Intranatal Care: Comprehensive Guide to Normal Labor Process
A Complete Resource for Nursing Students
Introduction to Intranatal Care
Intranatal care encompasses all care provided during the labor and delivery process. For community health nurses, understanding normal labor is essential to provide appropriate care, identify complications early, and support women through this transformative experience. This comprehensive guide explores the normal labor process, monitoring techniques, and management strategies from a community health nursing perspective.
Focus: This guide specifically addresses normal labor processes, providing nursing students with evidence-based knowledge to deliver quality care in various community settings.
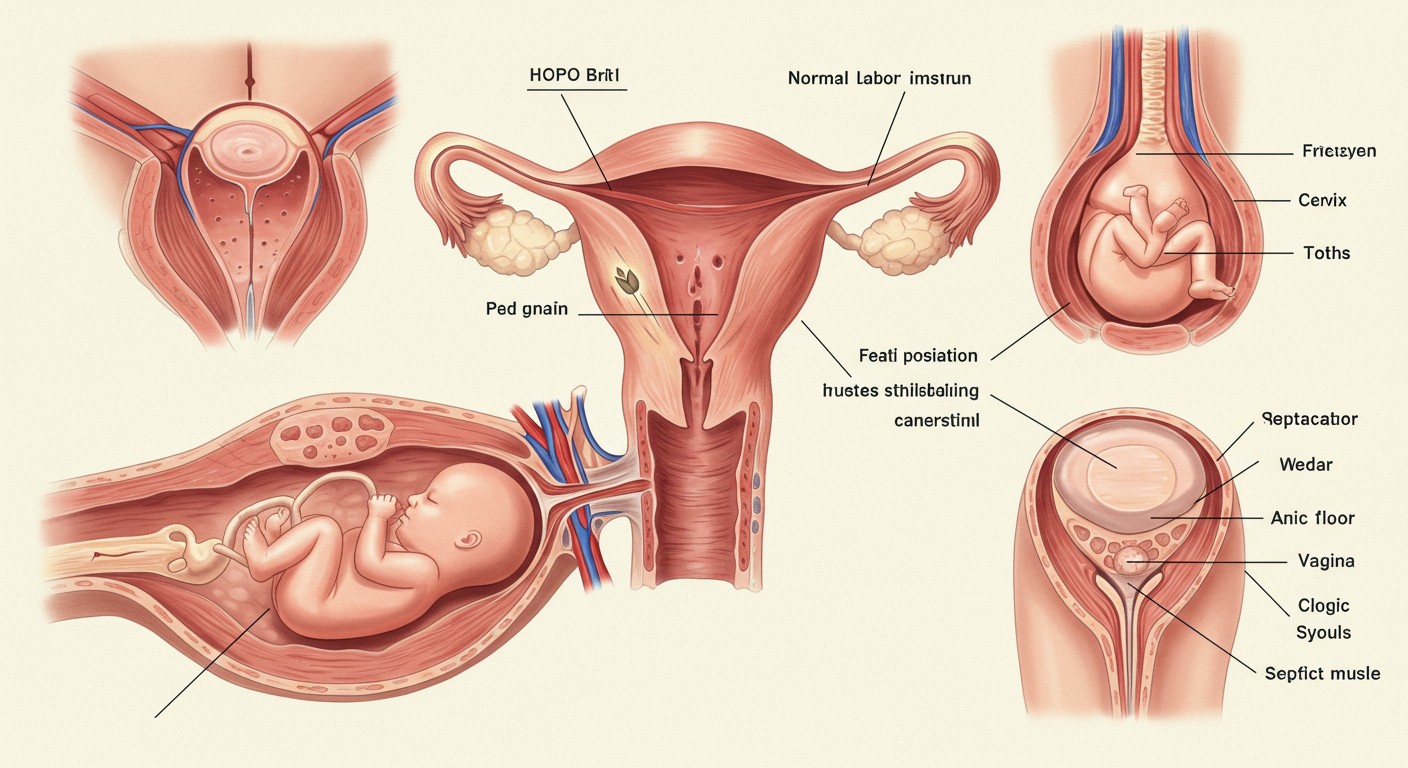
Table of Contents
Normal Labor Process
Labor is defined as the physiological process by which a fetus is expelled from the uterus to the outside world. Normal labor involves regular, progressive contractions that cause cervical effacement and dilation, resulting in the birth of the baby followed by delivery of the placenta.
Characteristics of Normal Labor
| Parameter | Description |
|---|---|
| Spontaneous onset | Labor begins on its own without artificial induction |
| Term pregnancy | Between 37-42 weeks of gestation |
| Single fetus | One baby, not twins or multiples |
| Cephalic presentation | Head-first position |
| Progressive cervical dilation | Cervix dilates at approximately 1cm/hour in active labor |
| Duration | Generally completes within 24 hours |
| Outcome | Birth of a healthy baby with minimal interventions |
Physiology of Labor
The normal labor process is regulated by a complex interplay of mechanical and hormonal factors:
- Hormonal factors: Oxytocin, prostaglandins, estrogen, relaxin, and other hormones
- Mechanical factors: Pressure of the presenting part against the cervix, uterine contractions
- Neurological factors: Ferguson reflex during the second stage of labor
- Psychological factors: Mental preparedness, emotional state, and support system
Onset of Labor
Labor typically begins when the body is physiologically ready. The exact trigger for the onset of labor remains incompletely understood, but several theories exist, including:
- Declining progesterone levels
- Increased estrogen-to-progesterone ratio
- Rising oxytocin levels
- Increased prostaglandin production
- Fetal cortisol production
- Mechanical stretching of the uterus
Signs and Symptoms of Labor Onset
Premonitory Signs (Prodromal Labor)
These signs may occur days or weeks before actual labor begins:
- Lightening: The baby descends into the pelvis, creating more breathing room but increased pressure on the bladder
- Braxton Hicks contractions: Irregular, painless “practice” contractions
- Bloody show: Pinkish or blood-streaked mucus discharge
- Cervical ripening: Softening of the cervix
- Energy burst: Some women experience a sudden energy increase (“nesting instinct”)
- Weight loss: A small weight loss (1-3 pounds) due to fluid shifts and hormonal changes
Definitive Signs of True Labor
| Sign | True Labor | False Labor |
|---|---|---|
| Contraction pattern | Regular, increasing in frequency, duration, and intensity | Irregular, not progressively increasing |
| Contraction location | Start in lower back and radiate to abdomen | Often felt only in abdomen |
| Effect of movement | Continue regardless of activity or position | May decrease with rest or position change |
| Cervical changes | Progressive dilation and effacement | No significant cervical changes |
| Rupture of membranes | May occur before or during labor | Membranes remain intact |
Physiological Changes at the Onset of Labor
As labor begins, several important physiological changes occur:
- Increased myometrial sensitivity to oxytocin due to rising estrogen levels
- Enhanced prostaglandin synthesis promoting cervical ripening
- Cervical remodeling involving changes in collagen structure
- Development of the lower uterine segment and retraction of the upper segment
- Increased sympathetic nervous system activity leading to elevated heart rate and blood pressure
- Changes in maternal glucose metabolism to ensure adequate energy supply
Stages of Labor
The labor process is traditionally divided into four distinct stages, each with unique characteristics and nursing care requirements.
First Stage: Dilation
The first stage of labor is the longest and begins with the onset of regular contractions and ends with complete cervical dilation (10 cm). This stage is further divided into three phases:
| Phase | Cervical Dilation | Duration | Characteristics |
|---|---|---|---|
| Latent Phase | 0-3 cm | 8-12 hours (nulliparous) 5-8 hours (multiparous) |
|
| Active Phase | 4-7 cm | 3-5 hours (nulliparous) 2-4 hours (multiparous) |
|
| Transition Phase | 8-10 cm | 30 min-2 hours |
|
Second Stage: Expulsion
The second stage begins with complete cervical dilation (10 cm) and ends with the birth of the baby.
Key Characteristics:
- Duration: 20 min-2 hours (nulliparous); 5-30 min (multiparous)
- Contractions: Every 2-3 minutes, lasting 60-90 seconds
- Ferguson reflex: Involuntary urge to push due to pressure on pelvic floor
- Descent and rotation: The fetal head descends and rotates through the birth canal
- Cardinal movements: Series of positional changes the fetus makes during descent
Cardinal Movements of Labor
- Engagement: The widest part of the fetal head enters the pelvic inlet
- Descent: The fetal head moves downward through the pelvis
- Flexion: The fetal chin flexes toward the chest to present the smallest diameter
- Internal rotation: The fetal head rotates to align with the pelvic outlet
- Extension: The fetal head extends as it passes under the pubic arch
- External rotation (restitution): The fetal head rotates back to align with shoulders
- Expulsion: Delivery of the shoulders and body
Third Stage: Placental Delivery
The third stage begins after the birth of the baby and ends with the delivery of the placenta.
Key Characteristics:
- Duration: 5-30 minutes
- Contractions: Continue but less intense
- Signs of placental separation:
- Cord lengthening at the vaginal entrance
- Small gush of blood
- Uterus rises in the abdomen and becomes more globular
- Placental delivery mechanisms:
- Schultze mechanism: Fetal side delivers first (more common, 80%)
- Duncan mechanism: Maternal side delivers first (20%)
Fourth Stage: Immediate Postpartum
The fourth stage begins after delivery of the placenta and typically lasts 1-2 hours. This critical period involves stabilization of the mother’s condition.
Key Processes:
- Uterine contraction and hemostasis: The uterus contracts to control bleeding
- Initiation of maternal-infant bonding: Often facilitated by skin-to-skin contact
- Physiological recovery: Vital signs stabilize, shivering may occur
- Initial breastfeeding: Helps with uterine contraction and establishes lactation
Monitoring and Active Management of Labor
Effective monitoring and appropriate management during each stage of labor are essential for ensuring maternal and fetal well-being. Community health nurses play a vital role in providing this care.
Management During First Stage
Maternal Assessment and Monitoring
| Parameter | Frequency | Normal Values |
|---|---|---|
| Vital signs | Every 4 hours (latent phase) Every hour (active phase) |
|
| Uterine contractions | Every 30-60 minutes |
|
| Vaginal examination | Every 4 hours or as clinically indicated |
|
| Hydration and nutrition | Ongoing assessment |
|
| Emotional status | Continuous |
|
Fetal Monitoring
| Method | Frequency | Normal Values |
|---|---|---|
| Intermittent auscultation |
|
|
| Electronic fetal monitoring (if available) | Continuous or intermittent |
|
Supportive Interventions
- Pain management techniques:
- Breathing techniques and relaxation
- Position changes
- Massage and counterpressure
- Hydrotherapy (shower or bath where available)
- Non-pharmacological methods (TENS, heat/cold therapy)
- Hydration and nutrition:
- Encourage oral fluids
- Light, easily digestible foods in early labor
- Emotional support:
- Continuous presence
- Encouragement and reassurance
- Involving birth partner
- Clear communication about progress
Warning Signs During First Stage
- Abnormal fetal heart rate patterns
- Meconium-stained amniotic fluid
- Prolonged labor (>20 hours for nulliparous, >14 hours for multiparous)
- Maternal fever (>38°C)
- Hypertension (>140/90 mmHg)
- Hypotension (<90/60 mmHg)
- Abnormal vaginal bleeding
Management During Second Stage
Monitoring
| Parameter | Frequency | Assessment |
|---|---|---|
| Maternal vital signs | Every 15-30 minutes | Monitor for changes indicating maternal distress |
| Fetal heart rate | Every 5-15 minutes | Monitor between contractions for baseline |
| Contractions | Continuous | Assess frequency, duration, and intensity |
| Fetal descent | Every 15-30 minutes | Observe progress through birth canal |
| Maternal pushing efforts | Continuous | Assess effectiveness and maternal fatigue |
| Perineum | Continuous during crowning | Assess for thinning, bulging, and need for support |
Active Management Techniques
- Pushing guidance:
- Encourage pushing with contractions
- Open-glottis pushing (breathing out while pushing)
- Position changes to facilitate descent
- Optimal positions for birth:
- Upright positions (squatting, kneeling, supported standing)
- Side-lying position
- Hands and knees position
- Perineal support techniques:
- Warm compresses
- Perineal massage
- Controlled delivery of the head
Birth Assistance
During delivery of the baby, the nurse or midwife should:
- Support the perineum during crowning
- Guide the mother to push gently as the head emerges
- Check for nuchal cord (umbilical cord around neck)
- Support the head as it extends
- Guide restitution of the head
- Guide delivery of the anterior, then posterior shoulder
- Support the body as it delivers
Management During Third Stage
Active vs. Expectant Management
| Active Management | Expectant (Physiological) Management |
|---|---|
|
|
| Advantages: Reduced risk of postpartum hemorrhage, shorter third stage | Advantages: More physiological, benefits for infant from delayed cord clamping |
WHO Recommendation
The World Health Organization (WHO) recommends active management of the third stage of labor for all births to reduce the risk of postpartum hemorrhage.
Placental Examination
After delivery, examine the placenta for:
- Completeness: Ensure all cotyledons and lobes are present
- Membrane completeness: Check for tears or missing fragments
- Cord insertion: Central, eccentric, marginal, or velamentous
- Number of vessels in cord: Normally three (two arteries, one vein)
- Abnormalities: Infarcts, calcifications, or other pathologies
Management During Fourth Stage
Immediate Postpartum Assessment and Care
| Assessment | Frequency | Normal Findings |
|---|---|---|
| Vital signs | Every 15 min for first hour, then every 30 min for second hour |
|
| Uterine tone | Every 15 min for first hour, then every 30 min | Firm, contracted uterus at or below umbilicus |
| Lochia (vaginal discharge) | Every 15 min for first hour |
|
| Perineum | Initial assessment and as needed |
|
| Bladder | Every 1-2 hours |
|
Key Interventions
- Promote bonding: Facilitate skin-to-skin contact between mother and baby
- Support breastfeeding initiation: Assist with first feeding within one hour of birth
- Monitor for bleeding: Assess fundal height and firmness, massage if needed
- Comfort measures: Provide warm blankets, clean linens, pain management
- Perineal care: Ice packs, witch hazel pads, sitz baths
- Nutrition and hydration: Offer light meal and fluids
Warning Signs in Fourth Stage
- Heavy vaginal bleeding or large clots
- Boggy, poorly contracted uterus
- Rising pulse or falling blood pressure
- Uterine inversion
- Retained placental fragments
- Inability to void
- Perineal hematoma formation
Care After Labor
Immediate postpartum care extends beyond the fourth stage and continues for the first 24 hours after birth. Community health nurses provide essential services during this critical period.
Physical Recovery Support
| System | Assessment | Interventions |
|---|---|---|
| Cardiovascular |
|
|
| Reproductive |
|
|
| Urinary |
|
|
| Gastrointestinal |
|
|
| Musculoskeletal |
|
|
Lactation Support
- Early initiation: Support breastfeeding within first hour after birth
- Positioning guidance: Ensure proper latch and comfortable positions
- Education: Teach signs of adequate intake and milk transfer
- Address concerns: Provide solutions for common breastfeeding challenges
- Comfort measures: Management of breast engorgement and nipple discomfort
Emotional and Psychological Support
- Process birth experience: Allow mother to discuss labor and delivery
- Normalize emotions: Explain common feelings and mood fluctuations
- Screen for red flags: Be alert for signs of postpartum depression or anxiety
- Family adjustment: Include partners and other family members in care
- Cultural considerations: Respect cultural practices around postpartum period
Discharge Education
BUBBLE-HE Mnemonic for Postpartum Education
- B – Breasts: Care, engorgement, feeding
- U – Uterus: Involution, fundal massage
- B – Bladder: Voiding frequency, retention
- B – Bowels: Constipation prevention
- L – Lochia: Normal patterns and warning signs
- E – Episiotomy/perineum: Care and healing
- H – Hormones: Mood changes and coping
- E – Exercise: Gradual resumption of activities
Warning Signs Review
Educate the mother about warning signs requiring immediate attention:
- Heavy bleeding (soaking a pad in less than an hour)
- Severe pain not relieved by medication
- Fever over 38°C (100.4°F)
- Foul-smelling vaginal discharge
- Severe headache or changes in vision
- Calf pain, redness, or swelling
- Difficulty breathing or chest pain
- Thoughts of harming self or baby
Helpful Mnemonics for Labor Care
5 P’s of Labor
- Powers: Uterine contractions and maternal pushing efforts
- Passenger: The fetus and its presentation, position, and size
- Passage: The birth canal and pelvis
- Position: Maternal position during labor and delivery
- Psyche: Psychological state and preparation of the mother
REEDA Scale for Perineal Healing Assessment
- Redness: Normal healing vs. infection signs
- Edema: Amount of swelling present
- Ecchymosis: Bruising extent and appearance
- Discharge: Type, amount, and odor
- Approximation: Wound edges coming together properly
AWHONN Criteria for Second Stage Labor Progress
- Analysis of contraction pattern
- Witness fetal descent with each push
- Hydration status of the mother
- Outlet assessment (pelvic adequacy)
- Need for maternal rest between contractions
- Normal FHR patterns maintained
VEAL CHOP for Fetal Heart Rate Pattern Assessment
Types of decelerations:
- Variable: Cord compression
- Early: Head compression (normal)
- Acceleration: Normal response
- Late: Uteroplacental insufficiency
- Consistent in shape
- Head compression (early)
- Oxygen insufficiency (late)
- Pressure on cord (variable)
Global Best Practices in Intranatal Care
WHO Recommendations for a Positive Labor Experience
The World Health Organization has developed evidence-based recommendations to ensure positive labor and birth experiences while maintaining safety:
- Respectful maternity care for all women
- Effective communication between caregivers and laboring women
- Companionship during labor and childbirth
- Allowing women to choose their preferred birth positions
- Freedom of movement during labor
- Avoiding routine interventions without clear medical indications
Notable Global Approaches
| Country/Region | Practice | Benefits |
|---|---|---|
| Netherlands | Integration of home births with hospital system | Lower intervention rates, comfortable environment, seamless transfer if needed |
| Sweden | Midwife-led care for low-risk pregnancies | Continuity of care, high maternal satisfaction, lower intervention rates |
| Japan | Satogaeri bunben (returning to parental home for birth and postpartum) | Enhanced family support, traditional knowledge transfer, reduced postpartum depression |
| New Zealand | Community-based midwifery model with continuous care | Strong relationship between woman and midwife, culturally sensitive care |
| Brazil | Birth centers (Casa de Parto) for normal births | Homelike environment, reduced interventions, emphasis on natural birth |
Community Health Nursing Applications
Community health nurses can implement global best practices by:
- Promoting birth preparedness and complication readiness in communities
- Facilitating community support networks for pregnant and postpartum women
- Conducting childbirth education that includes various labor coping strategies
- Advocating for culturally sensitive and respectful maternity care
- Training traditional birth attendants in safe delivery practices where applicable
- Establishing effective referral systems between community settings and higher levels of care
- Implementing postpartum home visit programs
