Management of Upper Respiratory Infections
A Community Health Nursing Perspective
1. Introduction
Upper respiratory infections (URIs) are among the most common health issues encountered in community health nursing practice. These infections affect the upper respiratory tract, which includes the nose, sinuses, pharynx, larynx, and trachea. As community health nurses, understanding the proper respiratory infection management protocols is essential for providing effective care and preventing complications.
This educational resource provides comprehensive guidance on the assessment, diagnosis, treatment, and referral criteria for common upper respiratory conditions from a community health nursing perspective. The conditions covered include rhinitis, sinusitis, pharyngitis, laryngitis, and tonsillitis.
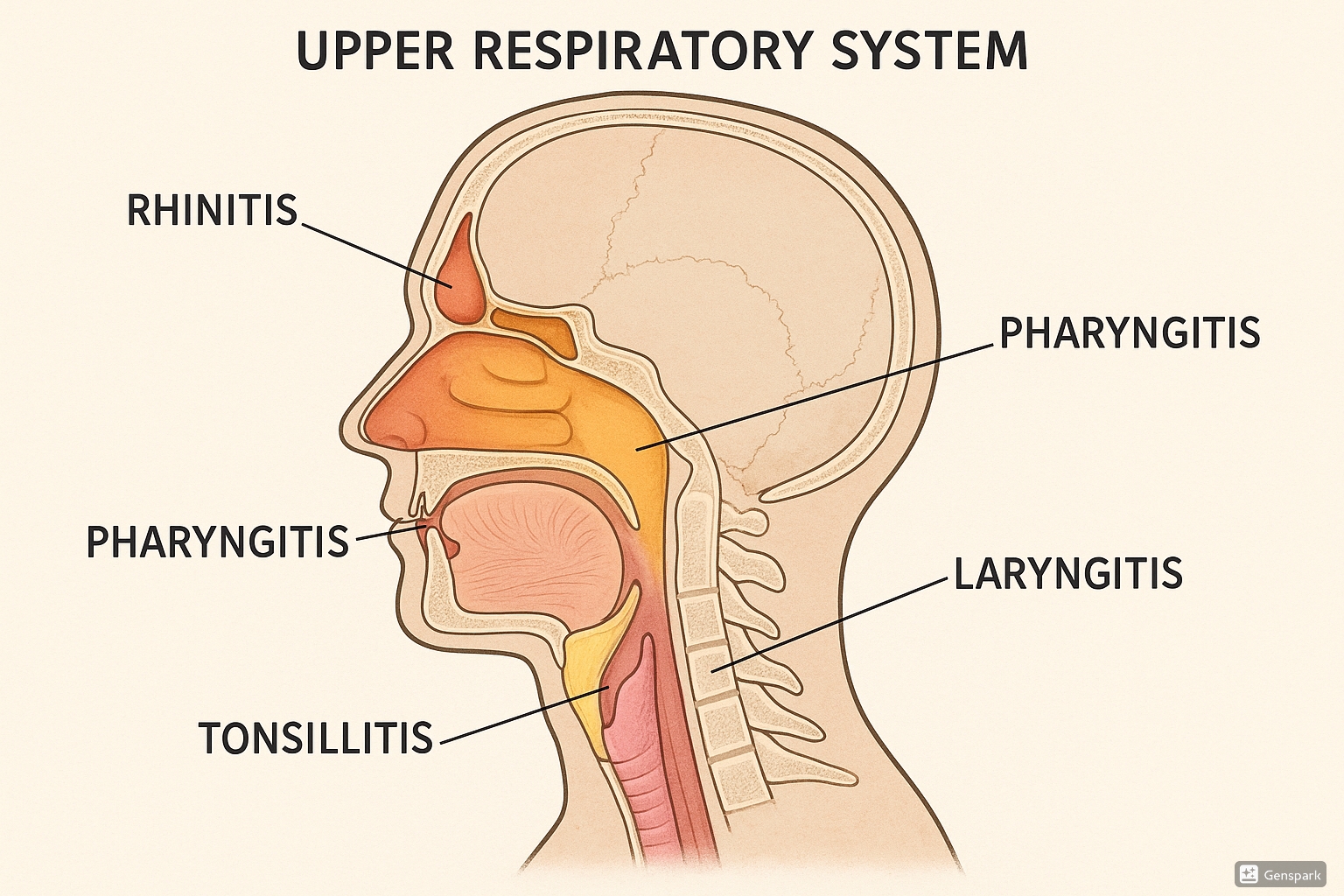
Figure 1: Anatomical representation of the upper respiratory system highlighting the areas affected by different conditions
2. Standing Orders: Definition and Uses
Definition
Standing orders are written medical protocols that authorize healthcare professionals, such as nurses, to carry out specific assessments and interventions without direct physician supervision for certain conditions when specific criteria are met.
Key Components of Standing Orders
In community health nursing practice, standing orders for respiratory infection management typically include:
- Specific criteria that must be met before implementing the standing order
- Clear description of assessments to be performed
- Detailed interventions that may be implemented
- Parameters for when physician consultation or referral is required
- Documentation requirements
Benefits of Standing Orders
Standing orders offer several advantages in community health settings:
- Expedited care for patients with common conditions
- Efficient use of healthcare resources
- Standardization of care based on evidence-based practices
- Expanded scope of practice for nurses in primary care settings
- Improved access to care, especially in underserved areas
Legal Considerations
When implementing standing orders for respiratory infection management, nurses must:
- Ensure the standing orders are signed by an authorized prescriber
- Stay within the scope of practice defined by state nursing boards
- Implement orders exactly as written
- Document all assessments and interventions thoroughly
- Recognize when a situation exceeds the parameters of the standing order
3. Screening and Diagnosis of Upper Respiratory Infections

Figure 2: Flowchart for screening and diagnosis of upper respiratory infections
3.1 Assessment Approach
A systematic approach to respiratory infection management begins with a thorough assessment:
RIPPAS Assessment Framework
A systematic approach to respiratory assessment:
- R Respiratory rate: Count for a full minute
- I Inspection: Observe for signs of respiratory distress
- P Palpation: Check for tenderness, swelling, crepitus
- P Percussion: Assess for abnormal sounds
- A Auscultation: Listen for abnormal breath sounds
- S Saturation: Measure oxygen levels
History Taking
Key elements to include in patient history for suspected upper respiratory infections:
- Onset, duration, and progression of symptoms
- Specific symptoms (congestion, sore throat, cough, fever)
- Exposure to sick contacts
- Previous episodes and treatments
- Vaccination history
- Comorbid conditions (asthma, COPD, immunocompromised status)
- Current medications
- Allergies
3.2 Diagnostic Methods
Several diagnostic methods are available for confirming specific upper respiratory infections:
| Diagnostic Method | Appropriate Conditions | Considerations for Community Settings |
|---|---|---|
| Throat Culture | Pharyngitis, Tonsillitis | Gold standard for bacterial pharyngitis; results take 24-48 hours |
| Rapid Strep Test | Pharyngitis, Tonsillitis | Results in minutes; negative results may require confirmation with culture |
| Nasal/Nasopharyngeal Swabs | Rhinitis, Sinusitis | Useful for viral identification; can be performed in community settings |
| Anterior Rhinoscopy | Rhinitis | Simple procedure to visualize nasal mucosa; requires proper lighting |
| Transillumination | Sinusitis | Simple screening tool for sinusitis; limited accuracy |
| Oxygen Saturation | All respiratory conditions | Quick, non-invasive assessment of respiratory status |
Clinical Pearl
In community settings, diagnosis of upper respiratory infections is often clinical, based on symptom patterns and physical examination findings. Reserve laboratory testing for cases where results would change management decisions, such as suspected bacterial infections that would benefit from antibiotics.
4. Common Upper Respiratory Conditions
Definition
Inflammation of the nasal mucous membranes characterized by nasal congestion, rhinorrhea, sneezing, and nasal itching.
Types
- Allergic Rhinitis: Triggered by allergens like pollen, dust mites, or pet dander
- Non-allergic Rhinitis: Not immune-mediated; triggered by irritants, medications, or hormonal changes
- Infectious Rhinitis: Caused by viral or bacterial infections
Assessment
- Clinical Presentation: Clear watery rhinorrhea, nasal congestion, sneezing, itchy nose/eyes
- Physical Examination: Pale, boggy nasal mucosa; clear discharge; allergic shiners (dark circles under eyes)
Management
Non-pharmacological Interventions:
- Allergen avoidance and environmental control
- Saline nasal irrigation
- Adequate hydration
- Air humidification
Pharmacological Interventions:
- Antihistamines (oral or intranasal)
- Intranasal corticosteroids
- Decongestants (limited use)
- Leukotriene modifiers
- Mast cell stabilizers
Nursing Considerations
- Assess patient’s understanding of proper nasal spray technique
- Monitor for medication side effects
- Educate on environmental control measures
- Provide guidance on symptom management
Teaching Point
When teaching proper nasal spray technique, instruct patients to:
- Gently blow nose to clear nasal passages
- Tilt head slightly forward
- Insert spray tip into nostril, pointing toward the outer eye
- Spray while breathing in gently through the nose
- Repeat in other nostril as prescribed
Definition
Inflammation of the paranasal sinuses, often following a viral upper respiratory infection or allergic rhinitis.
Types
- Acute Sinusitis: Symptoms lasting less than 4 weeks
- Subacute Sinusitis: Symptoms lasting 4-12 weeks
- Chronic Sinusitis: Symptoms lasting more than 12 weeks
- Recurrent Acute Sinusitis: 4 or more episodes per year with complete resolution between episodes
Assessment
- Clinical Presentation: Facial pain/pressure, nasal congestion, purulent nasal discharge, reduced sense of smell
- Physical Examination: Tenderness over involved sinuses, purulent drainage in nasal passages or posterior pharynx
Red Flags
The following symptoms warrant immediate medical attention:
- Severe headache with high fever
- Mental status changes
- Orbital or periorbital swelling/erythema
- Visual changes
- Severe facial swelling
Management
Non-pharmacological Interventions:
- Saline nasal irrigation
- Adequate hydration
- Steam inhalation
- Warm compresses to affected areas
Pharmacological Interventions:
- Analgesics for pain relief
- Intranasal corticosteroids
- Decongestants (short-term use only)
- Antibiotics (only for bacterial sinusitis; typically amoxicillin or amoxicillin-clavulanate for 5-10 days)
Nursing Considerations
- Teach proper technique for nasal irrigation
- Emphasize importance of completing full course of antibiotics if prescribed
- Monitor for improvement or worsening of symptoms
- Educate on prevention of recurrence
Definition
Inflammation of the pharynx (throat) characterized by throat pain, difficulty swallowing, and redness of the pharyngeal walls.
Etiology
- Viral: Most common cause (rhinovirus, adenovirus, coronavirus, influenza)
- Bacterial: Group A Streptococcus (GAS), Mycoplasma, Chlamydia
- Other: Allergies, irritants, postnasal drip, gastroesophageal reflux
CENTOR Criteria for Strep Pharyngitis
Used to assess the likelihood of streptococcal pharyngitis:
- C Cough absence
- E Exudates (tonsillar)
- N Nodes (tender cervical lymph nodes)
- T Temperature (fever >38°C/100.4°F)
- O Onset (age 3-15 years, add point; age >45, subtract point)
- R Risk (score 0-1: 2-6% risk; 2-3: 10-28% risk; ≥4: 38-63% risk)
Assessment
- Clinical Presentation: Sore throat, painful swallowing, fever, malaise, headache
- Physical Examination: Erythematous pharynx, tonsillar exudates, enlarged tender cervical lymph nodes
Management
Non-pharmacological Interventions:
- Warm salt water gargles
- Throat lozenges or hard candy
- Adequate hydration
- Soft, cool foods
- Rest voice if needed
Pharmacological Interventions:
- Viral pharyngitis: Symptomatic treatment with analgesics/antipyretics
- Bacterial pharyngitis: Antibiotics (penicillin, amoxicillin, or macrolides for penicillin-allergic patients)
Nursing Considerations
- Emphasize importance of completing full course of antibiotics if prescribed
- Teach symptomatic management techniques
- Educate about when to return (worsening symptoms, inability to drink fluids)
- Provide guidance on contagious period and return to school/work
Definition
Inflammation of the larynx (voice box) resulting in voice changes, ranging from mild hoarseness to complete voice loss.
Types
- Acute Laryngitis: Typically viral; resolves within 1-2 weeks
- Chronic Laryngitis: Symptoms persisting more than 3 weeks; often due to irritants, voice overuse, or GERD
Assessment
- Clinical Presentation: Hoarseness, voice changes or loss, dry cough, sore throat, sensation of lump in throat
- Physical Examination: Redness and swelling of laryngeal structures (if visible); assessment of breathing status
Warning Signs
The following symptoms may indicate epiglottitis or other serious conditions requiring immediate attention:
- Stridor (high-pitched inspiratory sound)
- Respiratory distress
- Drooling
- Difficulty swallowing
- Sitting forward in “tripod” position
Management
Non-pharmacological Interventions:
- Voice rest (critical component of treatment)
- Adequate hydration
- Humidification of air
- Avoid irritants (smoking, alcohol)
- Steam inhalation
Pharmacological Interventions:
- Analgesics for pain relief
- Antireflux medications if GERD-related
- Rarely, short course of corticosteroids in severe cases
Nursing Considerations
- Emphasize importance of voice rest
- Advise against whispering (can strain vocal cords more than soft speech)
- Teach proper hydration techniques
- Educate about vocal hygiene for prevention
Patient Education
Teach patients the “5 Commandments of Voice Care”:
- Rest your voice when hoarse
- Avoid screaming or shouting
- Stay hydrated (8-10 glasses of water daily)
- Avoid throat clearing and excessive coughing
- Eliminate or reduce smoking and alcohol consumption
Definition
Inflammation of the palatine tonsils, typically due to infection, resulting in sore throat, difficulty swallowing, and visible tonsillar changes.
Types
- Acute Tonsillitis: Sudden onset; resolves within 10-14 days
- Recurrent Tonsillitis: Multiple episodes per year
- Chronic Tonsillitis: Persistent symptoms for extended periods
Etiology
- Viral: Adenovirus, Epstein-Barr virus (mononucleosis), influenza
- Bacterial: Group A Streptococcus (most common bacterial cause), Staphylococcus aureus
Assessment
- Clinical Presentation: Sore throat, painful swallowing, fever, malaise, headache, bad breath
- Physical Examination: Enlarged, erythematous tonsils often with exudate; tender cervical lymphadenopathy
Management
Non-pharmacological Interventions:
- Warm salt water gargles
- Adequate hydration
- Soft, cool foods
- Rest
Pharmacological Interventions:
- Analgesics/antipyretics for pain and fever
- Antibiotics for bacterial tonsillitis (similar to pharyngitis)
Surgical Management: Tonsillectomy may be considered for:
- Recurrent bacterial tonsillitis (typically ≥7 episodes in the past year, ≥5 per year for 2 years, or ≥3 per year for 3 years)
- Peritonsillar abscess
- Airway obstruction due to tonsillar hypertrophy
Nursing Considerations
- Monitor for signs of dehydration
- Teach parents/caregivers about fever management
- Educate about signs of complications (difficulty breathing, drooling, severe difficulty swallowing)
- Provide guidance on return to school/work
5. First Aid and Emergency Management
While most upper respiratory infections are mild and self-limiting, some situations may require emergency intervention. Community health nurses should be proficient in recognizing and responding to respiratory emergencies.
Recognizing Respiratory Emergencies
The following signs and symptoms may indicate a respiratory emergency requiring immediate intervention:
DiapHRaGM Mnemonic for Respiratory Distress
- D Diaphoresis (sweating)
- H Hypoxia (oxygen saturation <92%)
- R Respiratory rate (increased)
- G Gasping (labored breathing)
- M Muscle use (accessory muscle use)
Emergency Response Steps
- Assess: Quickly evaluate airway, breathing, and circulation (ABC)
- Position: Place patient in high Fowler’s position (semi-sitting) if conscious
- Oxygen: Administer oxygen if available and indicated
- Monitor: Check vital signs, including oxygen saturation if possible
- Activate EMS: Call emergency services for signs of severe respiratory distress
Specific Emergency Scenarios
| Emergency Condition | Signs/Symptoms | Immediate Nursing Interventions |
|---|---|---|
| Epiglottitis | Sudden onset of high fever, severe sore throat, drooling, muffled voice, stridor, sitting in “tripod” position |
|
| Severe Croup (Laryngotracheobronchitis) | Barking cough, inspiratory stridor, respiratory distress, retractions |
|
| Anaphylaxis (with respiratory involvement) | Sudden onset of respiratory symptoms, facial/tongue swelling, difficulty breathing, wheezing, often with skin manifestations |
|
| Foreign Body Aspiration | Sudden onset of coughing, choking, wheezing, or respiratory distress |
|
First Aid Kit for Community Health Nurses
Recommended items for respiratory infection management in community settings:
- Pocket mask with one-way valve for rescue breathing
- Pulse oximeter
- Disposable thermometers
- Stethoscope
- Penlight for throat examination
- Tongue depressors
- Disposable gloves
- Surgical masks
- Hand sanitizer
- Emergency contact information
6. Referral Guidelines
As community health nurses, knowing when to refer patients to higher levels of care is essential for effective respiratory infection management. The following guidelines can help determine when referral is appropriate.
General Criteria for Referral
- Severe or persistent symptoms despite appropriate primary care
- Signs of complications
- Diagnostic uncertainty
- Underlying conditions that increase risk (immunocompromised, chronic lung disease)
- Failure to respond to standard therapy
Condition-Specific Referral Criteria
| Condition | Referral Criteria | Level of Referral |
|---|---|---|
| Rhinitis |
|
ENT specialist (non-urgent) |
| Sinusitis |
|
ENT specialist (urgent if complications present) |
| Pharyngitis |
|
Emergency department for severe symptoms/complications; ENT for persistent cases |
| Laryngitis |
|
ENT specialist; emergency department for respiratory distress |
| Tonsillitis |
|
ENT specialist; emergency department for severe cases |
Emergency Referral Indicators
The following findings warrant immediate emergency referral:
- Respiratory distress or significant stridor
- Severe dehydration
- Altered mental status
- Toxic appearance
- Periorbital or orbital cellulitis
- Suspected epiglottitis
- Severe trismus (inability to open mouth)
- Drooling and inability to handle secretions
Effective Referral Communication
When referring patients, provide the following information:
- Clear, concise reason for referral
- Duration and progression of symptoms
- Treatments already attempted and results
- Relevant medical history and risk factors
- Current medications
- Abnormal findings on examination
- Results of any tests performed
- Level of urgency
7. Mnemonics and Learning Aids
Mnemonics can help nursing students remember key concepts in respiratory infection management. Here are several useful mnemonics for upper respiratory conditions:
NOSE for Rhinitis Assessment
- N Nasal congestion and discharge
- O Ocular symptoms (tearing, itching)
- S Sneezing and itching
- E Environmental triggers
SINUS for Sinusitis Symptoms
- S Sinus pain or pressure
- I Inflammation and congestion
- N Nasal discharge (purulent)
- U Unable to smell (hyposmia)
- S Symptoms persist >10 days
THROAT for Pharyngitis Assessment
- T Temperature (fever)
- H Hurts to swallow (odynophagia)
- R Redness of pharynx
- O Onset and duration
- A Adenopathy (swollen lymph nodes)
- T Tonsillar exudates
VOICE for Laryngitis Management
- V Voice rest (essential)
- O Optimal hydration
- I Irritant avoidance
- C Comfort measures (steam, lozenges)
- E Evaluate for underlying causes
Pneumonic for Differentiation of Upper Respiratory Infections
RAPIDS: Clinical Differentiation of Upper Respiratory Conditions
- R Rhinitis: Nasal congestion, clear discharge, sneezing, minimal fever
- A Allergic vs. Infectious: Seasonal pattern, itching, and eye symptoms suggest allergic
- P Pharyngitis: Sore throat, painful swallowing, fever; bacterial if exudates, absent cough
- I Infection location: Which part of the respiratory tract is primarily affected?
- D Duration: Viral typically <10 days; bacterial or complications if longer
- S Sinusitis: Facial pain/pressure, purulent discharge, symptoms >10 days or worsening after 5-7 days
8. Global Best Practices
Around the world, various approaches to respiratory infection management have proven effective. Some notable global best practices include:
Nurse-Led Care Models
- United Kingdom: Nurse practitioners with specialized training manage minor respiratory illnesses through the NHS, reducing the burden on emergency departments and general practitioners.
- Australia: Remote nursing stations use telehealth protocols for respiratory assessment and management in rural areas, with clear referral pathways when needed.
- Canada: Community health nurses implement standardized assessment tools and standing orders for common respiratory conditions in underserved regions.
Antimicrobial Stewardship
- Netherlands: Implements strict guidelines for antibiotic use in respiratory infections, requiring clear evidence of bacterial infection before prescribing.
- Sweden: Uses delayed antibiotic prescribing strategies for respiratory infections, reducing unnecessary antimicrobial use while maintaining patient satisfaction.
- Finland: Conducts national education campaigns for healthcare providers on appropriate antibiotic use for upper respiratory conditions.
Community Education Initiatives
- Singapore: Implements widespread public education on respiratory hygiene and prevention in schools and community centers.
- Thailand: Community health nurses utilize visual education materials for respiratory illness prevention tailored to local cultural contexts.
- New Zealand: Incorporates indigenous health practices alongside modern medicine in community respiratory care models.
Implementing Global Best Practices Locally
To incorporate these global best practices into your community health nursing approach:
- Assess community needs and resources for respiratory infection management
- Adapt evidence-based protocols to your specific healthcare setting
- Develop clear standing orders with physician collaboration
- Implement regular training for assessment skills and current guidelines
- Create culturally appropriate patient education materials
- Establish clear referral pathways for complex cases
- Monitor outcomes and adjust approaches as needed
9. References
- Center for Disease Control and Prevention. (2024). Preventing Transmission of Viral Respiratory Pathogens in Healthcare Settings. https://www.cdc.gov/infection-control/hcp/viral-respiratory-prevention/index.html
- Center for Excellence in Primary Care, UCSF. (2024). Standing Orders. https://cepc.ucsf.edu/standing-orders
- Cleveland Clinic. (2024). Upper Respiratory Infection: Causes, Symptoms & Treatment. https://my.clevelandclinic.org/health/diseases/4022-upper-respiratory-infection
- Cleveland Clinic. (2024). Allergic Rhinitis (Hay Fever): Symptoms & Treatment. https://my.clevelandclinic.org/health/diseases/8622-allergic-rhinitis-hay-fever
- Cleveland Clinic. (2024). Sinus Infection (Sinusitis): Causes, Symptoms & Treatment. https://my.clevelandclinic.org/health/diseases/17701-sinusitis
- Cleveland Clinic. (2024). Laryngitis: Diagnosis, Symptoms, Causes, Treatments & Recovery. https://my.clevelandclinic.org/health/diseases/22268-laryngitis
- Meneghetti, A. (2024). Upper Respiratory Tract Infection Workup. Medscape. https://emedicine.medscape.com/article/302460-workup
- National Center for Biotechnology Information. (2022). Acute Laryngitis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK534871/
- National Center for Biotechnology Information. (2022). Allergic Rhinitis (Nursing). StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK568690/
- National Center for Biotechnology Information. (2022). Acute Sinusitis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK547701/
- Nurseslabs. (2024). Allergic Rhinitis Nursing Care Management. https://nurseslabs.com/allergic-rhinitis/
- Nurseslabs. (2024). Tonsillitis and Adenoiditis Nursing Care Management. https://nurseslabs.com/tonsillitis-adenoiditis/
- Oxford Medical Education. (2024). Respiratory Mnemonics. https://oxfordmedicaleducation.com/medical-mnemonics/respiratory-mnemonics/
- Saketkhoo, K., et al. (2023). Diagnostic techniques for critical respiratory infections. National Center for Biotechnology Information. https://pmc.ncbi.nlm.nih.gov/articles/PMC10432708/
