Bacillus thuringiensis)
2. Personal Protection
- Use of insecticide-treated bed nets (ITNs)
- Window and door screens
- Wearing long-sleeved clothes, especially during peak biting hours
- Application of insect repellents
3. Mass Drug Administration (MDA)
Annual administration of antifilarial drugs to entire at-risk populations:
- Regimen in most areas: Diethylcarbamazine (DEC) + Albendazole
- In areas with onchocerciasis: Ivermectin + Albendazole
- Triple therapy (IDA): Ivermectin + DEC + Albendazole in certain regions
- Minimum 5 annual rounds with >65% population coverage is recommended
Secondary Prevention Strategies
These focus on preventing disability in already infected individuals:
- Morbidity management and disability prevention (MMDP)
- Hygiene measures for affected limbs
- Compression therapy and exercises to reduce lymphedema
- Prompt treatment of secondary infections
Role of Community Health Nurses in Prevention
| Prevention Level | Nursing Activities |
|---|---|
| Community Education |
|
| MDA Implementation |
|
| Vector Control |
|
| Patient Care |
|
Mnemonic: “PREVENT FILARIASIS”
- P – Protect with bed nets and screens
- R – Remove standing water sources
- E – Educate communities about transmission
- V – Vector control through multiple approaches
- E – Ensure proper sanitation
- N – Nighttime protection (when vectors are most active)
- T – Treatment through mass drug administration
- F – Follow-up with affected individuals
- I – Improve housing conditions
- L – Limb hygiene for those with lymphedema
- A – Advocacy for community resources
- R – Regular surveillance of cases
- I – Integrate prevention into primary healthcare
- A – Address misconceptions about the disease
- S – Support affected individuals
- I – Implement WHO guidelines
- S – Sustain prevention efforts
Screening and Diagnosis
Early detection of filariasis through systematic screening is essential for timely intervention and preventing chronic complications. Community health nurses must be familiar with various screening and diagnostic methods.
Screening Approaches
- Mass screening: Conducted in endemic areas as part of elimination programs
- Targeted screening: Focusing on high-risk populations or symptomatic individuals
- Passive detection: Based on clinical presentations at healthcare facilities
- Active surveillance: Systematic screening in communities by health workers
Diagnostic Methods
| Diagnostic Method | Description | Nursing Considerations |
|---|---|---|
| Microscopic Examination |
|
|
| Immunochromatographic Test (ICT) |
|
|
| ELISA Tests |
|
|
| Polymerase Chain Reaction (PCR) |
|
|
| Ultrasonography |
|
|
Clinical Assessment
In resource-limited settings, clinical assessment remains valuable:
- History taking:
- Residence in endemic areas
- Episodes of fever with lymphangitis
- Progressive swelling of extremities
- Family history of similar conditions
- Physical examination:
- Inspection for lymphedema and its grading
- Assessment for hydrocele in males
- Examination of skin for thickening, folds, or lesions
- Palpation of lymph nodes
Nursing Protocol: Community Screening for Filariasis
- Prepare screening materials (ICT cards, gloves, alcohol swabs, lancets)
- Educate community about screening purpose and procedure
- Obtain informed consent from participants
- Collect demographic information and relevant history
- Perform rapid diagnostic test according to protocol
- Record results systematically
- Provide appropriate counseling based on results
- Refer positive cases for confirmation and treatment
- Ensure follow-up mechanism is in place
- Compile and report screening data to health authorities
Primary Management
Management of filariasis aims to eliminate the parasite, prevent transmission, and manage chronic complications. Community health nurses play a crucial role in both acute and chronic disease management.
Pharmacological Management
| Medication | Dosage and Administration | Nursing Considerations |
|---|---|---|
| Diethylcarbamazine (DEC) |
|
|
| Albendazole |
|
|
| Ivermectin |
|
|
| Doxycycline |
|
|
Supportive Management for Acute Episodes
- Antipyretics for fever (acetaminophen, ibuprofen)
- Analgesics for pain relief
- Antibiotics for secondary bacterial infections
- Anti-inflammatory drugs to reduce lymphangitis
- Rest and elevation of affected limbs
- Cool compresses for local relief
Management of Chronic Manifestations
Lymphedema Management
The WHO-recommended basic lymphedema management package includes:
- Hygiene: Daily washing of affected limbs with soap and clean water
- Skin care: Application of moisturizers to prevent cracks
- Elevation: Raising affected limbs when resting or sleeping
- Exercise: Regular movement to promote lymph flow
- Compression: Using bandages or compression garments
- Wound care: Prompt treatment of entry lesions
- Fungal infection prevention: Keeping interdigital spaces dry
Hydrocele Management
- Surgical intervention (hydrocelectomy) for large or symptomatic hydroceles
- Pre-operative assessment and counseling
- Post-operative care and follow-up
Nursing Intervention: Teaching Lymphedema Self-Care
- Limb Washing: Demonstrate proper washing technique using mild soap and clean water
- Drying: Emphasize thorough but gentle drying, especially between digits
- Moisturizing: Show application of non-irritating moisturizer
- Elevation: Teach proper positioning during rest and sleep
- Exercise: Demonstrate simple exercises to promote lymph flow
- Inspection: Train in daily self-examination for cuts, cracks, or infections
- Compression: If appropriate, teach proper application of bandages or garments
- Warning Signs: Educate on signs of acute infection requiring medical attention
Referral Criteria
Community health nurses must recognize situations requiring referral to higher levels of care. Timely referrals can prevent complications and improve outcomes.
Indications for Immediate Referral
- Severe adverse reactions to antifilarial medications
- Acute dermatolymphangioadenitis (ADL) with high fever and systemic symptoms
- Signs of sepsis (altered mental status, hypotension, tachycardia)
- Cellulitis unresponsive to first-line antibiotics
- Lymphedema with ulceration or deep tissue infection
- Chyluria (milky urine) indicating lymphatic damage to urinary system
- Tropical pulmonary eosinophilia with respiratory distress
Indications for Elective Referral
- Progressive lymphedema despite basic management
- Large or symptomatic hydrocele requiring surgical evaluation
- Recurrent episodes of ADL despite preventive measures
- Diagnostic uncertainty requiring specialized testing
- Psychological distress related to disfigurement
- Complications affecting quality of life or functional capacity
Referral Protocol for Community Health Nurses
- Assess patient using standardized criteria
- Document clinical findings thoroughly
- Contact receiving facility to arrange transfer
- Provide initial stabilization as needed
- Complete referral form with essential information
- Arrange appropriate transportation
- Educate patient/family about reason for referral
- Follow up to ensure patient reached referral center
- Document outcomes and maintain continuity of care
Follow-up Care
Effective follow-up care is essential for monitoring treatment efficacy, preventing recurrence, and managing chronic manifestations of filariasis.
Follow-up Schedule
| Time Period | Assessment Focus | Nursing Interventions |
|---|---|---|
| Immediate Post-Treatment (1-7 days) |
|
|
| Short-term (1-3 months) |
|
|
| Intermediate (3-12 months) |
|
|
| Long-term (Annual) |
|
|
Follow-up Documentation
Community health nurses should maintain detailed records including:
- Treatment history and compliance
- Lymphedema measurements and grading
- Episodes of acute dermatolymphangioadenitis (ADL)
- Secondary complications
- Impact on daily activities and quality of life
- Referrals and specialty care received
Community-Based Follow-up Strategies
- Self-help groups for patients with chronic manifestations
- Peer educators to reinforce self-care practices
- Community health workers for home-based follow-up
- Mobile health clinics in remote endemic areas
- Telemedicine consultations where available
- Integration with existing primary healthcare services
Patient Follow-up Card
A standardized patient-held record can facilitate continuity of care. Key elements include:
- Patient identification and contact information
- Diagnosis details and date
- Treatment regimen and dates
- Follow-up appointment schedule
- Lymphedema measurements and progression
- ADL episode record
- Self-care adherence checklist
- Contact information for emergency assistance
Nursing Interventions
Comprehensive nursing care for filariasis patients encompasses various interventions across the disease spectrum. These interventions are guided by the nursing process: assessment, diagnosis, planning, implementation, and evaluation.
Assessment
- Physical Assessment:
- Inspection of limbs for edema, skin changes
- Measurement of limb circumference
- Assessment of mobility and functional capacity
- Examination for entry lesions or infections
- Psychosocial Assessment:
- Impact of condition on daily activities
- Social isolation or stigma experiences
- Emotional response to chronic condition
- Family support system
- Environmental Assessment:
- Home conditions affecting hygiene practices
- Access to clean water
- Vector breeding sites near residence
- Protective measures in use
Common Nursing Diagnoses
- Impaired Skin Integrity related to chronic lymphedema
- Chronic Pain related to lymphatic inflammation
- Impaired Physical Mobility related to limb enlargement
- Risk for Infection related to compromised lymphatic system
- Disturbed Body Image related to visible physical changes
- Ineffective Health Maintenance related to insufficient knowledge
- Social Isolation related to stigma of visible manifestations
Implementation: Nursing Interventions by Disease Stage
| Disease Stage | Nursing Interventions |
|---|---|
| Asymptomatic Infection |
|
| Acute Manifestations |
|
| Early Lymphedema |
|
| Advanced Lymphedema |
|
| Psychosocial Support (All Stages) |
|
Health Education Topics
- Disease Process: Transmission cycle, progression, potential complications
- Treatment Adherence: Importance of completing medication course
- Self-Management: Daily hygiene practices, exercises, elevation
- Early Warning Signs: Recognizing infections requiring medical attention
- Environmental Control: Reducing mosquito breeding sites
- Protection Methods: Bed nets, repellents, clothing
- Psychological Adaptation: Coping with chronic condition
Mnemonic: “CARE FOR FILARIASIS”
Key nursing care principles:
- C – Clean affected areas daily
- A – Apply moisturizer to prevent skin cracks
- R – Raise limbs when resting
- E – Exercise regularly to promote lymph flow
- F – Fungal infections need prevention
- O – Observe for signs of infection
- R – Reduce standing/sitting for prolonged periods
- F – Follow medication regimen
- I – Inspect skin daily
- L – Limit exposure to mosquitoes
- A – Avoid injury to affected limbs
- R – Remember compression if prescribed
- I – Immediate attention to wounds
- A – Attend follow-up appointments
- S – Seek support from family/community
- I – Incorporate self-care into daily routine
- S – Stay hydrated and maintain nutrition
Community Initiatives and Global Practices
Successful filariasis control and elimination programs around the world offer valuable lessons for community health nursing practice. These initiatives demonstrate the effectiveness of coordinated approaches to disease management.
Global Elimination Program
The Global Programme to Eliminate Lymphatic Filariasis (GPELF), launched by WHO in 2000, aims to eliminate lymphatic filariasis as a public health problem by 2030. The program employs a two-pronged strategy:
- Interrupt transmission through mass drug administration (MDA)
- Alleviate suffering through morbidity management and disability prevention (MMDP)
Successful Country Programs
| Country/Region | Successful Approaches | Nursing Implications |
|---|---|---|
| India |
|
|
| Sri Lanka |
|
|
| Samoa |
|
|
| Tanzania |
|
|
| Brazil |
|
|
Innovative Community Approaches
- Community Drug Distributors (CDDs): Trained community members who distribute medications during MDA campaigns
- Lymphedema Management Groups: Patient-led support groups for self-care education and emotional support
- Mobile Health Technologies: SMS reminders for MDA days and treatment adherence
- Integrated NTD Approaches: Combining filariasis with other neglected tropical disease control efforts
- School-Based Education: Engaging children as change agents for prevention practices
- Faith-Based Organizations: Utilizing religious leaders to address stigma and encourage participation
Case Study: Community Care Groups in Haiti
In Haiti, “community care groups” have been effective in filariasis control. Each group consists of 10-15 volunteer community health workers who each work with 10-15 households. These volunteers:
- Conduct monthly home visits
- Provide education on filariasis prevention
- Demonstrate lymphedema care techniques
- Monitor MDA compliance
- Identify and refer cases with complications
This approach has achieved high MDA coverage rates (>80%) and improved lymphedema self-management practices. Community health nurses supervise and train these volunteers, creating a sustainable care network.
Lessons for Nursing Practice
Key lessons from global initiatives that can be applied in community health nursing:
- Integration: Embedding filariasis control within existing health services
- Community Engagement: Involving community members in all aspects of programs
- Cultural Adaptation: Tailoring interventions to local contexts and beliefs
- Sustainable Approaches: Building local capacity for long-term management
- Comprehensive Care: Addressing both disease transmission and chronic morbidity
- Data-Driven Strategies: Using surveillance data to target interventions
- Multisectoral Collaboration: Working with water, sanitation, and education sectors
Transferable Best Practices for Community Health Nurses
- Community Mapping: Identifying high-risk areas and vulnerable populations
- Cascade Training: Training community volunteers who then train households
- Simple Tools: Using pictorial guides for patient education
- Integration Opportunities: Combining filariasis activities with other health services
- Monitoring Systems: Simple tracking methods for community-based interventions
- Stigma Reduction: Community events celebrating progress and supporting affected individuals
- Income Generation: Supporting livelihood activities for affected individuals
