Dengue Fever
Epidemiology, Prevention, Screening and Management
A Community Health Nursing Perspective
Table of Contents
Introduction to Dengue Fever
Dengue fever is a mosquito-borne viral infection that has become a major public health concern globally. It is transmitted primarily by female Aedes aegypti mosquitoes and, to a lesser extent, by Aedes albopictus. As community health nurses, understanding dengue is essential for effective prevention, early detection, and management of outbreaks within communities.
Key Facts About Dengue
- Dengue is caused by any of four dengue virus serotypes (DENV-1, DENV-2, DENV-3, and DENV-4)
- Approximately 100-400 million infections occur annually worldwide
- The global incidence of dengue has grown dramatically in recent decades
- About half of the world’s population is now at risk of dengue infection
- Dengue is endemic in over 100 countries, primarily in tropical and subtropical regions
Clinical Manifestations
Dengue fever presents with a wide spectrum of clinical manifestations, ranging from asymptomatic infection to severe dengue. Understanding these manifestations is crucial for community health nurses to identify potential cases and implement appropriate interventions.
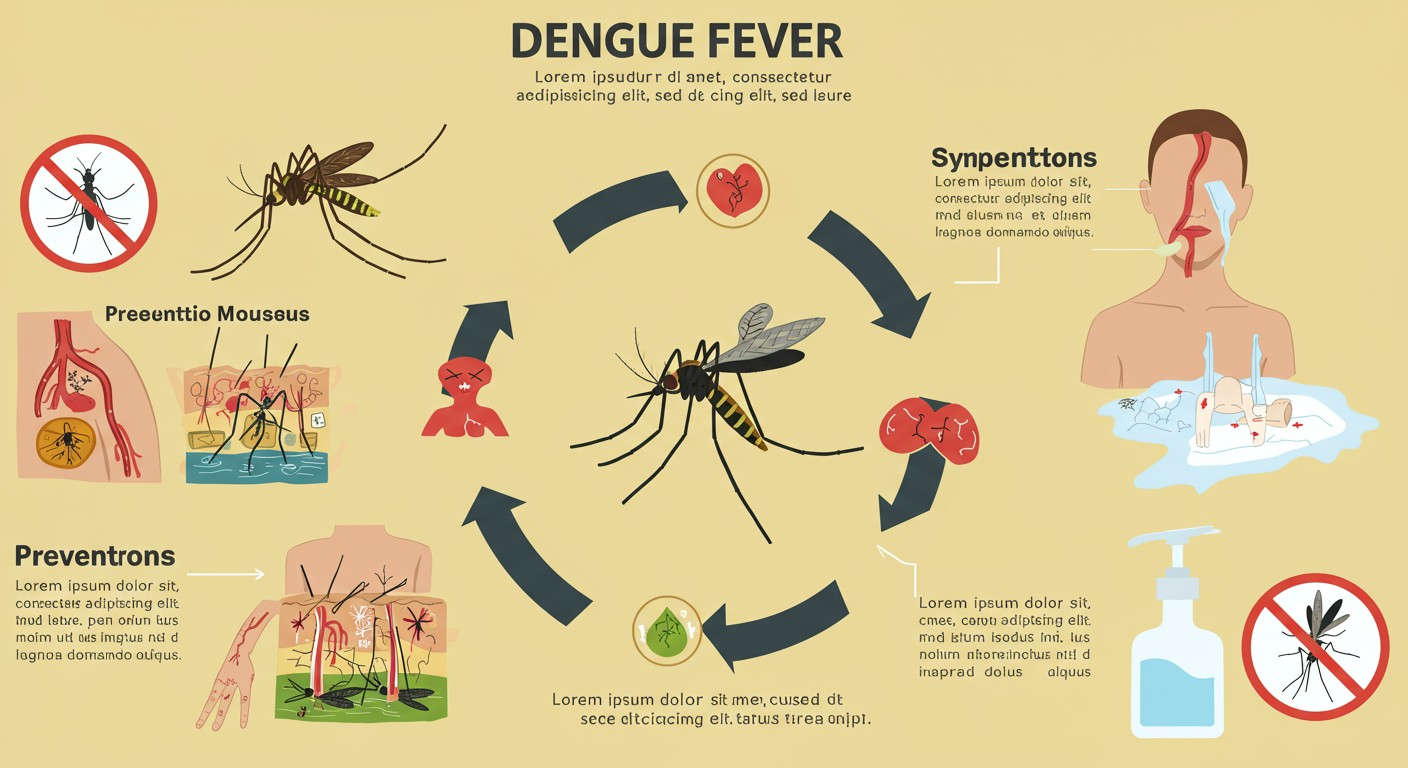
Fig 1: Dengue fever mosquito life cycle, symptoms, and prevention measures
Epidemiology of Dengue
Global Distribution
Dengue is now endemic in more than 100 countries across the Americas, South-East Asia, Western Pacific, Africa, and Eastern Mediterranean regions. The incidence of dengue has increased 30-fold over the last 50 years, with up to 400 million infections occurring annually, of which approximately 100 million manifest clinically.
Risk Factors
Environmental Factors
- Tropical and subtropical climate (temperature, humidity)
- Unplanned rapid urbanization
- Inadequate water storage practices
- Improper solid waste disposal
Human Factors
- Population density and growth
- Global travel and trade
- Lack of effective mosquito control
- Low community awareness and participation
Biological Factors
- Multiple dengue virus serotypes
- Individual susceptibility
- Previous dengue infection (risk for severe dengue)
- Adaptation of the vector to urban environments
Transmission Dynamics
Understanding dengue transmission patterns is essential for effective community-based interventions. The transmission cycle involves:
- Human-to-mosquito transmission: When a mosquito bites a person infected with dengue during the viremic phase (usually 4-5 days after fever onset)
- Extrinsic incubation period: The virus develops within the mosquito for 8-12 days
- Mosquito-to-human transmission: After the extrinsic incubation period, infected mosquitoes can transmit the virus for the rest of their lives
- Intrinsic incubation period: After a human is bitten, symptoms appear within 3-14 days (average 4-7 days)
Seasonal Patterns
Dengue exhibits seasonal patterns that correlate with increased vector abundance and activity. These patterns are essential for community health nurses to anticipate and prepare for potential outbreaks:
| Region | Peak Season | Associated Factors |
|---|---|---|
| Southeast Asia | Monsoon and post-monsoon seasons | Increased rainfall, water accumulation, humidity |
| Americas | Rainy season, summer months | Increased temperature, precipitation |
| Western Pacific | Wet season | Rainfall, water storage practices |
| Africa | Rainy season | Standing water, temperature increases |
Community Health Nursing Relevance:
Understanding the epidemiological patterns of dengue enables community health nurses to implement timely interventions, allocate resources effectively, and educate communities about preventive measures during high-risk periods. This epidemiological knowledge is the foundation for developing targeted dengue prevention and control strategies.
Vector Information
Primary Vectors of Dengue
The primary vectors responsible for dengue transmission are Aedes aegypti and Aedes albopictus mosquitoes. Understanding their characteristics is crucial for implementing effective vector control strategies.
Aedes aegypti
- Principal vector of dengue worldwide
- Highly domesticated, prefers to live close to humans
- Breeds primarily in artificial containers
- Day-biting species with peak activity at dawn and dusk
- Limited flight range (usually less than 100 meters)
- Easily recognizable by white markings on legs and thorax
Aedes albopictus
- Secondary dengue vector, known as “Asian tiger mosquito”
- More adaptable to cooler temperatures than Ae. aegypti
- Can breed in natural and artificial containers
- Has expanded its geographic range globally
- Day-biting behavior
- Can tolerate rural and peri-urban environments
Vector Life Cycle
The life cycle of Aedes mosquitoes involves four distinct stages. Understanding this cycle is essential for implementing targeted vector control interventions.
| Stage | Duration | Description | Control Implications |
|---|---|---|---|
| Egg | 2-7 days (can survive desiccation for months) | Laid individually on water surfaces or damp substrates | Regular container emptying and cleaning to remove eggs |
| Larva | 5-14 days (temperature dependent) | Aquatic stage, requires water to develop | Larviciding, biological control, source reduction |
| Pupa | 1-4 days | Non-feeding stage, mobile in water | Similar to larval control methods |
| Adult | 2-4 weeks (in favorable conditions) | Flying stage, females require blood meals for egg production | Indoor residual spraying, space spraying, personal protection |
Vector Behavior Relevant to Transmission
- Feeding patterns: Primarily day-biting, with peak activity in early morning and late afternoon
- Multiple feeding: Ae. aegypti often takes multiple blood meals during a single gonotrophic cycle
- Indoor resting: Tends to rest indoors, often in dark, cool areas
- Anthropophilic behavior: Strong preference for human blood
- Breeding site preference: Artificial containers with clean water (tires, flower pots, water storage containers)
Mnemonic: “ABCDE” of Dengue Vectors
- A – Aedes mosquitoes are the primary vectors
- B – Breeding in artificial containers
- C – Clean water preference for laying eggs
- D – Daytime biting behavior
- E – Eggs can survive desiccation for months
Prevention & Control Measures
Effective prevention and control of dengue requires a comprehensive approach targeting both the vector and human components of transmission. Community health nurses play a pivotal role in implementing these measures at the community level.
Vector Control Strategies
Environmental Management
- Source reduction (elimination of breeding sites)
- Container management (covering, emptying, cleaning)
- Proper disposal of solid waste
- Modification of water storage practices
- Improved urban planning and housing design
Chemical Control
- Larvicides in water containers (temephos, Bti)
- Adulticides for space spraying during outbreaks
- Indoor residual spraying
- Insecticide-treated materials
- Novel approaches (attractive toxic sugar baits)
Biological Control
- Introduction of larvivorous fish (e.g., Gambusia)
- Use of copepods in water containers
- Release of genetically modified mosquitoes
- Wolbachia-infected mosquitoes
- Sterile insect technique
Personal Protection Measures
- Use of insect repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus
- Wearing long-sleeved shirts and long pants, especially during peak mosquito activity
- Installing and maintaining window and door screens
- Using bed nets (especially for daytime sleeping children, elderly, and sick individuals)
- Avoiding outdoor activities during peak biting times
Community Engagement and Education
Community health nurses are uniquely positioned to engage communities in dengue prevention and control efforts. Effective community engagement includes:
Mnemonic: “CLEAN UP” Strategy for Community-Based Dengue Prevention
- C – Communication of dengue risks and prevention methods
- L – Local leadership involvement and capacity building
- E – Education on vector biology and control techniques
- A – Action-oriented community participation
- N – Network development among stakeholders
- U – Understanding local contexts and barriers
- P – Persistence in implementing control measures
Integrated Vector Management (IVM)
The WHO recommends an Integrated Vector Management approach that combines multiple control strategies tailored to local contexts. Community health nurses should promote this comprehensive approach, which includes:
- Evidence-based decision making
- Integrated approaches (combining methods)
- Collaboration within the health sector and with other sectors
- Advocacy, social mobilization, and legislation
- Capacity building at all levels
Important Consideration for Community Health Nurses:
Dengue prevention programs must be sustainable and engage communities as active partners rather than passive recipients. One-time interventions or purely top-down approaches often fail to produce lasting results. Community ownership is essential for the sustainability of dengue control efforts.
Screening Methods
Early identification of dengue cases through effective screening is critical for prompt intervention and outbreak control. Community health nurses play a vital role in implementing dengue screening in primary healthcare settings and during community outreach activities.
Clinical Screening
Clinical screening involves the systematic assessment of individuals for signs and symptoms suggestive of dengue infection. This approach is particularly important in resource-limited settings where laboratory testing may not be readily available.
Key Clinical Features to Screen For:
- Sudden onset of high fever (typically 39-40°C/102-104°F)
- Severe headache (typically frontal)
- Retro-orbital (behind the eye) pain
- Myalgia (muscle pain) and arthralgia (joint pain)
- Nausea and vomiting
- Rash (typically appears 3-4 days after fever onset)
- Mild bleeding manifestations (petechiae, ecchymosis, bleeding gums, epistaxis)
- Leukopenia (decreased white blood cell count)
WHO Dengue Case Classification
The World Health Organization’s revised dengue case classification system provides a framework for screening and categorizing dengue cases according to their severity.
| Classification | Clinical Features | Screening Actions |
|---|---|---|
| Dengue without warning signs | Fever with two of the following: nausea/vomiting, rash, aches and pains, leukopenia | Monitor for warning signs, ensure adequate fluid intake, check for dehydration |
| Dengue with warning signs | Above plus: abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy/restlessness, liver enlargement, increase in hematocrit with decrease in platelets | Refer for in-hospital observation, initiate IV fluid therapy if needed |
| Severe dengue | Severe plasma leakage (shock, fluid accumulation with respiratory distress), severe bleeding, severe organ involvement | Immediate emergency referral, urgent fluid resuscitation |
Rapid Diagnostic Tests (RDTs)
Rapid diagnostic tests are valuable screening tools that can be used at the point of care by community health nurses. These tests detect dengue viral antigens or anti-dengue antibodies.
NS1 Antigen Tests
- Detects dengue NS1 antigen
- Most useful during the first week of illness
- Sensitivity: 60-90%
- Specificity: 95-100%
- Results available in 15-30 minutes
- Can detect infection before antibody response
IgM/IgG Antibody Tests
- Detects anti-dengue IgM and/or IgG antibodies
- IgM detectable 5-7 days after onset of symptoms
- IgG rises later or immediately in secondary infections
- Sensitivity: 80-90% (after day 5)
- Specificity: 80-95%
- Cross-reactivity with other flaviviruses
Community-Based Screening Approaches
Community health nurses can implement various screening approaches to detect dengue cases early in community settings:
- Fever surveillance: Systematic screening of individuals with acute febrile illness in endemic areas
- School absenteeism monitoring: Tracking patterns of student absences due to fever
- Community health worker networks: Training local health workers to recognize and report suspected cases
- Mobile screening clinics: Temporary clinics in high-risk areas during dengue season
- Active case finding: Door-to-door screening during outbreaks
Mnemonic: “FEVER” Screening Protocol
- F – Find cases through active surveillance
- E – Evaluate using clinical criteria and warning signs
- V – Verify with rapid diagnostic tests when available
- E – Educate patients about warning signs to monitor
- R – Refer cases with warning signs or severe manifestations
Community Health Nursing Tip:
Integrate dengue screening with other routine health services to maximize efficiency and coverage. For example, include dengue screening during maternal and child health visits, immunization sessions, or community outreach activities during dengue season.
Diagnostic Approaches
While screening helps identify suspected dengue cases, definitive diagnosis requires laboratory confirmation. Community health nurses should understand the various diagnostic methods available, their interpretation, and the appropriate timing for each test.
Laboratory Diagnostic Methods
| Diagnostic Method | Timing | Advantages | Limitations |
|---|---|---|---|
| Virus isolation | 0-5 days after onset | Gold standard; identifies serotype | Time-consuming (1-2 weeks); requires specialized facilities |
| RT-PCR | 0-7 days after onset | Rapid; highly sensitive and specific; identifies serotype | Requires specialized equipment; relatively expensive |
| NS1 antigen detection | 0-7 days after onset | Early diagnosis; rapid tests available | Variable sensitivity; doesn’t identify serotype |
| IgM ELISA | 5+ days after onset | Widely available; relatively inexpensive | Not detectable early; cross-reactivity with other flaviviruses |
| IgG ELISA | 7+ days (primary); earlier in secondary | Can distinguish primary from secondary infections | Significant cross-reactivity; requires paired samples for confirmation |
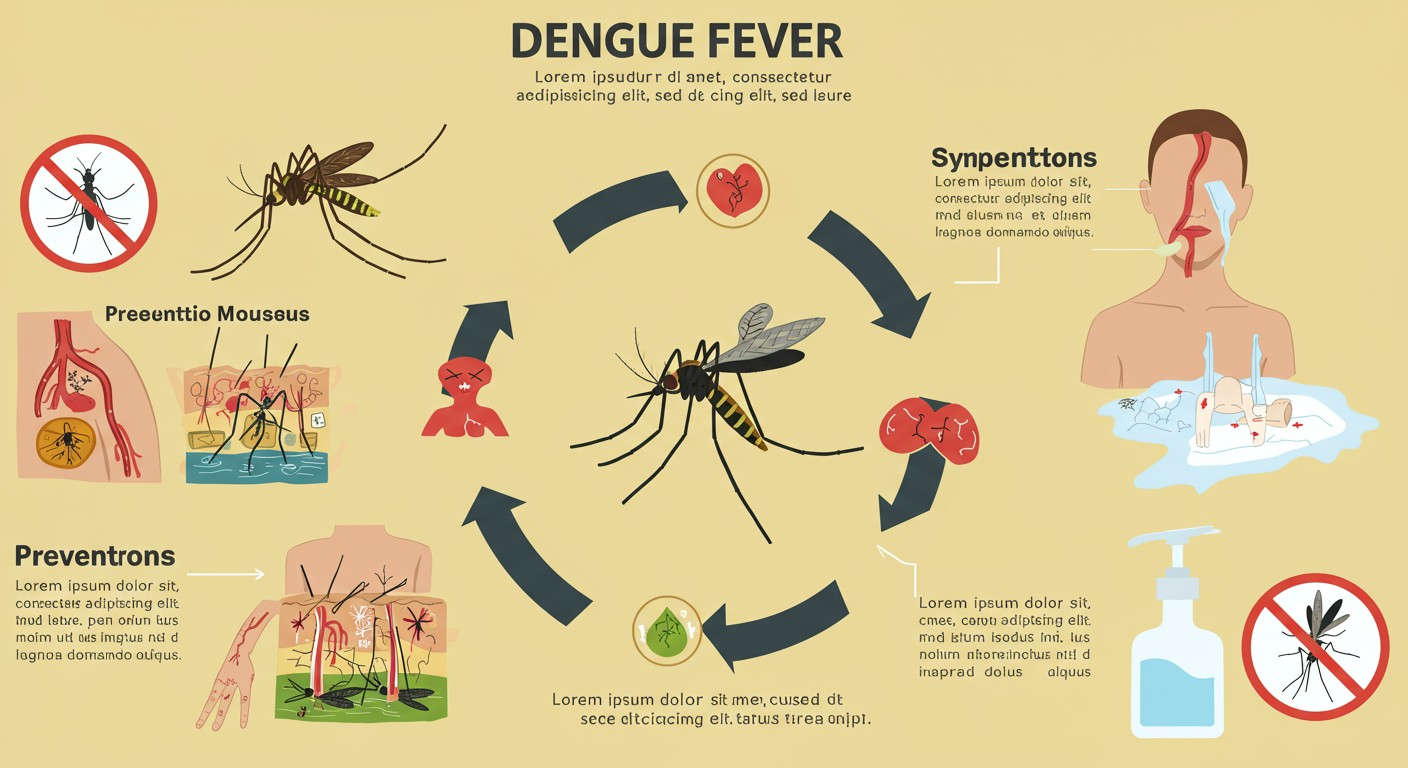
Fig 2: Timeline of dengue infection showing diagnostic markers and appropriate testing windows
Essential Laboratory Investigations
In addition to specific dengue diagnostic tests, several routine laboratory investigations are crucial for assessing disease severity and guiding management decisions.
Complete Blood Count (CBC)
- Leukopenia (white blood cell count < 5,000/mm³)
- Thrombocytopenia (platelet count < 150,000/mm³)
- Hemoconcentration (hematocrit increase ≥ 20% from baseline)
- Monitor trends over time, not just absolute values
- Serial monitoring recommended during critical phase
Other Relevant Tests
- Liver function tests (elevated AST/ALT)
- Serum albumin (decreased in plasma leakage)
- Blood glucose (monitor for hypo/hyperglycemia)
- Coagulation profile (PT, PTT, fibrinogen)
- Renal function tests (BUN, creatinine)
Differential Diagnosis
Accurate diagnosis of dengue requires consideration of other febrile illnesses that may present similarly. Community health nurses should be aware of key differential diagnoses:
- Other arboviral infections: Chikungunya, Zika, Yellow fever
- Malaria: Especially important in co-endemic areas
- Leptospirosis: Similar epidemiological settings
- Typhoid fever: Prolonged fever, gastrointestinal symptoms
- Influenza: Respiratory symptoms more prominent
- Measles: Characteristic rash pattern
- Rubella: Milder illness with lymphadenopathy
- Rickettsial infections: Eschar may be present
Diagnostic Challenges in Community Settings:
In many endemic areas, limited access to laboratory facilities may restrict diagnostic capabilities. Community health nurses should utilize available resources effectively, prioritize testing based on clinical presentation, and establish clear referral pathways for cases requiring advanced diagnostic workup.
Mnemonic: “DENGUE” Diagnostic Approach
- D – Determine timing of symptom onset
- E – Evaluate clinical features and warning signs
- N – NS1 testing if within first week
- G – Get complete blood count for platelet and hematocrit trends
- U – Utilize serology (IgM/IgG) after day 5
- E – Exclude other similar febrile illnesses
Primary Management
The primary management of dengue focuses on supportive care, close monitoring for complications, and prompt recognition of warning signs that may indicate progression to severe disease. Community health nurses play a crucial role in the initial management of dengue cases, especially in outpatient settings.
Management Principles Based on Disease Phase
Dengue has three distinct phases (febrile, critical, and recovery), each requiring specific management approaches.
| Phase | Duration | Clinical Features | Management Approach |
|---|---|---|---|
| Febrile Phase | 2-7 days | High fever, headache, myalgia, arthralgia, mild bleeding manifestations |
|
| Critical Phase | 24-48 hours (days 3-7) | Defervescence, plasma leakage, hemoconcentration, thrombocytopenia, bleeding, organ impairment |
|
| Recovery Phase | 2-3 days | Clinical improvement, resolution of plasma leakage, diuresis, stabilization of hematocrit, recovery of platelet count |
|
Outpatient Management Guidelines for Community Health Nurses
- Hydration therapy:
- Encourage oral fluids (ORS, fruit juices, coconut water)
- Minimum intake: 2-3 liters per day for adults or age-appropriate amounts for children
- Monitor urine output (frequency, volume, color)
- Fever management:
- Acetaminophen/paracetamol (not exceeding 4g/day for adults)
- Tepid sponging for high fever
- Avoid aspirin, ibuprofen, and other NSAIDs due to bleeding risk
- Symptom relief:
- Antiemetics if needed for nausea/vomiting
- Rest and limited physical activity
- Nutritional support (small, frequent meals if appetite is poor)
- Monitoring:
- Daily follow-up during febrile phase if possible
- CBC monitoring every 24-48 hours during critical period
- Temperature chart maintained by patient/family
- Fluid intake/output record
Warning Signs Requiring Immediate Attention
Critical Warning Signs:
- Severe abdominal pain or tenderness
- Persistent vomiting (≥3 times in 1 hour or ≥4 times in 6 hours)
- Clinical fluid accumulation (ascites, pleural effusion)
- Mucosal bleeding (gums, nose, gastrointestinal tract)
- Lethargy or restlessness
- Liver enlargement >2 cm
- Laboratory: increase in hematocrit concurrent with rapid decrease in platelet count
Action: Immediate referral to a hospital setting
Home-Based Care Instructions
Community health nurses should provide clear instructions to patients and caregivers for home-based management:
Mnemonic: “FLUID” Home Care Protocol
- F – Fluids – Increase oral fluid intake
- L – Look for warning signs and seek immediate care if they appear
- U – Use only acetaminophen for fever (no aspirin or NSAIDs)
- I – Intake and output monitoring
- D – Daily follow-up with healthcare provider during critical period
Community Health Nursing Strategy:
Consider implementing a community-based monitoring system for dengue patients managed at home. This could include training community health workers to conduct daily home visits during dengue outbreaks to monitor patients’ clinical status, provide supportive care, and facilitate early referral when necessary.
Referral Criteria
Timely and appropriate referral is critical in dengue management. Community health nurses must recognize conditions that require higher levels of care and establish efficient referral pathways to minimize delays in treatment.
Indications for Hospital Referral
Clinical Indications
- Presence of any warning signs
- Signs of severe dengue (shock, severe bleeding, organ impairment)
- Hemodynamic instability
- Persistent high fever (>39°C for >5 days)
- Pregnancy
- Infants and elderly patients
- Significant comorbidities (diabetes, hypertension, etc.)
- Inability to maintain oral hydration
Laboratory Indications
- Rapidly decreasing platelet count (<100,000/mm³)
- Rising hematocrit (>20% increase from baseline)
- Evidence of organ dysfunction (elevated liver enzymes, impaired renal function)
- Metabolic acidosis
- Abnormal coagulation profile
- Significant electrolyte imbalances
Social Indications for Referral
- Living alone without adequate support for monitoring
- Limited access to healthcare facilities (remote locations)
- Inability to return for follow-up
- Inadequate home care conditions
- Poor compliance with outpatient management
- Multiple family members affected simultaneously
Preparation for Referral
Community health nurses should follow these steps when referring dengue patients to higher levels of care:
- Initial stabilization: Start oral or IV rehydration as appropriate before transport
- Documentation: Prepare a comprehensive referral note including:
- Duration of illness
- Clinical findings and vital signs
- Warning signs observed
- Laboratory results (if available)
- Treatment already administered
- Reason for referral
- Communication: Contact receiving facility to inform about the case
- Transportation: Arrange appropriate transport with monitoring capabilities
- Family support: Brief family members on the need for referral and next steps
Referral Pathway Framework
Community health nurses should help establish clear referral pathways for dengue cases, which include:
| Level of Care | Capabilities | Types of Dengue Cases Managed |
|---|---|---|
| Primary Care / Community Health Center | Basic clinical assessment, CBC, NS1/rapid tests, oral rehydration | Uncomplicated dengue without warning signs |
| Secondary Care / District Hospital | IV fluid therapy, more extensive laboratory tests, monitoring capabilities | Dengue with warning signs, mild to moderate complications |
| Tertiary Care / Specialist Center | ICU facilities, blood products, specialist care, mechanical ventilation | Severe dengue, organ dysfunction, major bleeding, shock |
Critical Consideration:
Referral decisions should be made early rather than late. The transition from non-severe to severe dengue can occur rapidly, particularly during the critical phase. When in doubt, it is safer to refer patients to a higher level of care, especially in remote areas where transportation delays may be significant.
Community Health Nursing Action:
Develop and maintain an updated directory of referral facilities with their capabilities, contact information, and transportation options. This directory should be readily available to all community health nurses, especially during dengue outbreaks.
Follow-up Protocols
Proper follow-up of dengue cases is essential for monitoring recovery, detecting late complications, and preventing future infections. Community health nurses should implement systematic follow-up protocols adapted to local contexts and resource availability.
Follow-up Schedule for Dengue Patients
The frequency and components of follow-up depend on the phase of illness and risk factors:
| Phase | Follow-up Frequency | Key Assessment Components |
|---|---|---|
| Febrile Phase (Outpatient) | Daily until defervescence |
|
| Critical Phase (Hospital) | Multiple times daily |
|
| Recovery Phase | Daily until clinically stable, then weekly |
|
| Post-Recovery | 2-4 weeks after recovery |
|
Home-Based Follow-up by Community Health Nurses
- Home visits: Scheduled visits to assess recovering patients, especially for vulnerable populations
- Telephone follow-up: Regular calls to monitor symptoms and adherence to care instructions
- Community health worker engagement: Training local health workers to conduct basic follow-up
- Group follow-up sessions: For multiple recovering patients in a community
- Mobile health technologies: SMS reminders, symptom reporting apps, telemedicine consultations
Post-Dengue Complications to Monitor
Community health nurses should be aware of potential post-dengue complications and include their assessment in follow-up protocols:
Short-term Complications
- Post-dengue fatigue syndrome
- Depression and psychological effects
- Prolonged convalescence in elderly
- Secondary bacterial infections
- Rebound thrombocytosis
Long-term Complications
- Persistent fatigue and weakness
- Neurological sequelae
- Renal complications in severe cases
- Chronic liver dysfunction
- Immune-mediated complications
Prevention of Re-infection
An essential component of follow-up is education to prevent future dengue infections:
Mnemonic: “PREVENT” Secondary Infection Strategy
- P – Personal protection measures (repellents, protective clothing)
- R – Remove standing water around the home
- E – Eliminate mosquito breeding sites weekly
- V – Verify that water storage containers are covered
- E – Educate family members about dengue prevention
- N – Network with neighbors for community-wide prevention
- T – Take extra precautions during outbreaks
Community Surveillance and Follow-up
In addition to individual patient follow-up, community health nurses should implement broader surveillance and follow-up activities:
- Active case finding in neighborhoods with reported cases
- Vector surveillance in affected communities
- Monitoring of fever clusters and school absenteeism
- Community education sessions following local outbreaks
- Evaluation of prevention practices post-outbreak
- Documentation and reporting to local health authorities
Documentation and Record-Keeping:
Maintain comprehensive records of all follow-up activities using standardized forms. These records serve multiple purposes: monitoring individual patient outcomes, identifying patterns in community spread, evaluating intervention effectiveness, and providing data for future outbreak preparedness. Digital health records and mobile applications can facilitate more efficient documentation and analysis.
Global Best Practices in Dengue Control
Several countries have implemented successful dengue prevention and control programs that can serve as models for community health nursing interventions. These best practices demonstrate the effectiveness of integrated, community-based approaches.
Singapore’s Integrated Vector Management Approach
Singapore has achieved significant success in dengue control through its comprehensive National Dengue Prevention and Control Program:
- Strong legislative framework with penalties for premises with mosquito breeding
- Regular premise inspections using digital tools for data collection
- Integrated surveillance system combining entomological, virological, and clinical data
- Public education campaigns with clear messaging
- Community engagement through grassroots organizations
- Use of technology for risk prediction and resource allocation
Key Lesson for Community Health Nursing: Systematic inspection routines combined with community accountability can significantly reduce breeding sites.
Cuba’s Community Participation Model
Cuba’s approach emphasizes strong community participation in dengue control:
- Family doctor and nurse teams responsible for specific geographic areas
- House-to-house active surveillance during outbreaks
- Community working groups involved in decision-making
- Integration of vector control into primary healthcare services
- Rapid response teams for outbreak management
- Sustained political commitment and intersectoral coordination
Key Lesson for Community Health Nursing: Integration of dengue control activities into primary healthcare systems improves sustainability and effectiveness.
Thailand’s School-Based Prevention Programs
Thailand has successfully implemented school-based dengue prevention programs:
- Integration of dengue education into school curricula
- Student “dengue scouts” trained to identify and eliminate breeding sites
- Regular mosquito larvae surveys conducted by students
- School-to-community knowledge transfer
- Competitive activities between schools to promote engagement
- Collaboration between health and education sectors
Key Lesson for Community Health Nursing: Engaging children as agents of change can effectively spread prevention knowledge throughout communities.
Vietnam’s Biological Control Innovation
Vietnam has pioneered community-based biological control methods:
- Use of Mesocyclops copepods in water storage containers
- Community-based production and distribution systems
- Women’s Union members as key implementers
- Combination with community clean-up campaigns
- Sustained coverage through community ownership
- Significant reductions in dengue incidence in implementation areas
Key Lesson for Community Health Nursing: Locally appropriate, sustainable biological control methods can be effectively implemented through community structures.
Mexico’s Risk Communication Strategy
Mexico has developed effective risk communication approaches for dengue prevention:
- Targeted messaging based on formative research
- Use of multiple communication channels (mass media, social media, interpersonal)
- Clear, actionable messages focused on specific behaviors
- Seasonal communication campaigns aligned with vector abundance
- Involvement of local influencers and community leaders
- Evaluation and adaptation of messaging based on community feedback
Key Lesson for Community Health Nursing: Evidence-based risk communication that addresses local perceptions and barriers can significantly improve preventive behaviors.
Adaptation for Local Implementation:
When adapting these global best practices, community health nurses should consider:
- Local epidemiological patterns of dengue transmission
- Available resources and infrastructure
- Cultural norms and community structures
- Existing health system organization
- Community preferences and priorities
The most successful programs combine elements from multiple approaches and adapt them to local contexts with strong community involvement in planning and implementation.
References
- World Health Organization. (2022). Dengue and Severe Dengue. Retrieved from https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue
- World Health Organization. (2009). Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. Geneva: World Health Organization.
- Centers for Disease Control and Prevention. (2021). Dengue: Clinical Guidance. Retrieved from https://www.cdc.gov/dengue/healthcare-providers/clinical-guidance.html
- Pan American Health Organization. (2016). Integrated Management Strategy for Dengue Prevention and Control in the Region of the Americas. Washington, D.C.: PAHO.
- Wilder-Smith, A., Ooi, E. E., Horstick, O., & Wills, B. (2019). Dengue. The Lancet, 393(10169), 350-363.
- Guzman, M. G., & Harris, E. (2015). Dengue. The Lancet, 385(9966), 453-465.
- Kularatne, S. A. (2015). Dengue fever. BMJ, 351, h4661.
- Achee, N. L., Gould, F., Perkins, T. A., Reiner, R. C., Morrison, A. C., Ritchie, S. A., … & Scott, T. W. (2015). A critical assessment of vector control for dengue prevention. PLoS Neglected Tropical Diseases, 9(5), e0003655.
- Bowman, L. R., Donegan, S., & McCall, P. J. (2016). Is dengue vector control deficient in effectiveness or evidence?: Systematic review and meta-analysis. PLoS Neglected Tropical Diseases, 10(3), e0004551.
- Anders, K. L., & Hay, S. I. (2012). Lessons from malaria control to help meet the rising challenge of dengue. The Lancet Infectious Diseases, 12(12), 977-984.
- World Health Organization. (2012). Global strategy for dengue prevention and control 2012-2020. Geneva: World Health Organization.
- Thisyakorn, U., & Thisyakorn, C. (2014). Latest developments and future directions in dengue vaccines. Therapeutic Advances in Vaccines, 2(1), 3-9.
