The Menstrual Cycle: Physiology and Hygiene
Comprehensive Nursing Notes
Introduction
The menstrual cycle is a complex, cyclical process orchestrated by hormonal fluctuations that prepare the female body for potential pregnancy. Understanding the menstrual cycle physiology is fundamental for nursing practice, especially in women’s health, gynecology, fertility counseling, and patient education. These notes provide a comprehensive overview of menstrual cycle physiology and hygiene practices to enhance clinical knowledge and patient care.
Overview of the Menstrual Cycle
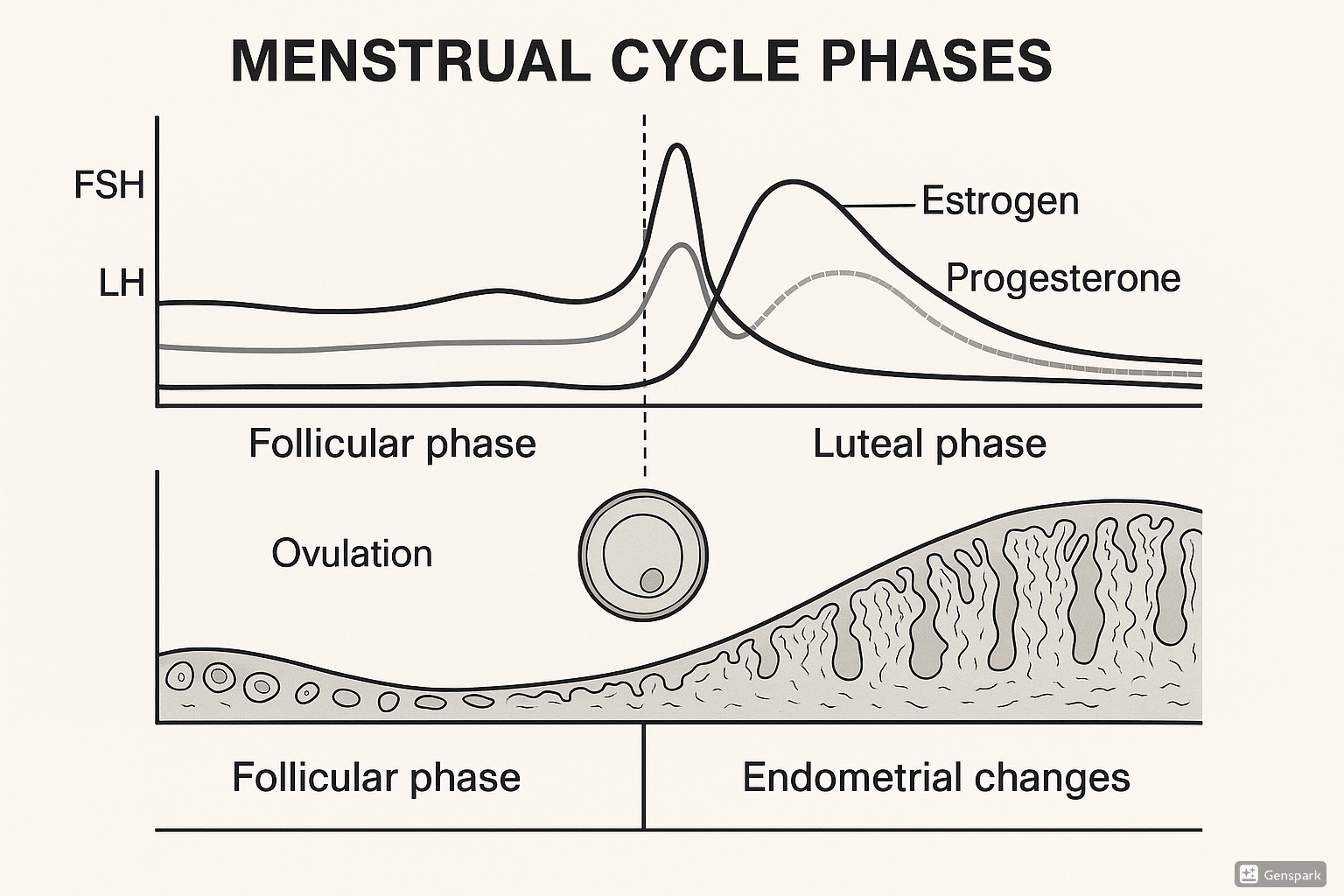
Figure 1: The menstrual cycle showing hormonal fluctuations, ovarian phases, and endometrial changes.
The menstrual cycle is a natural reproductive process occurring in females of reproductive age, typically lasting 28 days on average (though normal cycles can range from 21-35 days). It represents the monthly preparation of the female body for potential pregnancy through coordinated hormonal signals between the hypothalamus, pituitary gland, and ovaries.
Key Components of the Menstrual Cycle:
- Hypothalamic-pituitary-ovarian (HPO) axis coordination
- Ovarian follicular development and ovulation
- Endometrial proliferation and shedding
- Cyclical hormonal fluctuations
The menstrual cycle serves a crucial reproductive function and reflects overall health status. Regular cycles indicate proper hormonal balance and reproductive health, while irregularities may signal underlying health conditions requiring assessment.
Hormonal Regulation
The intricate hormonal regulation of the menstrual cycle involves several key hormones working in synchronized patterns:
| Hormone | Source | Primary Function | Pattern During Cycle |
|---|---|---|---|
| Gonadotropin-Releasing Hormone (GnRH) | Hypothalamus | Stimulates release of FSH and LH | Pulsatile secretion; frequency changes throughout cycle |
| Follicle-Stimulating Hormone (FSH) | Anterior Pituitary | Promotes follicular development | Peaks early in follicular phase |
| Luteinizing Hormone (LH) | Anterior Pituitary | Triggers ovulation; supports corpus luteum | Surges at mid-cycle; slight elevation in luteal phase |
| Estrogen (Estradiol) | Developing Follicles | Promotes endometrial proliferation; triggers LH surge | Low early in cycle; peaks before ovulation; moderate in luteal phase |
| Progesterone | Corpus Luteum | Prepares endometrium for implantation | Low in follicular phase; elevated in luteal phase |
| Inhibin | Developing Follicles/Corpus Luteum | Inhibits FSH secretion | Increases with follicular development; peaks in luteal phase |
| Prostaglandins | Endometrium | Contributes to myometrial contractions | Increases during menstruation |
Feedback Mechanisms:
- Negative Feedback: Rising estrogen and progesterone levels inhibit GnRH, FSH, and LH production during most of the cycle
- Positive Feedback: High estrogen levels at mid-cycle trigger the LH surge that induces ovulation
The delicate balance of these hormones ensures proper follicular development, timely ovulation, and appropriate endometrial preparation. Disruptions in this hormonal orchestra can lead to menstrual irregularities, anovulation, or other reproductive health issues.
Phases of the Menstrual Cycle
The menstrual cycle consists of concurrent ovarian and endometrial cycles that occur in phases. Understanding these phases is essential for interpreting clinical manifestations and providing appropriate patient education.
Ovarian Cycle
1. Follicular Phase (Days 1-13)
- Early Follicular (Days 1-7): FSH stimulates recruitment of 15-20 primordial follicles
- Mid-Follicular (Days 8-10): Selection of dominant follicle; others undergo atresia
- Late Follicular (Days 11-13): Dominant follicle matures, increases estrogen production
- Hormonal Profile: Rising FSH followed by rising estrogen; low progesterone
2. Ovulation (Day 14 ± 2)
- High estrogen triggers LH surge (24-36 hours before ovulation)
- LH surge initiates final follicular maturation and oocyte meiotic division
- Rupture of follicle and release of oocyte into fallopian tube
- Characterized by mid-cycle spotting in some women, mittelschmerz (ovulation pain)
- Hormonal Profile: Peak LH and estrogen levels
3. Luteal Phase (Days 15-28)
- Formation of corpus luteum from ruptured follicle
- Corpus luteum secretes progesterone and estrogen
- If fertilization doesn’t occur, corpus luteum degenerates after 10-12 days
- Declining hormone levels trigger menstruation
- Hormonal Profile: High progesterone, moderate estrogen; both decline if no pregnancy occurs
Endometrial Cycle
1. Menstrual Phase (Days 1-5)
- Shedding of functional layer of endometrium
- Average blood loss: 30-80 mL over 3-7 days
- Characterized by cramping due to prostaglandin-induced myometrial contractions
- Histologically: Tissue debris, red blood cells, inflammatory cells
2. Proliferative Phase (Days 6-14)
- Estrogen-driven regeneration and growth of endometrium
- Endometrial thickness increases from 0.5 mm to 3-5 mm
- Development of endometrial glands and spiral arteries
- Histologically: Straight, narrow glands; compact stroma; mitotic activity
3. Secretory Phase (Days 15-28)
- Progesterone-driven development of secretory endometrium
- Glands become tortuous and secrete glycogen-rich mucus
- Spiral arteries develop further, endometrium becomes edematous
- Maximal preparation for potential implantation
- Histologically: Tortuous glands with secretions; edematous stroma; predecidual changes near vessels
4. Ischemic Phase (Last 24 hours if no pregnancy)
- Vasoconstriction of spiral arteries due to falling progesterone levels
- Endometrial ischemia and focal necrosis
- Precedes menstrual shedding
- Histologically: Predecidual changes, leukocyte infiltration, stromal breakdown
Endometrial Changes
The endometrium undergoes remarkable cyclical changes during the menstrual cycle, preparing for potential implantation of a fertilized ovum. These changes can be assessed clinically through endometrial thickness measurements via ultrasound.
| Phase | Endometrial Thickness | Glandular Characteristics | Vascular Changes |
|---|---|---|---|
| Early Proliferative | 1-2 mm | Straight, narrow glands | Short, straight arteries |
| Late Proliferative | 3-5 mm | Longer, slightly coiled glands | Longer, slightly coiled arteries |
| Early Secretory | 6-8 mm | Subnuclear vacuolation; glycogen accumulation | Further coiling of spiral arteries |
| Mid-Secretory | 7-10 mm | Maximal secretory activity; saw-toothed appearance | Prominent spiral arteries |
| Late Secretory | 5-8 mm | Exhausted secretory activity; predecidual changes | Constriction of spiral arteries |
| Menstrual | 0.5-1 mm | Fragmentation and shedding | Dilation, constriction, extravasation |
Functional Layers of the Endometrium:
- Basalis Layer: Deep layer adjacent to myometrium; remains intact during menstruation; contains stem cells for endometrial regeneration
- Functionalis Layer: Superficial layer that responds to hormonal fluctuations; divided into:
- Stratum compactum: Upper compact layer with dense stromal cells
- Stratum spongiosum: Lower spongy layer with glands and loose stroma
The regenerative capacity of the endometrium is remarkable, with complete renewal occurring approximately 400 times during a woman’s reproductive lifespan. This process requires precise hormonal orchestration and adequate nutritional support, particularly iron, vitamin B12, and folate.
Clinical Significance
Understanding the menstrual cycle has crucial clinical implications for nursing assessment, diagnosis, and patient education:
Assessment Parameters
- Menstrual history (menarche, regularity, duration, flow volume)
- Associated symptoms (pain, mood changes, breast tenderness)
- Last menstrual period (LMP) for pregnancy assessment
- Basal body temperature patterns
- Cervical mucus changes throughout cycle
Fertility Awareness
- Identification of fertile window (typically days 10-17)
- Natural family planning methods
- Symptothermal method combining multiple fertility signs
- Ovulation prediction using LH test kits
- Cervical position and consistency changes
Menstrual Disorders
- Amenorrhea: Absence of menstruation
- Dysmenorrhea: Painful menstruation
- Menorrhagia: Heavy/prolonged bleeding
- Oligomenorrhea: Infrequent periods
- Premenstrual Syndrome (PMS): Physical and emotional symptoms
- Premenstrual Dysphoric Disorder (PMDD): Severe form of PMS
Hormonal Contraception
- Mechanism: Suppression of GnRH pulsatility, prevention of LH surge
- Combined hormonal methods (estrogen + progestin)
- Progestin-only methods
- Effect on endometrial thickness and cervical mucus
- Withdrawal bleeding vs. true menstruation
Red Flags Requiring Further Assessment:
- Sudden changes in menstrual pattern
- Bleeding between periods (intermenstrual bleeding)
- Postmenopausal bleeding
- Excessive bleeding (soaking through pad/tampon hourly)
- Severe pain unrelieved by over-the-counter medications
- Cycles shorter than 21 days or longer than 35 days
Menstrual Hygiene
Menstrual hygiene management (MHM) is a crucial aspect of women’s health that encompasses practices, facilities, and socio-cultural support that enable women and girls to manage their menstruation with dignity and comfort.
Menstrual Products
| Product | Description | Advantages | Disadvantages | Usage Guidelines |
|---|---|---|---|---|
| Disposable Pads | Absorbent material with adhesive backing | Easy to use, widely available, various absorbencies | Environmental impact, potential skin irritation, cost | Change every 4-6 hours; never >8 hours |
| Tampons | Cylindrical absorbent material inserted vaginally | Internal wear, allows swimming, less noticeable | TSS risk, learning curve for insertion | Change every 4-6 hours; never >8 hours |
| Menstrual Cups | Flexible silicone/rubber cup inserted vaginally | Reusable (5-10 years), eco-friendly, cost-effective | Learning curve, initial cost, proper cleaning needed | Empty every 8-12 hours; sterilize between cycles |
| Cloth Pads | Washable fabric pads | Reusable, eco-friendly, customizable | Requires washing, not as absorbent as disposables | Change every 4-6 hours; wash thoroughly with soap |
| Period Underwear | Absorbent underwear designed for menstruation | Comfortable, reusable, discrete | Higher initial cost, limited capacity for heavy flow | Change daily; rinse before washing |
| Menstrual Discs | Flexible disc that sits at vaginal fornix | 12-hour wear, can be worn during intercourse | Insertion learning curve, potential leakage | Empty every 12 hours; disposal or cleaning based on type |
Essential Hygiene Practices
Personal Cleanliness
- Wash genital area with plain water or mild soap daily
- Avoid douching or vaginal washing with harsh products
- Change menstrual products regularly according to flow
- Wash hands before and after changing menstrual products
- Shower or bathe regularly during menstruation
Product Management
- Store unused products in clean, dry place
- Check expiration dates on commercial products
- Dispose of used products properly (not in toilet)
- Wash reusable products thoroughly with mild soap
- Sterilize menstrual cups between cycles (boiling water)
Preventing Infections
- Change products before they become fully saturated
- Avoid leaving tampons in for >8 hours (TSS risk)
- Use appropriate absorbency for flow level
- Monitor for unusual odor, discharge, or irritation
- Seek healthcare advice for persistent symptoms
Pain Management
- NSAIDs for cramp relief (ibuprofen, naproxen)
- Heat therapy with heating pads or warm baths
- Regular physical activity to reduce cramping
- Relaxation techniques for stress reduction
- Adequate hydration and balanced nutrition
Toxic Shock Syndrome (TSS) Awareness
TSS Warning Signs:
- Sudden high fever (>102°F/38.9°C)
- Widespread sunburn-like rash
- Muscle aches and headache
- Vomiting or diarrhea
- Dizziness, confusion, or fainting
- Low blood pressure
- Requires immediate medical attention
Cultural Considerations
Cultural beliefs and practices surrounding menstruation vary widely around the world. As healthcare providers, it’s important to:
- Approach menstrual health discussions with cultural sensitivity
- Recognize diverse religious and cultural practices regarding menstruation
- Address misconceptions while respecting cultural beliefs
- Provide factual information in a culturally appropriate manner
- Support access to menstrual products across socioeconomic backgrounds
Mnemonics for Learning
5 P’s of the Menstrual Cycle Phases
- Period (Menstrual phase)
- Proliferation (Estrogen-dominant phase)
- Peak (Ovulation)
- Progesterone (Luteal phase)
- Premenstrual (Late luteal phase)
FOLLICLES for Follicular Phase Events
- FSH rises
- Ovaries activate follicles
- Lining begins regeneration
- LH starts to increase
- Initial recruitment of follicles
- Competing follicles undergo selection
- Leading follicle becomes dominant
- Estrogen production increases
- Selects one follicle for ovulation
OVUM for Ovulation Indicators
- Oogonia completes first meiotic division
- Viscosity of cervical mucus decreases (more stretchy)
- Uterine contractility increases
- Mittelschmerz (ovulation pain) may occur
MENSES for Menstrual Phase Characteristics
- Myometrial contractions expel endometrium
- Endometrial functional layer sheds
- Neovascularization begins for repair
- Stemming of blood flow by vasoconstriction
- Epithelial regeneration from basal layer
- Surge of FSH begins next cycle
Hormonal Dance Sequence:
“GnRH conducts the orchestra, FSH recruits the performers, Estrogen builds the stage, LH starts the show, Progesterone prepares for the audience, and without pregnancy, the curtain falls to begin again.”
Global Best Practices
Around the world, various organizations, governments, and communities have implemented innovative approaches to menstrual health and hygiene:
Educational Initiatives
- Scotland: First country to make menstrual products free and accessible in public buildings
- New Zealand: Provides free menstrual products in all schools
- Kenya: Implemented comprehensive menstrual health education in school curriculum
- Japan: “Period Leave” policies in workplaces for menstrual discomfort
Sustainable Solutions
- India: Self-help groups manufacturing low-cost reusable pads
- Sweden: Environmental certification for menstrual products
- South Africa: Community washing stations for reusable products
- Australia: “Share the Dignity” initiative providing products to homeless
Healthcare Integration
- Netherlands: Menstrual health screening in routine gynecological care
- Rwanda: Community health workers trained in menstrual health counseling
- Canada: Integration of menstrual health in Indigenous healthcare services
- UK: Specialized menstrual disorder clinics within NHS
Policy Advancements
- Germany: Reduced taxation on menstrual products as essential items
- United States: “Menstrual Equity For All Act” proposal for accessibility
- Nepal: Legislation against chhaupadi (menstrual isolation practice)
- Colombia: Constitutional Court ruling on menstrual dignity rights
These global practices demonstrate the increasing recognition of menstrual health as a fundamental aspect of public health and human rights. As healthcare professionals, advocating for improved menstrual health policies and education can significantly impact women’s overall wellbeing.
Summary
The menstrual cycle is a sophisticated physiological process orchestrated by the hypothalamic-pituitary-ovarian axis. It consists of cyclical changes in hormone levels that drive follicular development, ovulation, and endometrial preparation for potential implantation. Understanding the menstrual cycle physiology is essential for nursing assessment, clinical interpretation, patient education, and promotion of menstrual hygiene.
Key aspects of the menstrual cycle include:
- Hormonal regulation through GnRH, FSH, LH, estrogen, and progesterone
- Ovarian phases (follicular, ovulation, luteal) coinciding with endometrial phases (menstrual, proliferative, secretory)
- Cyclic endometrial changes in preparation for potential implantation
- Clinical significance in fertility awareness, contraception, and menstrual disorders
- Importance of proper menstrual hygiene practices for health and wellbeing
As nursing professionals, providing evidence-based education on menstrual cycle physiology and hygiene practices empowers patients to make informed decisions about their reproductive health and overall wellbeing.
References
- 1. Reed, B. G., & Carr, B. R. (2018). The Normal Menstrual Cycle and the Control of Ovulation. In K. R. Feingold et al. (Eds.), Endotext. South Dartmouth, MA: MDText.com, Inc.
- 2. Mihm, M., Gangooly, S., & Muttukrishna, S. (2011). The normal menstrual cycle in women. Animal Reproduction Science, 124(3-4), 229-236.
- 3. Hawkins, S. M., & Matzuk, M. M. (2008). The menstrual cycle: basic biology. Annals of the New York Academy of Sciences, 1135, 10-18.
- 4. Sommer, M., Chandraratna, S., Cavill, S., Mahon, T., & Phillips-Howard, P. (2016). Managing menstruation in the workplace: an overlooked issue in low- and middle-income countries. International Journal for Equity in Health, 15, 86.
- 5. World Health Organization. (2022). Guide to menstrual hygiene materials. Geneva: World Health Organization.
- 6. American College of Obstetricians and Gynecologists. (2020). Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Committee Opinion No. 651.
- 7. Critchley, H. O., Maybin, J. A., Armstrong, G. M., & Williams, A. R. (2020). Physiology of the Endometrium and Regulation of Menstruation. Physiological Reviews, 100(3), 1149-1179.
- 8. Hennegan, J., Shannon, A. K., Rubli, J., Schwab, K. J., & Melendez-Torres, G. J. (2019). Women’s and girls’ experiences of menstruation in low- and middle-income countries: A systematic review and qualitative metasynthesis. PLoS Medicine, 16(5), e1002803.
