Fertilization, Conception, and Implantation
A Comprehensive Guide for Nursing Students
Table of Contents
Introduction
Human reproduction is a complex, precisely orchestrated process that represents one of the fundamental aspects of life. Understanding the mechanisms of fertilization, conception, and implantation is crucial for nursing professionals working in reproductive health, obstetrics, and gynecology. This knowledge forms the foundation for comprehending normal pregnancies as well as reproductive disorders.
Human reproduction begins with the creation of specialized cells called gametes (sperm and eggs), continues through fertilization and early development, and ultimately results in implantation of the embryo in the uterine wall. Each step of this process requires specific conditions and timing for successful outcomes.
Key Requirements for Successful Reproduction:
- Healthy gamete formation
- Successful transport of both sperm and egg
- Properly timed fertilization
- Normal embryonic development
- Receptive uterine environment for implantation
Gamete Formation
Gametes are specialized reproductive cells that contain half the chromosomal complement of typical body cells. In humans, these haploid cells each contain 23 chromosomes (compared to the 46 chromosomes in diploid somatic cells). When they unite during fertilization, they restore the full diploid complement.
Spermatogenesis
Spermatogenesis is the process by which mature sperm cells (spermatozoa) develop from precursor cells in the testes. Unlike egg formation, sperm production continues throughout adult male life.
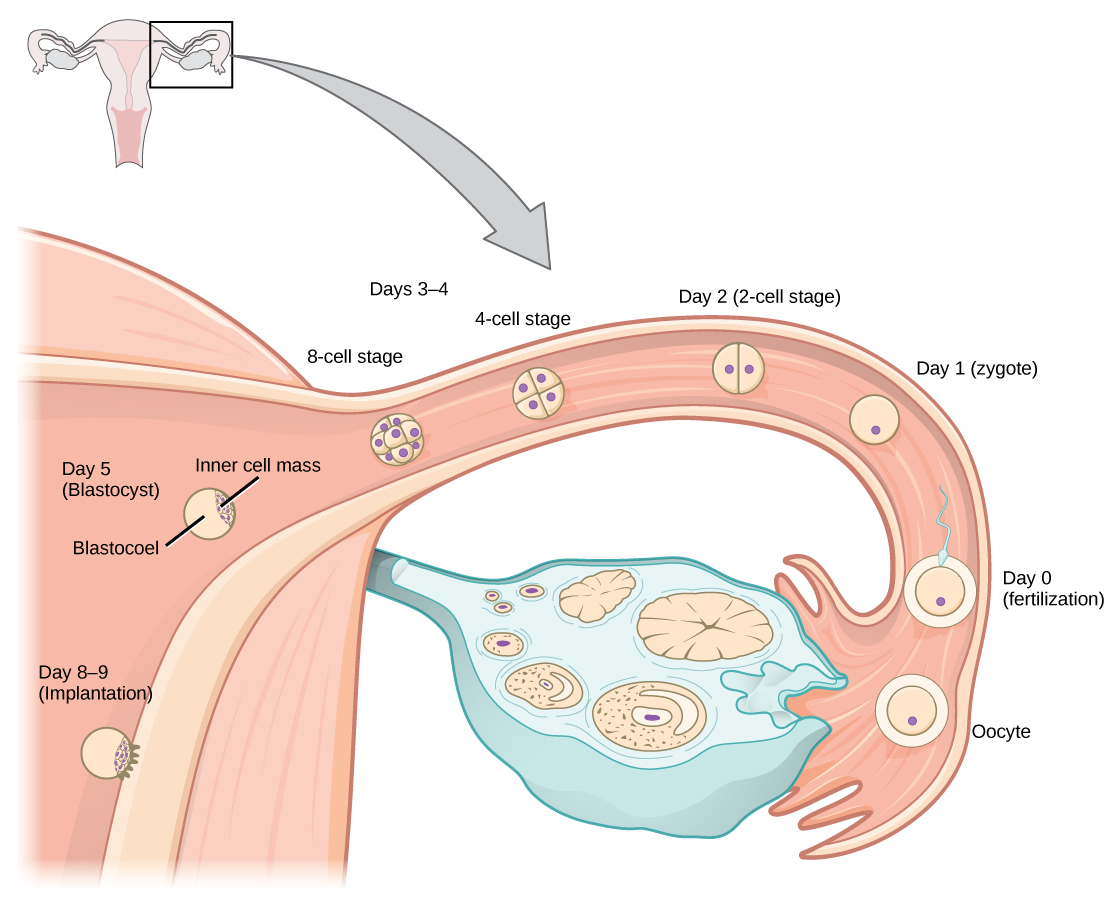
Figure 1: Development of sperm and egg cells through meiosis. Note the differences in the resulting cells.
Key features of spermatogenesis:
- Begins at puberty and continues throughout life
- Takes approximately 74 days to complete
- Occurs in the seminiferous tubules of the testes
- Involves mitotic division of spermatogonia, followed by meiotic division
- Results in four haploid spermatids from each primary spermatocyte
- Spermatids undergo metamorphosis (spermiogenesis) to become functional sperm
Mature sperm cells consist of:
- Head: Contains the nucleus with condensed DNA and the acrosome with enzymes necessary for penetrating the egg
- Midpiece: Houses mitochondria that provide energy for movement
- Tail (flagellum): Propels the sperm through fluid by whip-like movements
Oogenesis
Oogenesis is the process of female gamete (egg or ovum) formation. Unlike spermatogenesis, oogenesis begins before birth and has extended pause periods.
Key features of oogenesis:
- Begins during fetal development with approximately 7 million oogonia
- By birth, the number decreases to around 1 million immature eggs
- At puberty, about 400,000 immature eggs remain
- Only 400-500 eggs will mature and be released during a woman’s reproductive years
- Primary oocytes remain arrested in prophase I of meiosis from fetal development until ovulation
- Meiosis resumes and continues only if fertilization occurs
| Characteristic | Spermatogenesis | Oogenesis |
|---|---|---|
| Timing | Begins at puberty, continues throughout life | Begins during fetal development, pauses until puberty |
| Location | Seminiferous tubules in testes | Ovarian follicles in ovaries |
| Duration | Approximately 74 days | From fetal life to fertilization (can be decades) |
| Number produced | Millions daily | Usually one per month during reproductive years |
| Products from one primary cell | Four functional sperm | One functional egg and three polar bodies |
| Cytoplasmic division | Equal | Unequal (egg retains most cytoplasm) |
Gamete Formation Mnemonic: “ONE SPE(A)RM”
Oogenesis produces Numerous Eggs before birth
SPermatogenesis produces Endless sperm cells After puberty Repeating Mitosis
Fertilization Process
Fertilization is the fusion of gametes to produce a new organism. In humans, this process takes place in the ampulla of the fallopian tube. For fertilization to occur successfully, several sequential events must take place.
Figure 2: The process of fertilization, zygote development, and implantation in the human reproductive system.
Sperm Transport
After ejaculation, sperm begin their journey through the female reproductive tract. This process involves several critical steps:
- Semen liquefaction: Following ejaculation, semen forms a gel that protects sperm from the acidic environment of the vagina. Within 20-30 minutes, enzymes from the prostate gland liquefy this gel, freeing the sperm for transport.
- Cervical mucus navigation: During ovulation, cervical mucus becomes thinner and less acidic, creating a more favorable environment for sperm passage. The cervical mucus acts as a reservoir, allowing for extended sperm survival.
- Uterine transport: Contractions in the uterus help propel sperm upward into the fallopian tubes.
- Capacitation: Sperm undergo biochemical changes in the female reproductive tract that allow them to fertilize an egg. This process takes several hours and involves the removal of cholesterol from the sperm membrane and changes in motility patterns.
Sperm Survival Facts:
Healthy sperm can survive in the female reproductive tract for up to 5 days, though fertility is highest with intercourse 1-2 days before ovulation. Of the approximately 200 million sperm released during ejaculation, only a few hundred reach the vicinity of the egg.
Egg Transport
Egg transport begins with ovulation and concludes when the egg reaches the uterus (if not fertilized).
- Ovulation: Triggered by the LH surge, the mature follicle ruptures and releases the secondary oocyte (commonly referred to as an egg).
- Capture by fimbriae: Finger-like projections called fimbriae sweep over the surface of the ovary and guide the released egg into the fallopian tube.
- Transport in fallopian tube: Cilia within the tube and muscular contractions move the egg toward the uterus. This journey takes approximately 30 hours.
- Viability window: After ovulation, the egg remains viable for only 12-24 hours. If fertilization does not occur during this period, the egg will degenerate.
Fertilization Steps
The actual process of fertilization involves several critical steps:
Fertilization Steps Mnemonic: “BRRT”
Binding of sperm to zona pellucida
Reaction of the acrosome
Reaction of the cortex (cortical reaction)
Transfer of genetic material
- Binding: The sperm head contains receptors that bind specifically to ZP3 glycoproteins in the zona pellucida surrounding the egg.
- Acrosomal reaction: Once bound, the sperm releases enzymes from the acrosome that digest a path through the zona pellucida.
- Sperm entry: A single sperm penetrates through the zona pellucida and contacts the egg cell membrane.
- Membrane fusion: The plasma membranes of the egg and sperm fuse, allowing the sperm nucleus to enter the egg.
- Cortical reaction: The egg releases enzymes from cortical granules that alter the zona pellucida, preventing additional sperm from entering (block to polyspermy).
- Completion of meiosis II: The entry of the sperm triggers the egg to complete its second meiotic division.
- Pronuclei formation: The sperm and egg nuclei swell and are transformed into male and female pronuclei.
- DNA synthesis: DNA replication occurs in both pronuclei.
- Syngamy: The pronuclei membranes break down, and the chromosomes align on a common spindle, completing fertilization.
Clinical Consideration:
Polyspermy (fertilization by multiple sperm) is abnormal and usually results in a non-viable zygote. The cortical reaction prevents this by creating a fast block (electrical depolarization of the egg membrane) and a slow block (zona reaction) to additional sperm entry.
Zygote Development and Transportation
Following fertilization, the newly formed zygote undergoes rapid cell division while traveling through the fallopian tube toward the uterus. This early developmental process is critical for establishing the foundation of the embryo.
Cleavage and Early Development
The zygote undergoes a series of mitotic divisions called cleavage, which increases the cell number without increasing the overall size:
- Day 1: Single-celled zygote (2n = 46 chromosomes)
- Day 2: 2-4 cell stage
- Day 3: 8-16 cell stage (morula)
- Day 4: Early blastocyst formation begins
- Day 5: Blastocyst with distinct inner cell mass and trophoblast
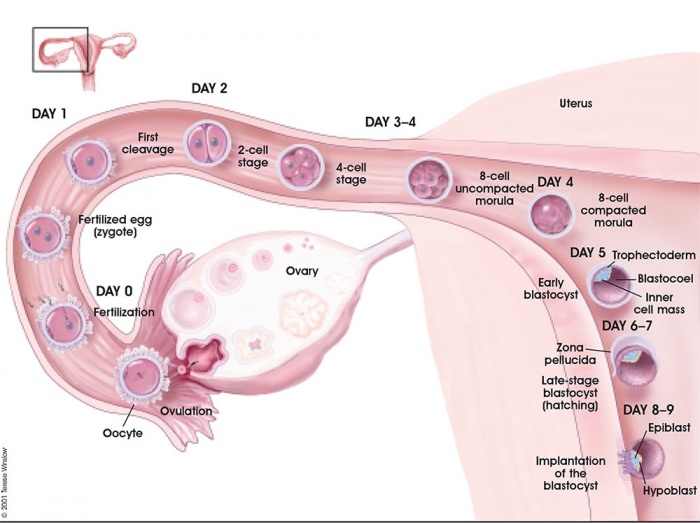
Figure 3: Early embryonic development from fertilization through implantation.
The Morula
The morula is a solid ball of cells formed by approximately day 3 after fertilization. Key features include:
- 16-32 tightly packed blastomeres
- No significant increase in overall size from the zygote
- Compaction of cells, establishing initial cell polarity
- First evidence of cell differentiation
The Blastocyst
By day 4-5, the morula develops into a blastocyst with distinct features:
- Trophoblast: Outer layer of cells that will develop into extraembryonic structures including the placenta
- Inner cell mass (embryoblast): Cluster of cells that will develop into the embryo proper
- Blastocoel: Fluid-filled cavity inside the blastocyst
- Zona pellucida: Still present but beginning to thin
Zona Hatching
Before implantation can occur, the blastocyst must escape from the zona pellucida, a process called “hatching”:
- Occurs around day 5-6 after fertilization
- Facilitated by proteolytic enzymes released by the trophoblast
- Allows direct contact between the trophoblast and endometrium
- Necessary prerequisite for implantation
Early Development Mnemonic: “MITCH-B”
Morula develops by day 3 (16 cells)
Inner cell mass forms by day 4
Trophoblast surrounds the outer layer
Cavity forms (blastocoel)
Hatching from zona pellucida by day 5-6
Blastocyst ready for implantation
Implantation
Implantation is the process by which the blastocyst attaches to and embeds within the endometrium of the uterus. This process typically begins around 6-7 days after fertilization and is completed by 10-12 days. Successful implantation establishes the pregnancy and initiates placental development.
Critical Timing:
For implantation to occur successfully, the blastocyst development must synchronize with the receptivity of the endometrium. This creates a limited “window of implantation” lasting approximately 24-36 hours, typically occurring 7-10 days after ovulation.
Five Stages of Implantation
Implantation occurs through five distinct yet sequential stages:
| Stage | Description | Key Events |
|---|---|---|
| 1. Migration and Hatching | Movement of blastocyst to implantation site and escape from zona pellucida |
|
| 2. Pre-contact (Apposition) | Initial loose connection between blastocyst and endometrium |
|
| 3. Attachment | Stronger connection between trophoblast and endometrial epithelium |
|
| 4. Adhesion | Further strengthening of attachment with molecular binding |
|
| 5. Invasion | Penetration of trophoblasts into endometrium |
|
Window of Implantation
The window of implantation refers to the limited timeframe when the endometrium is receptive to embryo implantation. Several factors contribute to creating this window:
Endometrial Factors:
- Pinopodes: Mushroom-like projections from the endometrial epithelial cells that appear during the receptive phase
- Adhesion molecules: Expression of specific integrins and other adhesion molecules
- Decidualization: Transformation of endometrial stromal cells into specialized decidual cells
- Cytokines: Increased production of LIF, IL-6, and other cytokines
- Reduced mucin expression: Decreased expression of MUC1 and MUC16 that normally inhibit adhesion
Hormonal Regulation:
- Estrogen: Stimulates endometrial proliferation in the early secretory phase
- Progesterone: Induces secretory changes and decidualization
- hCG: Produced by the blastocyst to maintain corpus luteum function
Clinical Perspective: Implantation Failure
Implantation failure is a significant cause of infertility and early pregnancy loss. Factors that can interfere with implantation include:
- Endometrial receptivity defects
- Embryo chromosomal abnormalities
- Hormonal imbalances
- Immunological factors
- Anatomical abnormalities of the uterus
These factors are important considerations in the evaluation and management of recurrent implantation failure in assisted reproduction.
Post-implantation Events
Following successful implantation, several critical events occur:
- Placental development: Trophoblast cells continue to invade maternal tissues, establishing early placental structures
- Hormone production: Syncytiotrophoblast produces hCG, which maintains corpus luteum function
- Embryonic development: The inner cell mass continues to develop into the embryo proper
- Immunological adaptation: Maternal immune system adapts to tolerate the semi-allogenic embryo
- Vascular remodeling: Extravillous trophoblasts remodel maternal spiral arteries to enhance blood flow
Clinical Implications
Understanding the normal processes of fertilization, conception, and implantation is essential for diagnosing and managing reproductive health issues. Abnormalities at any stage can result in infertility, early pregnancy loss, or other reproductive disorders.
Infertility Factors
| Process Stage | Potential Issues | Clinical Assessment |
|---|---|---|
| Gamete Production |
|
|
| Gamete Transport |
|
|
| Fertilization |
|
|
| Early Development |
|
|
| Implantation |
|
|
Early Pregnancy Assessment
Signs and symptoms of successful implantation and early pregnancy:
- Implantation bleeding: Light spotting 6-12 days after fertilization as the blastocyst embeds in the endometrium
- Missed menstrual period: Most common early sign of pregnancy
- hCG detection: The basis for pregnancy tests, detectable in blood 7-10 days after fertilization and in urine 12-14 days after fertilization
- Early pregnancy symptoms: Breast tenderness, fatigue, nausea, food aversions (typically begin 2-8 weeks after conception)
Nursing Consideration:
Not all implantation bleeding is normal. Patients should be educated to report heavy bleeding, severe pain, or passage of tissue, as these may indicate ectopic pregnancy or early miscarriage.
Assisted Reproductive Technologies (ART)
Various techniques have been developed to overcome barriers to natural conception:
- In Vitro Fertilization (IVF): Eggs and sperm are combined in a laboratory dish, and resulting embryos are transferred to the uterus
- Intracytoplasmic Sperm Injection (ICSI): Direct injection of a single sperm into an egg
- Assisted Hatching: Creating a small opening in the zona pellucida to facilitate embryo hatching
- Embryo Transfer: Placement of embryos into the uterus at the optimal time for implantation
- Endometrial Preparation: Hormonal treatment to optimize the uterine environment for implantation
Helpful Mnemonics
Memorizing the complex processes of fertilization, conception, and implantation can be challenging. Here are additional mnemonics to help nursing students retain this information:
Sperm Journey: “SEVEN UP”
Seminiferous tubules
Epididymis
Vas deferens
Ejaculatory duct
Nothing
Urethra
Penis
Fertilization to Implantation: “ZEBRA”
Zygote formation (fertilization)
Early cleavage (2-4 cell)
Ball of cells (morula)
Ready blastocyst
Attachment and invasion (implantation)
Window of Implantation: “POWER”
Pinopodes appear
Open receptivity
Week 3 of cycle (days 20-24)
Endometrium secretory phase
Receptors expressed
Implantation Stages: “MAP-AI”
Migration and hatching
Apposition (pre-contact)
Positive attachment
Adhesion strengthening
Invasion of trophoblasts
Review & Key Points
Understanding the process of fertilization, conception, and implantation is crucial for nursing practice in reproductive health, obstetrics, and gynecology. Let’s review the most important concepts:
Key Points – Reproductive Process:
- Gamete Formation: Spermatogenesis produces millions of sperm daily throughout adult male life. Oogenesis begins before birth and releases one mature egg approximately monthly during reproductive years.
- Fertilization: Occurs in the ampulla of the fallopian tube when a single sperm penetrates the egg, restoring the diploid number of chromosomes and creating a zygote.
- Early Development: The zygote undergoes cleavage to form a morula, then develops into a blastocyst with inner cell mass and trophoblast.
- Zona Hatching: The blastocyst must escape from its protective zona pellucida before implantation can occur.
- Implantation: A five-stage process (migration/hatching, apposition, attachment, adhesion, invasion) that embeds the blastocyst in the endometrium.
- Window of Implantation: Limited timeframe (24-36 hours) when the endometrium is receptive to implantation, typically 7-10 days after ovulation.
- Biochemical Recognition: hCG produced by the implanting embryo maintains corpus luteum function and prevents menstruation.
Nursing Assessment in Reproductive Health
When assessing patients with fertility concerns or in early pregnancy, nurses should consider:
- Menstrual history and cycle regularity
- Timing of intercourse relative to ovulation
- Previous pregnancy outcomes
- Age-related fertility factors
- Lifestyle factors (smoking, alcohol, weight, stress)
- Environmental exposures
- Signs and symptoms of early pregnancy
- Warning signs of complications
Patient Education
Effective patient education about reproduction should include:
- Basic reproductive anatomy and physiology
- Optimal timing of intercourse for conception
- Methods to track ovulation
- Lifestyle modifications to enhance fertility
- Age-related fertility decline
- When to seek medical evaluation for infertility
- Early pregnancy signs and symptoms
- Pregnancy test timing and interpretation
Global Perspectives on Reproductive Health
Around the world, different approaches to reproductive education and care exist:
- Japan: Features advanced reproductive technologies but faces declining birth rates due to social and economic factors
- Nordic Countries: Comprehensive reproductive education starting at young ages with good outcomes
- Sub-Saharan Africa: Growing focus on integrating traditional midwifery knowledge with modern medical practice
- Australia: Pioneered “Fertility Awareness” programs for young adults to increase knowledge about age-related fertility decline
Nurses should maintain cultural sensitivity when discussing reproduction with patients from diverse backgrounds.
