Viral Hepatitis Treatment in Community
A Community Health Nursing Perspective
Table of Contents
1. Introduction to Viral Hepatitis
Viral hepatitis is a widespread inflammation of the liver that results in degeneration and necrosis of liver cells. It represents a significant public health challenge globally, affecting millions of people and causing substantial morbidity and mortality. From a community health nursing perspective, understanding viral hepatitis treatment in community settings is crucial for effective patient management and disease control.
The term “hepatitis” refers to inflammation of the liver, which can be caused by various factors, including:
- Viral infections (hepatitis A, B, C, D, E, and G)
- Bacterial invasions
- Injury by physical agents
- Toxic chemical agents (drugs, alcohol, industrial chemicals)
- Autoimmune responses
This comprehensive guide focuses primarily on the viral causes of hepatitis and their treatment in community settings, emphasizing the community health nursing perspective. Viral hepatitis creates a global health burden with significant morbidity and mortality from both acute infection and chronic complications. The condition can be self-limiting or can progress to liver fibrosis (scarring), cirrhosis, or liver cancer.
Important Concept
Viral hepatitis treatment in community settings requires a comprehensive approach that includes prevention, screening, diagnosis, management, and follow-up care. Community health nurses play a pivotal role in all aspects of this process, serving as educators, advocates, care coordinators, and providers.
2. Epidemiology of Viral Hepatitis
Understanding the epidemiology of viral hepatitis is essential for developing effective community-based prevention and treatment strategies. The global burden of viral hepatitis continues to grow, with significant variations across regions, age groups, and viral types.
Global Burden
- An estimated 254 million people are living with hepatitis B and 50 million with hepatitis C worldwide (WHO, 2022)
- Approximately 1.3 million deaths occur annually due to viral hepatitis (3,500 deaths per day)
- About 6,000 people are newly infected with viral hepatitis each day
- Viral hepatitis is the seventh leading cause of mortality globally
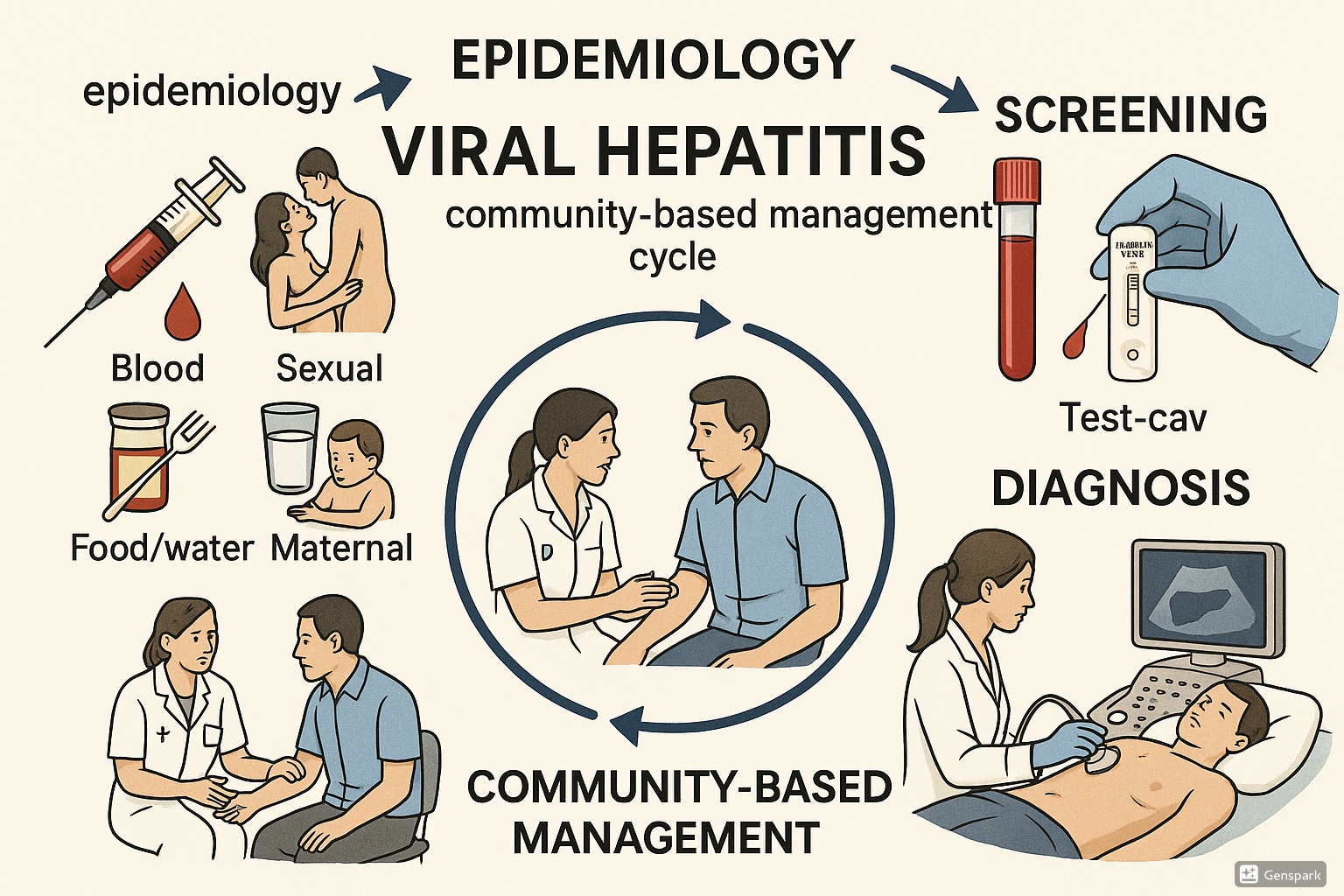
Figure 1: Comprehensive overview of viral hepatitis epidemiology, screening, diagnosis, and community-based management
Prevalence by Hepatitis Type
| Hepatitis Type | Global Prevalence | Major Affected Regions | Annual Deaths |
|---|---|---|---|
| Hepatitis A | ~100 million infections annually | Low-income regions with poor sanitation | 15,000-30,000 |
| Hepatitis B | 254 million chronic cases | Western Pacific (6.2%), Africa (6.1%) | ~820,000 |
| Hepatitis C | 50 million chronic cases | Eastern Mediterranean, Europe | ~400,000 |
| Hepatitis D | ~15 million (always with HBV) | Mediterranean Basin, Middle East, Central Asia | Included in HBV |
| Hepatitis E | 20 million infections annually | South Asia, Central Asia, East Africa | ~44,000 |
Risk Factors and Transmission Patterns
The epidemiology of viral hepatitis is closely linked to its transmission routes, which vary by hepatitis type:
- Fecal-oral route: Primary transmission mode for HAV and HEV, associated with poor sanitation and contaminated water
- Parenteral route: Primary transmission mode for HBV, HCV, and HDV through blood and body fluids
- Sexual transmission: Significant for HBV, possible but less efficient for HCV
- Vertical transmission: Mother-to-child transmission of HBV and HCV during pregnancy or childbirth
Mnemonic: “PAST” Risk Groups for Viral Hepatitis
- P – People who inject drugs
- A – At-risk sexual behaviors
- S – Settings with poor sanitation
- T – Transfusion recipients (before screening)
From a community health nursing perspective, understanding these epidemiological patterns is critical for targeting prevention efforts, identifying high-risk populations for screening, and allocating resources for viral hepatitis treatment in community settings.
3. Types of Viral Hepatitis
The 20th century unveiled the mystery of the etiology of viral hepatitis, with the identification of five main viral agents responsible for these infections. Each type has distinct characteristics, transmission routes, and implications for community-based management.
3.1 Hepatitis A (HAV)
Key Characteristics
- Virus type: Single-stranded RNA virus (Picornaviridae family)
- Transmission: Fecal-oral route through contaminated food/water
- Incubation period: 15-50 days (average 28 days)
- Chronic infection: No chronic state
- Severity: Usually self-limiting, rarely severe
Clinical Presentation
- Often asymptomatic in children
- Acute illness with jaundice, nausea, fatigue in adults
- Symptoms typically resolve within 2 months
Community Health Implications
- Outbreaks common in areas with poor sanitation
- Food handlers can be sources of outbreaks
- Preventable through improved sanitation and vaccination
3.2 Hepatitis B (HBV)
Key Characteristics
- Virus type: DNA virus (Hepadnaviridae family)
- Transmission: Blood, bodily fluids, sexual contact, mother-to-child
- Incubation period: 45-160 days (average 120 days)
- Chronic infection: Can become chronic (90% in infants, 5-10% in adults)
- Severity: Can lead to cirrhosis and hepatocellular carcinoma
Clinical Presentation
- Often asymptomatic in acute phase
- When symptomatic: jaundice, fatigue, abdominal pain
- Chronic infection may be silent for decades
Community Health Implications
- Major public health concern due to chronicity
- Universal vaccination highly effective
- Screening of pregnant women critical
3.3 Hepatitis C (HCV)
Key Characteristics
- Virus type: RNA virus (Flaviviridae family)
- Transmission: Blood-to-blood contact, less commonly sexual or perinatal
- Incubation period: 14-84 days (average 45 days)
- Chronic infection: 50-80% develop chronic infection
- Severity: Leading cause of liver transplantation
Clinical Presentation
- Often asymptomatic in acute phase (80%)
- Insidious progression to chronic liver disease
- Extrahepatic manifestations common
Community Health Implications
- Screening of high-risk populations essential
- New direct-acting antivirals offer cure rates >95%
- Treatment as prevention approach
3.4 Hepatitis D (HDV)
Key Characteristics
- Virus type: Defective RNA virus (requires HBV for replication)
- Transmission: Similar to HBV (blood and body fluids)
- Incubation period: 30-180 days
- Chronic infection: Can cause chronic infection with HBV
- Severity: Most severe form of viral hepatitis
Clinical Presentation
- Co-infection or superinfection with HBV
- More severe manifestations than HBV alone
- Accelerated progression to cirrhosis
Community Health Implications
- Prevention focuses on HBV vaccination
- Limited treatment options
- Higher prevalence in specific geographical regions
3.5 Hepatitis E (HEV)
Key Characteristics
- Virus type: RNA virus (Hepeviridae family)
- Transmission: Fecal-oral, zoonotic in some regions
- Incubation period: 15-60 days (average 40 days)
- Chronic infection: Rare, except in immunocompromised
- Severity: Usually self-limiting; high mortality in pregnant women
Clinical Presentation
- Similar to HAV, but can be more severe
- Particularly dangerous for pregnant women (mortality 20-25%)
- More common in adults than children
Community Health Implications
- Major public health concern during waterborne outbreaks
- Prevention through improved water safety
- Special attention to pregnant women
Mnemonic: “ABCDE” of Viral Hepatitis Transmission
- A – Alimentary (Fecal-oral route)
- B – Blood, Body fluids, Birth
- C – Contaminated needles, blood Contact
- D – Depends on B (always with HBV)
- E – Enteric (Fecal-oral route)
4. Prevention & Control Measures
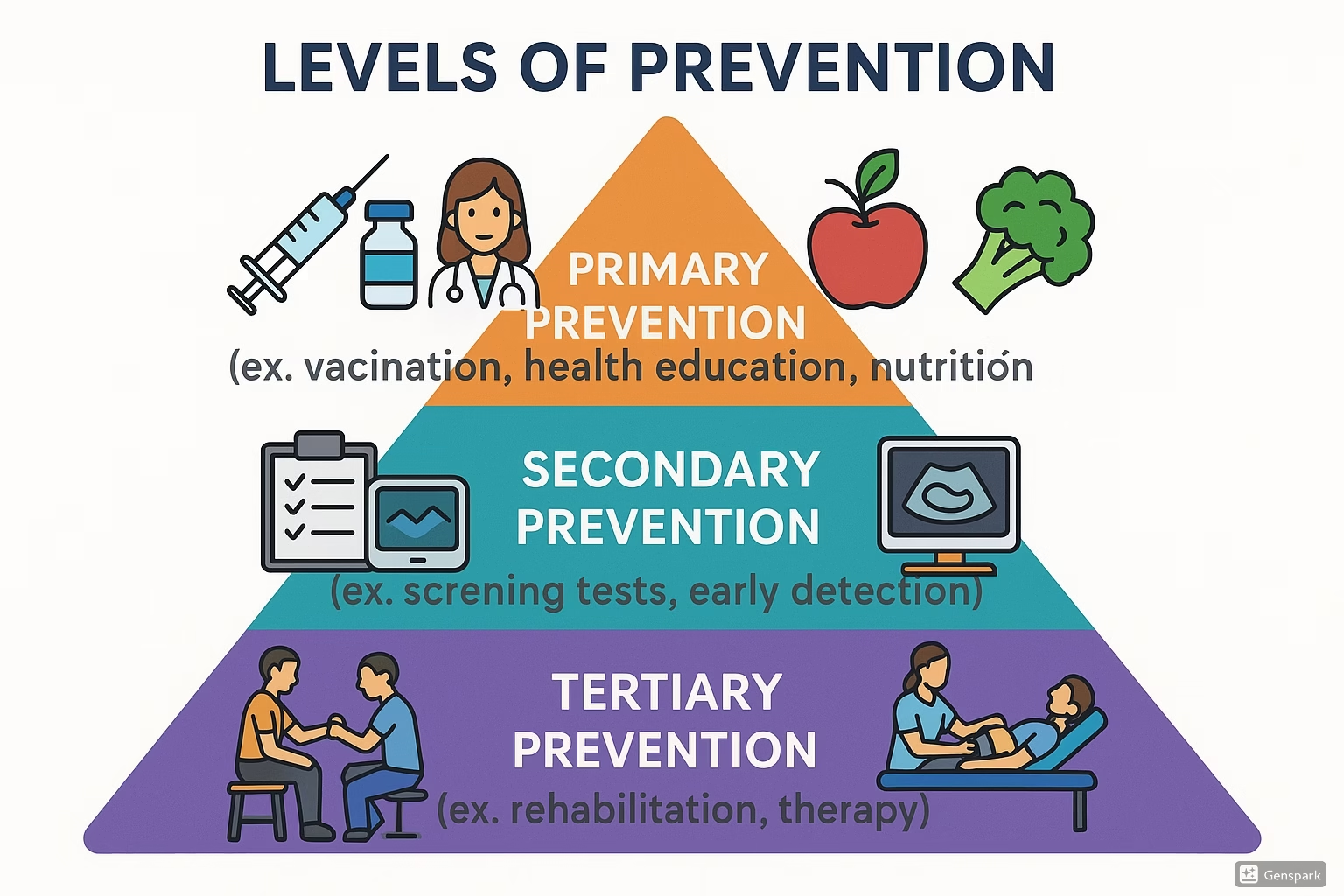
Prevention is a cornerstone of community-based approaches to viral hepatitis management. Community health nurses play a vital role in implementing prevention strategies at primary, secondary, and tertiary levels.
4.1 Primary Prevention
Primary prevention aims to prevent disease before it occurs by reducing exposure to risk factors and enhancing immunity.
Vaccination
- Hepatitis A: Two-dose vaccine series, recommended for:
- All children aged 12-23 months
- Travelers to endemic areas
- Men who have sex with men
- People with chronic liver disease
- Hepatitis B: Three-dose vaccine series, recommended for:
- All infants at birth
- All children and adolescents younger than 19 years
- Adults at risk for HBV infection
- Hepatitis E: Licensed in China but not widely available globally
- Hepatitis C and D: No vaccines currently available
Community Nursing Tip
Maintain a community vaccination registry to track completion rates for multi-dose hepatitis vaccines. Implement reminder systems using text messages or calls to improve completion of vaccine series for viral hepatitis treatment in community settings.
Sanitation and Hygiene
- Safe water supplies and improved sanitation to prevent HAV and HEV
- Food safety education and handwashing promotion
- Community education campaigns about proper hygiene practices
Blood Safety
- Universal screening of donated blood products
- Use of sterile equipment in healthcare settings
- Implementation of standard precautions
Harm Reduction Programs
- Needle and syringe exchange programs
- Opioid substitution therapy
- Education on safer injection practices
4.2 Secondary Prevention
Secondary prevention aims to detect and address disease in its earliest stages before symptoms appear.
Screening and Early Detection
- Risk-based and universal screening approaches
- Community screening events targeting high-risk populations
- Linkage to care for those with positive results
Post-Exposure Prophylaxis
- Hepatitis A: HAV vaccine and/or immunoglobulin within 2 weeks of exposure
- Hepatitis B: HBV vaccine and/or hepatitis B immune globulin (HBIG)
Contact Tracing
- Identification of potentially exposed individuals
- Testing and vaccination of contacts
- Education on preventing further transmission
4.3 Tertiary Prevention
Tertiary prevention focuses on managing disease to slow its progression and prevent complications.
Treatment as Prevention
- Antiviral therapy to reduce viral load and prevent transmission
- Treatment of chronic HBV to prevent progression to cirrhosis and hepatocellular carcinoma
- HCV cure to prevent liver-related morbidity and mortality
Lifestyle Modifications
- Alcohol avoidance for patients with viral hepatitis
- Nutritional counseling and support
- Regular exercise appropriate to condition
Monitoring and Management of Complications
- Regular liver function tests
- Ultrasound surveillance for hepatocellular carcinoma
- Management of portal hypertension and other complications
Prevention Priority Areas
Community health nurses should prioritize prevention efforts based on local epidemiology of viral hepatitis. In communities with high HAV and HEV prevalence, focus on water safety and sanitation. In areas with high HBV and HCV rates, emphasize blood safety, harm reduction, and vaccination.
Community Nurse’s Role in Prevention
Community health nurses serve as frontline workers in implementing prevention strategies for viral hepatitis treatment in community settings:
- Education: Providing information about transmission, risk factors, and prevention methods
- Vaccination: Administering vaccines and tracking completion of series
- Outreach: Engaging marginalized populations at higher risk
- Advocacy: Supporting policies that enhance prevention efforts
- Coordination: Collaborating with public health agencies and community organizations
5. Screening and Diagnosis
Effective screening and diagnosis are crucial components of viral hepatitis treatment in community settings. Community health nurses play a key role in implementing screening programs and ensuring appropriate diagnostic follow-up.
5.1 Screening Tests
Screening involves testing for viral hepatitis in asymptomatic individuals to identify infection before symptoms develop. Different approaches are used for different hepatitis viruses:
Hepatitis A Screening
- Not routinely recommended for the general population
- May be indicated for outbreak investigation
- Test: Anti-HAV IgM and total antibodies
Hepatitis B Screening
- Recommended for:
- All pregnant women
- People born in regions with HBV prevalence ≥2%
- Men who have sex with men
- People who inject drugs
- People with HIV
- Household contacts of HBV-infected individuals
- All adults aged 18 and older at least once
- Tests: HBsAg, anti-HBs, anti-HBc (triple panel)
Hepatitis C Screening
- Recommended for:
- All adults aged 18-79 years, at least once
- All pregnant women during each pregnancy
- People who have ever injected drugs
- People with HIV
- Recipients of blood transfusions before 1992
- Children born to HCV-positive mothers
- Tests: Anti-HCV antibody, followed by HCV RNA if positive
Hepatitis D Screening
- Only for those with confirmed HBV infection
- Test: Anti-HDV antibody
Hepatitis E Screening
- Not routinely recommended
- May be indicated in outbreak situations or unexplained hepatitis
- Test: Anti-HEV IgM and IgG
| Hepatitis Type | Primary Screening Test | Interpretation of Positive Result | Follow-up Test |
|---|---|---|---|
| Hepatitis A | Anti-HAV IgM | Acute infection | Liver function tests |
| Hepatitis B | HBsAg | Active infection (acute or chronic) | HBeAg, anti-HBe, HBV DNA |
| Hepatitis C | Anti-HCV | Past or current infection | HCV RNA, genotype |
| Hepatitis D | Anti-HDV | HDV infection in HBV+ person | HDV RNA |
| Hepatitis E | Anti-HEV IgM | Recent infection | HEV RNA |
5.2 Diagnostic Tests
When screening tests indicate possible infection, diagnostic tests are used to confirm diagnosis, assess severity, and guide treatment decisions:
Serological Tests
- HBV markers: HBsAg, anti-HBs, anti-HBc (IgM and total), HBeAg, anti-HBe
- HCV markers: Anti-HCV antibody, HCV core antigen
- HAV markers: Anti-HAV IgM (acute), Anti-HAV IgG (past infection/immunity)
- HDV markers: Anti-HDV (total and IgM)
- HEV markers: Anti-HEV IgM and IgG
Molecular Tests
- HBV DNA: Measures viral load, guides treatment decisions
- HCV RNA: Confirms active infection, monitors treatment response
- HCV genotyping: Determines HCV genotype (important for treatment decisions)
- HDV RNA: Confirms active HDV replication
Liver Function Tests
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Alkaline phosphatase (ALP)
- Gamma-glutamyl transferase (GGT)
- Bilirubin (total and direct)
- Albumin
- Prothrombin time (PT) / International Normalized Ratio (INR)
Liver Assessment
- Non-invasive tests: FibroScan (transient elastography), FibroTest, APRI score, FIB-4 index
- Imaging studies: Ultrasound, CT scan, MRI
- Liver biopsy: Gold standard but invasive; less commonly performed with improvements in non-invasive assessment
5.3 Community Screening Programs
Community-based screening programs are essential components of viral hepatitis treatment in community settings. They help identify cases that might otherwise go undetected and facilitate linkage to care.
Approaches to Community Screening
- Targeted screening: Focusing on high-risk populations
- Opportunistic screening: During routine healthcare visits
- Integrated screening: Combined with screening for other conditions (e.g., HIV)
- Mobile outreach: Taking screening services to underserved communities
- Community events: Health fairs, awareness campaigns
Community Health Nurse’s Role in Screening
- Conducting risk assessments
- Collecting specimens for testing
- Providing pre- and post-test counseling
- Ensuring appropriate follow-up for positive results
- Managing screening events
- Educating community members about screening importance
Community Nursing Tip
When conducting community hepatitis screening, always have a clear plan for how positive results will be communicated and what referral pathways are available. Ensure privacy during screening and confidentiality of results to reduce stigma associated with viral hepatitis treatment in community settings.
Mnemonic: “SCREEN” for Viral Hepatitis
- S – Serological markers appropriate for virus type
- C – Counsel before and after testing
- R – Risk assessment to guide testing
- E – Ensure confidentiality and privacy
- E – Educate about meaning of results
- N – Navigate positive patients to care
6. Primary Management
Primary management of viral hepatitis in community settings involves a range of interventions aimed at supporting the patient, managing symptoms, preventing disease progression, and, when possible, achieving viral clearance.
6.1 Acute Hepatitis Management
Management of acute viral hepatitis focuses primarily on supportive care while the immune system clears the infection:
Supportive Care
- Rest: Reducing physical activity during the acute phase
- Hydration: Ensuring adequate fluid intake
- Nutrition: Balanced diet with adequate protein and calories
- Symptom management: Addressing nausea, vomiting, abdominal pain
- Monitoring: Regular assessment of liver function
Medication Considerations
- Avoiding hepatotoxic medications
- Adjusting doses of medications cleared by the liver
- Cautious use of acetaminophen (limited to <2g/day if necessary)
- Absolute avoidance of alcohol
Patient Education
- Information about disease course and expected recovery
- Guidance on preventing transmission to household contacts
- Recognition of warning signs requiring medical attention
- Importance of follow-up testing
6.2 Chronic Hepatitis Management
Management of chronic viral hepatitis (primarily HBV and HCV) requires long-term monitoring and often antiviral therapy:
General Management Principles
- Regular monitoring: Liver function tests, viral load, ultrasound surveillance
- Lifestyle modifications: Alcohol avoidance, healthy diet, regular exercise
- Vaccination: HAV and HBV vaccines for non-immune patients with other forms of viral hepatitis
- Mental health support: Addressing psychological impact of chronic disease
Decision-Making for Treatment
- Assessment of disease activity and stage of fibrosis
- Evaluation of comorbidities and contraindications
- Discussion of treatment benefits, risks, and alternatives
- Consideration of patient preferences and barriers to adherence
Monitoring During Treatment
- Adherence assessment and support
- Monitoring for side effects
- Laboratory monitoring according to treatment protocols
- Viral load monitoring to assess treatment response
Warning Signs Requiring Urgent Attention
- Mental status changes (confusion, drowsiness)
- Severe abdominal pain or distention
- Significant bleeding (gums, nose, easy bruising)
- High fever
- Worsening jaundice
These may indicate fulminant hepatitis or acute liver failure requiring immediate hospitalization.
6.3 Type-Specific Treatments
Treatment approaches vary significantly based on the type of viral hepatitis:
Hepatitis A
- No specific antiviral treatment
- Supportive care only
- Most patients recover completely without specific treatment
- Rare severe cases may require hospitalization
Hepatitis B
- Acute HBV: Rarely requires treatment, supportive care
- Chronic HBV: Treatment indicated based on:
- HBV DNA levels
- ALT elevation
- Liver fibrosis stage
- Age and family history
- First-line treatments:
- Entecavir
- Tenofovir disoproxil fumarate
- Tenofovir alafenamide
- Treatment typically long-term/indefinite
Hepatitis C
- Direct-acting antivirals (DAAs): Highly effective (>95% cure rates)
- Treatment duration: Typically 8-12 weeks
- Regimen selection: Based on HCV genotype, prior treatment, and cirrhosis status
- Common regimens:
- Glecaprevir/pibrentasvir
- Sofosbuvir/velpatasvir
- Sofosbuvir/velpatasvir/voxilaprevir
- Goal: Sustained virological response (SVR)
Hepatitis D
- Limited treatment options
- Pegylated interferon alpha for 48 weeks
- Newer agent: Bulevirtide (approved in Europe)
- Control of underlying HBV infection
Hepatitis E
- Acute HEV: Usually self-limiting, supportive care
- Chronic HEV: (in immunosuppressed)
- Reduction of immunosuppression if possible
- Ribavirin for persistent cases
- Special attention to pregnant women (higher mortality)
| Hepatitis Type | Acute Management | Chronic Management | Treatment Success |
|---|---|---|---|
| Hepatitis A | Supportive care only | N/A (no chronic infection) | Complete recovery in most cases |
| Hepatitis B | Supportive care | Entecavir, Tenofovir (long-term) | Viral suppression in >90% |
| Hepatitis C | Usually not treated (unless severe) | Direct-acting antivirals (8-12 weeks) | Cure (SVR) in >95% |
| Hepatitis D | Supportive care | Pegylated interferon, Bulevirtide | Limited success (25-40%) |
| Hepatitis E | Supportive care | Ribavirin (for chronic in immunosuppressed) | >80% in immunocompetent |
Mnemonic: “LIVER” Care for Hepatitis Patients
- L – Lifestyle modifications (avoid alcohol, balanced diet)
- I – Infection prevention (prevent transmission)
- V – Viral load monitoring
- E – Evaluate for complications regularly
- R – Rest and regular follow-up
7. Referral Guidelines
Clear referral guidelines are essential for viral hepatitis treatment in community settings. Community health nurses must know when and how to refer patients for specialized care.
Indications for Referral to Specialist Care
- Acute hepatitis:
- Signs of severe illness or liver failure
- Persistent symptoms beyond expected duration
- Significant comorbidities complicating management
- Pregnancy
- Chronic hepatitis:
- All newly diagnosed cases for initial evaluation
- Evidence of advanced liver disease or cirrhosis
- Consideration for antiviral therapy
- Treatment failure or adverse reactions
- Coinfection with multiple hepatitis viruses or HIV
- Special populations:
- Pregnant women
- Children and adolescents
- Immunocompromised patients
- Patients with renal impairment
- Patients with extrahepatic manifestations
Referral Process
- Documentation: Prepare comprehensive referral including:
- Detailed history
- Physical examination findings
- Laboratory and imaging results
- Current medications
- Psychosocial factors affecting care
- Communication: Clear communication with specialist about:
- Reason for referral
- Urgency of evaluation
- Specific questions to be addressed
- Patient preparation:
- Explain reason for referral
- Address concerns and expectations
- Provide logistical information
- Ensure understanding of next steps
- Follow-up:
- Confirm that appointment was kept
- Obtain specialist recommendations
- Implement care plan collaboratively
Types of Specialists for Referral
- Hepatologist: Specialist in liver diseases
- Gastroenterologist: Specialist in digestive system disorders
- Infectious Disease Specialist: Expert in infectious diseases including viral hepatitis
- Transplant Hepatologist: For patients with end-stage liver disease who may need transplantation
Urgent Referral Warning Signs
Immediate referral to emergency services is necessary for patients with:
- Signs of hepatic encephalopathy (confusion, drowsiness)
- Severe coagulopathy (INR >1.5)
- Ascites with signs of infection
- Variceal bleeding
- Acute abdominal pain with fever
Role of Community Health Nurse in Referral Process
Community health nurses play a critical role in ensuring effective referrals for viral hepatitis treatment in community settings:
- Identifying patients who need specialist care
- Preparing complete referral documentation
- Educating patients about the referral purpose and process
- Addressing barriers to accessing specialist care (transportation, costs, etc.)
- Following up to ensure continuity of care
- Serving as a liaison between patient and specialist
8. Follow-up Care
Effective follow-up care is crucial for viral hepatitis treatment in community settings. It ensures ongoing monitoring, adherence to treatment, and prevention of complications.
Follow-up for Acute Viral Hepatitis
- HAV and HEV:
- Monitor liver function tests until normalization
- Typical follow-up: 2-4 weeks after diagnosis, then as needed
- Confirm resolution of infection in 3-6 months
- Acute HBV:
- Monitor for clearance vs. progression to chronic infection
- Follow-up at 1, 3, and 6 months after diagnosis
- Test for HBsAg at 6 months to confirm clearance
- Acute HCV:
- HCV RNA testing at 6 months to assess for spontaneous clearance
- If virus persists, evaluate for treatment
Follow-up for Chronic Viral Hepatitis
Chronic HBV
- Without treatment (inactive carriers):
- ALT every 6-12 months
- HBV DNA annually
- Liver ultrasound every 6-12 months for cirrhosis/HCC surveillance
- Assessment for treatment indications periodically
- On treatment:
- ALT, HBV DNA, adherence assessment every 3-6 months
- Renal function monitoring (for tenofovir)
- HCC surveillance every 6 months if cirrhotic or high risk
Chronic HCV
- During treatment:
- Monitoring schedule depends on regimen
- Typically includes CBC, liver and renal function tests
- Adherence assessment at each visit
- Side effect management
- After treatment:
- HCV RNA 12 weeks post-treatment to confirm SVR
- If SVR achieved and no advanced fibrosis: discharge from specialist care
- If cirrhosis present: continue HCC surveillance every 6 months
Post-Treatment Monitoring
- HBV: Lifelong monitoring typically needed
- HCV: After SVR confirmed:
- No cirrhosis: routine care, no special monitoring
- Advanced fibrosis/cirrhosis: continued surveillance for HCC
- Risk of reinfection: annual HCV RNA for high-risk patients
Community Health Nurse’s Role in Follow-up
Community health nurses are instrumental in ensuring effective follow-up for viral hepatitis treatment in community settings:
- Monitoring adherence: Assessing and supporting medication adherence
- Appointment reminders: Ensuring patients attend scheduled follow-up visits
- Laboratory coordination: Arranging and tracking necessary tests
- Assessment: Monitoring for complications and treatment side effects
- Education: Reinforcing health education at each contact
- Support: Providing psychosocial support throughout treatment journey
- Care coordination: Ensuring communication between providers
Follow-up Best Practice
Develop a standardized follow-up schedule for each hepatitis type and treatment regimen. Use a tracking system to identify patients who miss appointments, and implement a graduated outreach approach (phone call, text message, home visit) to re-engage patients who drop out of care.
9. Community Nursing Role
Community health nurses play a pivotal role in all aspects of viral hepatitis treatment in community settings. Their multifaceted role encompasses prevention, case-finding, care delivery, and system navigation.
Key Responsibilities
Prevention and Health Promotion
- Educating communities about viral hepatitis transmission and prevention
- Advocating for and administering hepatitis A and B vaccines
- Conducting outreach to high-risk populations
- Promoting harm reduction strategies for people who inject drugs
- Educating about safe sex practices to prevent HBV transmission
Screening and Case Finding
- Conducting risk assessments to identify candidates for screening
- Performing hepatitis screening tests in community settings
- Providing pre- and post-test counseling
- Notifying and testing contacts of infected individuals
- Participating in outbreak investigations
Patient Education and Counseling
- Providing information about disease process, prognosis, and treatment
- Educating about lifestyle modifications to support liver health
- Teaching medication management and side effect monitoring
- Addressing concerns about disease transmission
- Providing guidance on disclosure to partners/family
Care Coordination and Case Management
- Serving as liaison between patients and healthcare providers
- Coordinating appointments and follow-up testing
- Facilitating referrals to specialists and support services
- Advocating for patient needs within healthcare system
- Addressing social determinants affecting care (housing, transportation, etc.)
Direct Patient Care
- Monitoring vital signs and symptoms
- Assessing liver function through physical assessment
- Administering prescribed medications
- Managing complications of advanced liver disease
- Providing palliative care for end-stage disease
Supportive Care
- Addressing psychological impact of diagnosis
- Supporting patients dealing with stigma
- Connecting patients to support groups
- Helping patients navigate insurance and assistance programs
- Providing holistic, person-centered care
Care Models for Community-Based Hepatitis Management
Several models have proven effective for viral hepatitis treatment in community settings:
Nurse-Led Models
- Primary care integration: Nurses manage hepatitis care within primary care settings
- Community health center models: Specialized nurses provide comprehensive hepatitis services
- Mobile outreach: Nurses deliver screening and treatment in community locations
Task-Shifting Models
- Nurses taking on expanded roles in hepatitis management
- Nurse-initiated treatment under physician supervision
- Nurse-led monitoring of patients on treatment
Telehealth Models
- Remote consultation between community nurses and specialists
- Virtual monitoring of patients on treatment
- Tele-education for patients and providers
Community Nursing in Action
The nurse’s role extends beyond clinical care to include advocacy at community and policy levels. Community health nurses can champion improved access to hepatitis testing and treatment, reduction of stigma, and development of supportive policies for viral hepatitis treatment in community settings.
10. Best Practices Globally
Examining global best practices for viral hepatitis treatment in community settings provides valuable insights that can be adapted to local contexts.
Successful Global Strategies
Micro-elimination Approaches
- Focusing on specific high-prevalence populations or settings
- Examples:
- Iceland’s prison-based HCV testing and treatment program
- Australia’s targeted approach to HCV in people who inject drugs
- Egypt’s national HCV elimination program
- Benefits: More manageable goals, measurable outcomes, targeted resource allocation
Decentralized Care Models
- Moving hepatitis care from specialized centers to community settings
- Examples:
- Scotland’s community pharmacy-based HCV treatment
- India’s community health worker approach to HBV screening
- New Zealand’s primary care-based HCV treatment
- Benefits: Increased accessibility, reduced stigma, integration with other services
Simplified Testing and Treatment
- Streamlining diagnostic and treatment pathways
- Examples:
- Georgia’s simplified HCV care cascade
- Cambodia’s same-day HBV testing and treatment initiation
- Rwanda’s integrated HIV/HBV care model
- Benefits: Reduced loss to follow-up, improved treatment completion, cost-effectiveness
Digital Health Solutions
- Leveraging technology to enhance hepatitis care
- Examples:
- China’s mobile application for HBV medication adherence
- Brazil’s telemedicine support for rural hepatitis providers
- South Africa’s SMS reminder system for appointments
- Benefits: Extended reach, improved adherence, enhanced monitoring capabilities
Innovative Community Nursing Programs
Community Outreach and Education
- Australia’s Hepatitis Nurses: Specialized community nurses providing education, screening, and linkage to care
- UK’s BBV (Blood Borne Virus) Champions: Nurse-led program training peer educators in high-risk communities
- Vietnam’s Village Health Worker Program: Integration of hepatitis education into existing community health infrastructure
Treatment Support and Adherence
- Thailand’s DOT (Directly Observed Therapy) for HBV: Community nurses supervising medication adherence
- Canada’s Indigenous Health Nursing Model: Culturally appropriate hepatitis care for Indigenous communities
- Spain’s Harm Reduction Nursing Network: Integrated hepatitis care within harm reduction services
Lessons for Implementation
Key lessons from global best practices that can be applied to viral hepatitis treatment in community settings include:
- Integration: Embedding hepatitis services within existing healthcare structures
- Task-shifting: Empowering nurses and community health workers with expanded roles
- Simplification: Creating streamlined, user-friendly care pathways
- Destigmatization: Addressing stigma through normalization and education
- Community engagement: Involving affected communities in program design and implementation
- Data utilization: Using data for continuous quality improvement
- Advocacy: Leveraging success stories to advocate for policy and funding support
Adaptation Tip
When adapting global best practices for local implementation, consider cultural context, healthcare system structure, resource availability, and community needs. Pilot test new approaches before scaling, and involve community stakeholders in the adaptation process.
11. References
- World Health Organization. (2022). Global Hepatitis Report. WHO.
- Centers for Disease Control and Prevention. (2025). Viral Hepatitis Surveillance Report. CDC.
- Sharma, T. (2021). Nursing perspectives of care and cure for Viral Hepatitis. Global Journal of Digestive Diseases.
- World Health Organization. (2024). WHO sounds alarm on viral hepatitis infections claiming 3500 lives each day. WHO.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2023). What Is Viral Hepatitis? NIDDK.
- Centers for Disease Control and Prevention. (2025). Clinical Testing and Diagnosis for Hepatitis B. CDC.
- American Association for the Study of Liver Diseases. (2023). HCV Guidance: Recommendations for Testing, Managing, and Treating Hepatitis C. AASLD.
- European Association for the Study of the Liver. (2024). EASL Clinical Practice Guidelines: Management of hepatitis B virus infection. Journal of Hepatology.
- Centers for Disease Control and Prevention. (2025). Hepatitis A Prevention and Control. CDC.
- National Viral Hepatitis Roundtable. (2024). Community-based approaches to viral hepatitis elimination. NVHR.