Cardiac Tamponade
12 Comprehensive Nursing Care Plans
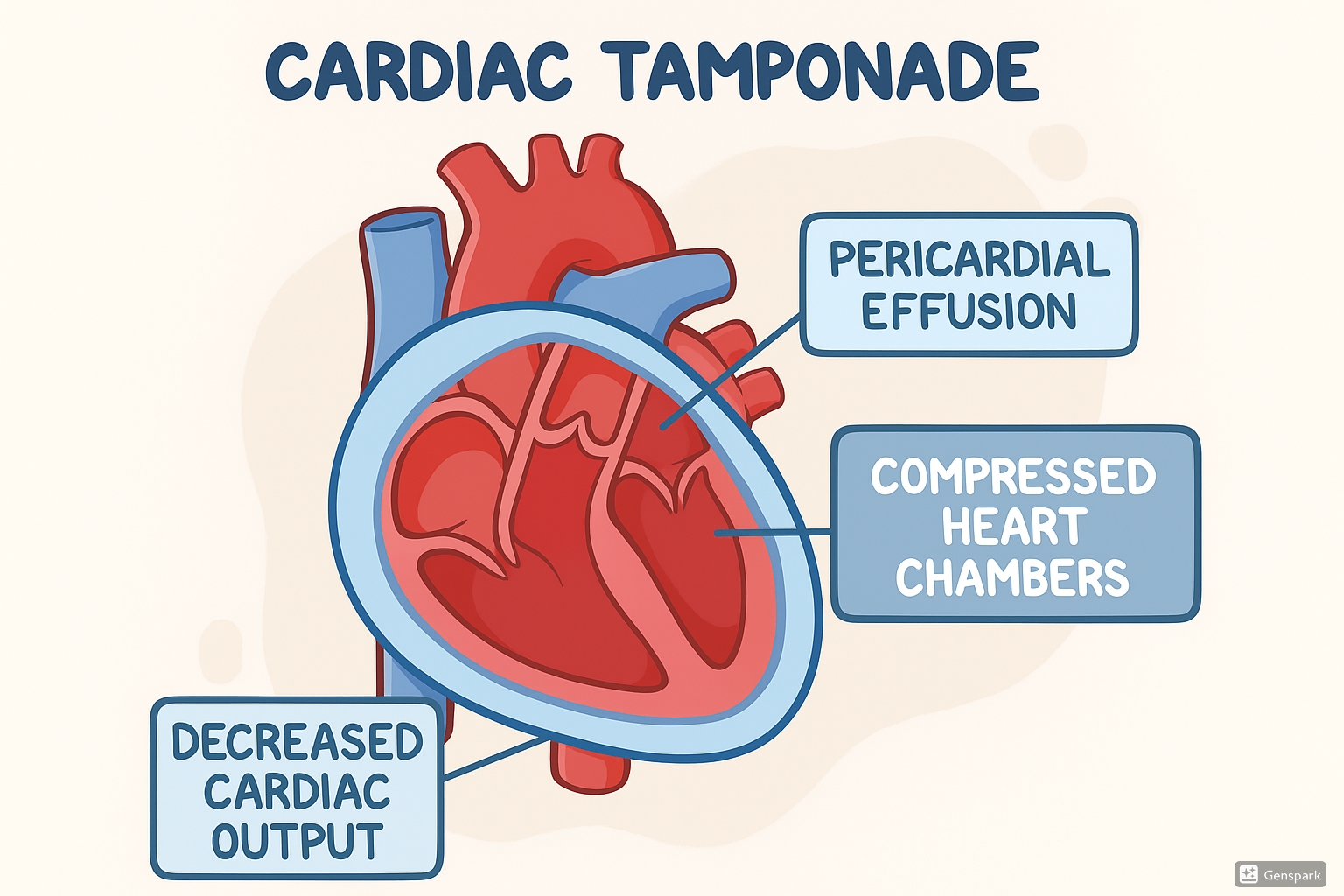
Cardiac tamponade showing fluid accumulation around the heart, compressed chambers, and decreased cardiac output
Overview
Cardiac tamponade is a life-threatening condition characterized by the accumulation of excessive fluid within the pericardial space, resulting in impaired cardiac filling, reduced stroke volume, and compression of the epicardial coronary arteries, which can lead to myocardial ischemia. This medical emergency requires prompt recognition and intervention to prevent cardiovascular collapse and cardiac arrest.
Table of Contents
Pathophysiology
Understanding Cardiac Tamponade
The heart is surrounded by a two-layered fibrous sac called the pericardium. Within this sac is the pericardial cavity containing a small amount of fluid (15-50ml) that allows the heart to move freely during contractions.
In cardiac tamponade, the pericardial cavity accumulates an abnormal amount of fluid (exudate, transudate, or blood), which puts pressure on the heart and restricts its movement and filling capacity.
Key Mechanism: The increased pressure from fluid accumulation compresses the heart chambers, particularly the right atrium and right ventricle during diastole, preventing adequate filling.
Progression of Pathophysiology:
- Fluid accumulates in the pericardial space
- Increased intrapericardial pressure compresses cardiac chambers
- Reduced ventricular filling during diastole
- Decreased stroke volume and cardiac output
- Compromised tissue perfusion throughout the body
- Compensatory tachycardia and increased systemic vascular resistance
- Eventually leads to obstructive shock and cardiovascular collapse
The speed of fluid accumulation is crucial in determining the clinical presentation. A rapidly developing tamponade (as little as 100ml of fluid) can be immediately life-threatening, while a slowly developing tamponade may allow the pericardium to stretch and accommodate as much as 1-2 liters before symptoms appear.
Etiology & Risk Factors
- Penetrating chest trauma (gunshot wounds, stab wounds)
- Blunt chest trauma (steering wheel impacts)
- Post-cardiac surgery
- Iatrogenic causes (central line insertion, pacemaker lead perforation)
- Aortic dissection with rupture into pericardium
- Myocardial rupture post-MI
- Malignancies (lung cancer, breast cancer, lymphoma, leukemia)
- Infections (viral, bacterial, fungal, tuberculosis)
- Autoimmune disorders (rheumatoid arthritis, lupus)
- Uremia (end-stage renal disease)
- Hypothyroidism (myxedema)
- Radiation therapy to the chest
- Drug-induced (anticoagulants, hydralazine, procainamide)
Clinical Presentation
Hypotension
Due to decreased cardiac output
Jugular Venous Distention
Due to increased central venous pressure
Muffled Heart Sounds
Due to fluid buffer between heart and stethoscope
| System | Manifestations |
|---|---|
| Cardiovascular |
|
| Respiratory |
|
| Neurological |
|
| Gastrointestinal |
|
| Integumentary |
|
| Renal |
|
Diagnostic Evaluations
Echocardiography (Gold Standard)
Shows pericardial effusion, diastolic collapse of right atrium and ventricle, swinging heart motion
Chest X-ray
Enlarged cardiac silhouette (“water bottle” heart) if effusion >200ml
CT Scan/MRI
Can confirm effusion and may identify underlying cause
Electrocardiogram (ECG)
- Sinus tachycardia
- Low QRS voltage
- Electrical alternans (alternating QRS amplitude)
Hemodynamic Monitoring
- Equalization of diastolic pressures in all chambers
- Elevated central venous pressure
- Pulsus paradoxus >10 mmHg
Nursing Care Plan 1: Decreased Cardiac Output
Assessment Findings/Defining Characteristics:
- Hypotension (systolic BP <90 mmHg)
- Tachycardia (heart rate >100 bpm)
- Narrowed pulse pressure (<30 mmHg)
- Pulsus paradoxus (>10 mmHg drop in systolic BP during inspiration)
- Jugular venous distention
- Muffled heart sounds
- Decreased urine output (<30 ml/hr)
- Cool, clammy skin
- Altered mental status
- Weak peripheral pulses
Expected Outcomes:
- Patient will maintain adequate cardiac output as evidenced by BP within 10% of baseline, HR 60-100 bpm, and urine output >30 ml/hr
- Patient will demonstrate improved tissue perfusion with warm extremities, strong peripheral pulses, and capillary refill <3 seconds
- Patient will remain alert and oriented with no signs of decreased cerebral perfusion
| Nursing Interventions | Rationales |
|---|---|
| Monitor vital signs continuously, with particular attention to blood pressure, heart rate, and presence of pulsus paradoxus | Early detection of hemodynamic deterioration allows for prompt intervention. Pulsus paradoxus >10 mmHg is a classic sign of cardiac tamponade |
| Position patient in high Fowler’s position (30-45° elevation) unless contraindicated | This position decreases venous return to the heart, reducing preload and cardiac workload |
| Administer supplemental oxygen as ordered to maintain SpO₂ >94% | Improves oxygen delivery to tissues when cardiac output is compromised |
| Initiate two large-bore IV lines (16-18 gauge) and administer IV fluids as ordered | Volume expansion increases venous return and right atrial pressure, which can temporarily improve cardiac filling and output despite tamponade |
| Monitor intake and output hourly; maintain accurate fluid balance records | Decreased urine output (<30 ml/hr) may indicate inadequate renal perfusion due to decreased cardiac output |
| Prepare for emergency pericardiocentesis; assemble equipment and assist physician during procedure | Removal of pericardial fluid is the definitive treatment for cardiac tamponade to relieve cardiac compression and restore normal hemodynamics |
| Administer inotropic agents (e.g., dobutamine) as prescribed | Increases myocardial contractility to enhance stroke volume and cardiac output in the presence of compromised filling |
| Continuously monitor cardiac rhythm via telemetry or bedside monitor | Detects dysrhythmias that may develop due to myocardial ischemia from coronary artery compression or electrolyte imbalances |
| Restrict activity and provide assistance with basic care needs | Decreases oxygen demand and cardiac workload when cardiac output is compromised |
| Monitor for signs of decreased cerebral perfusion (confusion, restlessness, decreased level of consciousness) | The brain is highly sensitive to decreased perfusion, and changes in mental status may be an early indicator of deteriorating cardiac output |
Evaluation:
- Patient maintains blood pressure within 10% of baseline
- Heart rate returns to 60-100 bpm
- Urine output is maintained at >30 ml/hr
- Peripheral pulses are strong and equal
- Skin is warm and dry
- Patient remains alert and oriented
- Hemodynamic parameters improve after pericardiocentesis
Nursing Care Plan 2: Impaired Gas Exchange
Assessment Findings/Defining Characteristics:
- Dyspnea
- Tachypnea (respiratory rate >24 breaths/min)
- Decreased oxygen saturation (SpO₂ <94% on room air)
- Abnormal arterial blood gases (hypoxemia, respiratory alkalosis)
- Use of accessory muscles for breathing
- Restlessness
- Confusion
- Cyanosis (late sign)
Expected Outcomes:
- Patient will maintain adequate oxygenation as evidenced by SpO₂ >94% and normal respiratory rate (12-20 breaths/min)
- Patient will demonstrate improved gas exchange as evidenced by normal arterial blood gases
- Patient will report decreased dyspnea
- Patient will exhibit no signs of respiratory distress
| Nursing Interventions | Rationales |
|---|---|
| Monitor respiratory rate, pattern, and effort every 1-2 hours or more frequently if unstable | Early detection of respiratory distress allows for timely intervention |
| Monitor oxygen saturation continuously via pulse oximetry | Provides ongoing assessment of oxygenation status and effectiveness of interventions |
| Administer supplemental oxygen via appropriate delivery method to maintain SpO₂ >94% | Improves oxygenation when gas exchange is compromised due to decreased pulmonary blood flow |
| Position patient in semi-Fowler’s or high Fowler’s position | Optimizes lung expansion and decreases work of breathing |
| Monitor arterial blood gases as ordered | Provides comprehensive assessment of oxygenation, ventilation, and acid-base status |
| Assess for signs of increasing respiratory distress (increased work of breathing, use of accessory muscles, nasal flaring) | Indicates worsening gas exchange and need for more aggressive intervention |
| Conserve patient’s energy by spacing activities and providing rest periods | Reduces oxygen demand and work of breathing when gas exchange is compromised |
| Prepare for possible intubation and mechanical ventilation if respiratory status deteriorates | Severe cardiac tamponade may lead to respiratory failure requiring advanced airway management |
| Teach and encourage deep breathing exercises | Promotes alveolar expansion and improves ventilation |
| Monitor mental status for changes that may indicate cerebral hypoxia | Confusion or altered mental status may be early signs of inadequate cerebral oxygenation |
Evaluation:
- Patient maintains oxygen saturation >94%
- Respiratory rate returns to normal range (12-20 breaths/min)
- Patient reports decreased dyspnea
- Arterial blood gases return to normal parameters
- No signs of respiratory distress are observed
- Patient remains alert and oriented
Nursing Care Plan 3: Ineffective Breathing Pattern
Assessment Findings/Defining Characteristics:
- Tachypnea (respiratory rate >24 breaths/min)
- Shallow breathing
- Use of accessory muscles
- Altered chest excursion
- Shortness of breath
- Kussmaul breathing (deep, rapid breathing)
- Anxiety related to difficulty breathing
Expected Outcomes:
- Patient will demonstrate effective breathing pattern with respiratory rate 12-20 breaths/min
- Patient will exhibit normal chest expansion and no use of accessory muscles
- Patient will report decreased shortness of breath
| Nursing Interventions | Rationales |
|---|---|
| Monitor respiratory rate, depth, and pattern every 1-2 hours or more frequently if unstable | Allows early detection of changes in breathing pattern and effectiveness of interventions |
| Position patient in semi-Fowler’s or high Fowler’s position (30-45° elevation) | Facilitates lung expansion and decreases work of breathing by reducing pressure on the diaphragm |
| Teach and assist with deep breathing exercises and incentive spirometry every 2 hours while awake | Promotes lung expansion, mobilizes secretions, and prevents atelectasis |
| Teach pursed-lip breathing techniques | Increases airway pressure during exhalation, preventing airway collapse and reducing air trapping |
| Administer supplemental oxygen as ordered | Improves oxygenation during periods of ineffective breathing |
| Implement relaxation techniques (guided imagery, progressive muscle relaxation) to reduce anxiety | Anxiety can worsen breathing pattern and create a cycle of increased respiratory distress |
| Monitor for signs of respiratory fatigue (increasing respiratory rate, decreasing tidal volume) | Indicates worsening condition and potential need for ventilatory support |
| Administer analgesics as prescribed for pain management | Pain can lead to shallow breathing and splinting, which compromises ventilation |
| Provide a calm environment and minimize stressors | Reduces anxiety which can contribute to rapid, shallow breathing |
| Document and report significant changes in breathing pattern | Ensures continuity of care and appropriate escalation of interventions if needed |
Evaluation:
- Respiratory rate returns to 12-20 breaths/min
- Normal depth and pattern of breathing are restored
- No use of accessory muscles is observed
- Patient reports decreased shortness of breath
- Normal symmetric chest expansion is observed
- Patient demonstrates effective breathing techniques
Nursing Care Plan 4: Activity Intolerance
Assessment Findings/Defining Characteristics:
- Exertional dyspnea
- Fatigue or weakness
- Abnormal heart rate or blood pressure response to activity (increase in HR >20 bpm, decrease in BP)
- Oxygen saturation decrease with activity
- Pallor or cyanosis with activity
- Expressed feelings of weakness
- Inability to perform activities of daily living
Expected Outcomes:
- Patient will demonstrate improved tolerance to activity as evidenced by stable vital signs during and after activity
- Patient will balance activity with appropriate rest periods
- Patient will report decreased fatigue and dyspnea during activity
- Patient will maintain oxygen saturation >94% during activities
| Nursing Interventions | Rationales |
|---|---|
| Assess baseline activity tolerance using a standardized scale (0-10) | Provides objective measurement for evaluating progress and planning activity progression |
| Monitor vital signs before, during, and after activity | Determines physiological response to activity and helps identify appropriate activity levels |
| Start with low-level activities and gradually increase as tolerated | Progressive activity prevents excessive cardiac workload while preventing deconditioning |
| Schedule activities during periods of highest energy; avoid scheduling activities immediately after meals | Maximizes patient’s limited energy resources; digestion diverts blood flow from muscles to digestive organs |
| Assist with activities of daily living as needed; encourage self-care as tolerated | Conserves energy while promoting independence and preventing complete deconditioning |
| Teach energy conservation techniques (pacing, prioritizing, planning, positioning) | Helps patient accomplish necessary activities while minimizing oxygen demand |
| Ensure adequate rest periods between activities | Allows restoration of energy reserves and prevents excessive fatigue |
| Administer supplemental oxygen during activity as ordered | Supports increased oxygen demands during activity when cardiac output is compromised |
| Instruct patient to report symptoms such as chest pain, dizziness, or severe shortness of breath | These symptoms indicate activity exceeds cardiac reserve and should be discontinued immediately |
| Collaborate with physical therapy for appropriate exercise prescription after stabilization | Provides specialized assessment and interventions to improve activity tolerance safely |
Evaluation:
- Heart rate remains within 20 bpm of resting rate during activity
- Blood pressure remains stable during activity
- Oxygen saturation remains >94% during activity
- Patient reports decreased fatigue with activity
- Patient demonstrates ability to pace activities and use energy conservation techniques
- Activity tolerance gradually improves over time
Nursing Care Plan 5: Acute Pain
Assessment Findings/Defining Characteristics:
- Verbal reports of chest pain or discomfort
- Guarding or protective behaviors
- Facial grimacing
- Pain that may worsen with deep breathing or lying flat
- Pain described as sharp, stabbing, or pressure-like
- Pain that may radiate to neck, shoulders, or back
- Restlessness or agitation
Expected Outcomes:
- Patient will report pain reduced to a tolerable level (≤3 on a 0-10 scale)
- Patient will demonstrate use of non-pharmacological pain management techniques
- Patient will exhibit decreased physical signs of pain
- Patient will verbalize understanding of pain management plan
| Nursing Interventions | Rationales |
|---|---|
| Assess pain comprehensively using a standardized pain scale, including location, quality, intensity, onset, duration, and aggravating/relieving factors | Provides baseline data for planning interventions and evaluating effectiveness; helps differentiate cardiac tamponade pain from other cardiac conditions like myocardial infarction |
| Position patient for comfort, usually in semi-Fowler’s or high Fowler’s position | Reduces pressure on the pericardium and may alleviate pain; pericardial pain often worsens when lying flat |
| Administer analgesics as prescribed, evaluating effectiveness 30 minutes after administration | Provides pharmacological pain relief; evaluation determines need for dosage adjustment |
| Apply supplemental oxygen as ordered | Improves oxygenation to ischemic tissues and may help reduce pain |
| Teach and encourage relaxation techniques (deep breathing, guided imagery, progressive muscle relaxation) | Non-pharmacological approaches can reduce pain perception and anxiety, which can exacerbate pain |
| Provide quiet environment and minimize disruptions | Environmental stressors can increase perception of pain |
| Assist with gentle position changes as needed | Prevents sudden movements that may exacerbate pain |
| Document pain assessments, interventions, and patient response | Ensures continuity of care and evaluation of pain management effectiveness |
| Explain that pericardiocentesis or definitive treatment of tamponade should alleviate pain | Understanding that pain relief will come with treatment can provide reassurance |
| Monitor for signs that pain is worsening, which may indicate progression of tamponade | Changes in pain characteristics may signal clinical deterioration requiring immediate intervention |
Evaluation:
- Patient reports pain at acceptable level (≤3 on a 0-10 scale)
- Patient demonstrates use of relaxation techniques
- Facial expressions and body posture indicate comfort
- Patient can rest and perform necessary activities without excessive pain
- Pain significantly improves after pericardiocentesis or definitive treatment
Nursing Care Plan 6: Anxiety
Assessment Findings/Defining Characteristics:
- Expressed concerns or fears
- Restlessness or agitation
- Increased heart rate and respiratory rate
- Increased blood pressure
- Verbal expressions of having “no control”
- Feelings of impending doom (common in cardiac tamponade)
- Difficulty concentrating
- Focused on self
Expected Outcomes:
- Patient will verbalize decreased anxiety
- Patient will demonstrate relaxed body language and calm facial expression
- Patient will use effective coping strategies to manage anxiety
- Patient will verbalize understanding of condition, treatment, and procedures
- Patient will exhibit stable vital signs not influenced by anxiety
| Nursing Interventions | Rationales |
|---|---|
| Establish therapeutic relationship using calm, reassuring approach | Creates trust and helps patient feel safe in a stressful situation |
| Assess level of anxiety using standardized scale (mild, moderate, severe) | Provides baseline for evaluating effectiveness of interventions |
| Provide clear, concise information about condition, treatments, and procedures | Knowledge helps reduce fear of the unknown and gives patient sense of control |
| Explain all procedures before performing them | Reduces surprise and anxiety related to unexpected interventions |
| Encourage expression of feelings and concerns | Verbalization of fears can reduce their intensity and help identify specific anxiety triggers |
| Teach relaxation techniques such as deep breathing, guided imagery, and progressive muscle relaxation | Provides patient with tools to self-manage anxiety; activates parasympathetic nervous system |
| Maintain a calm, quiet environment; limit number of personnel in room | Environmental stimuli can exacerbate anxiety |
| Involve family/support persons as appropriate | Presence of familiar support people often reduces anxiety |
| Administer anxiolytic medications as prescribed | Pharmacological intervention may be necessary for severe anxiety that does not respond to non-pharmacological approaches |
| Stay with patient during periods of increased anxiety, particularly before procedures | Provides reassurance and opportunity to address concerns immediately |
Evaluation:
- Patient verbalizes decreased anxiety
- Patient demonstrates use of relaxation techniques when feeling anxious
- Vital signs remain stable during procedures or discussions about condition
- Patient asks appropriate questions indicating engagement rather than avoidance
- Patient appears calm with relaxed facial expression and body language
Nursing Care Plan 7: Deficient Knowledge
Assessment Findings/Defining Characteristics:
- Verbalization of lack of information or misconceptions
- Multiple questions about condition and treatment
- Expressed uncertainty about self-care after treatment
- Inability to describe condition, causes, or warning signs
- Anxiety related to lack of understanding
- Unrealistic expectations about recovery
Expected Outcomes:
- Patient will verbalize accurate understanding of cardiac tamponade including causes, symptoms, and treatment
- Patient will demonstrate understanding of post-procedure care
- Patient will identify warning signs requiring medical attention
- Patient will verbalize understanding of medication regimen if applicable
- Patient will identify appropriate follow-up care requirements
| Nursing Interventions | Rationales |
|---|---|
| Assess patient’s current knowledge level, learning style, and readiness to learn | Establishes baseline for educational plan and identifies preferred learning methods |
| Provide information about cardiac tamponade in simple, clear language avoiding medical jargon | Ensures understanding regardless of educational background |
| Use visual aids, diagrams, and written materials to supplement verbal teaching | Addresses different learning styles and provides reference materials for later review |
| Explain pericardiocentesis or surgical procedure in detail, including preparation, expected sensations, and post-procedure care | Reduces anxiety related to unknown procedures and promotes cooperation |
| Teach signs and symptoms requiring immediate medical attention (increased shortness of breath, chest pain, fever, increased heart rate, dizziness) | Early recognition of complications enables prompt intervention |
| Provide information about post-procedure activity restrictions | Prevents complications and promotes recovery |
| Teach medication information including purpose, dosage, schedule, and side effects if applicable | Promotes adherence to medication regimen and recognition of adverse effects |
| Provide information about follow-up appointments and testing | Ensures continued monitoring and management of condition |
| Use teach-back method to evaluate understanding | Confirms comprehension and identifies areas needing clarification |
| Provide written discharge instructions in patient’s preferred language | Serves as reference after discharge when stress or information overload may affect recall |
Evaluation:
- Patient accurately describes cardiac tamponade and its treatment
- Patient correctly identifies signs and symptoms requiring medical attention
- Patient verbalizes understanding of medication regimen if applicable
- Patient describes appropriate activity restrictions
- Patient can explain follow-up care requirements
- Patient demonstrates decreased anxiety related to improved understanding
Nursing Care Plan 8: Risk for Decreased Cardiac Tissue Perfusion
Risk Factors:
- Compression of coronary arteries from pericardial fluid
- Reduced cardiac output
- Hypotension
- Tachycardia (increased myocardial oxygen demand)
- History of coronary artery disease
- Anemia (if present)
- Hypoxemia
Expected Outcomes:
- Patient will maintain adequate cardiac tissue perfusion as evidenced by absence of chest pain, normal ECG findings, and stable cardiac enzymes
- Patient will demonstrate hemodynamic stability with adequate heart rate, blood pressure, and cardiac output
- Patient will maintain normal sinus rhythm without ischemic changes on ECG
| Nursing Interventions | Rationales |
|---|---|
| Monitor ECG continuously for changes indicating myocardial ischemia (ST-segment changes, T-wave inversion, dysrhythmias) | Early detection of myocardial ischemia allows for prompt intervention |
| Monitor cardiac enzymes (troponin, CK-MB) as ordered | Elevated cardiac enzymes indicate myocardial cell damage from ischemia |
| Assess for chest pain using standardized pain assessment tool (location, quality, radiation, severity, timing) | Chest pain may indicate myocardial ischemia due to coronary artery compression |
| Administer supplemental oxygen as ordered to maintain SpO₂ >94% | Optimizes oxygen delivery to myocardium when coronary perfusion is compromised |
| Position patient comfortably with head of bed elevated 30-45 degrees | Reduces cardiac workload and myocardial oxygen demand |
| Administer prescribed medications such as nitroglycerin for chest pain if ordered | Dilates coronary arteries and reduces preload, improving coronary perfusion and reducing myocardial oxygen demand |
| Prepare for emergency pericardiocentesis or surgical intervention | Definitive treatment to relieve cardiac compression and restore coronary blood flow |
| Monitor hemoglobin and hematocrit levels | Anemia can exacerbate myocardial ischemia due to reduced oxygen-carrying capacity |
| Minimize activities that increase myocardial oxygen demand | Reduces risk of myocardial ischemia when coronary perfusion is compromised |
| Maintain normothermia | Fever increases metabolic rate and myocardial oxygen consumption |
Evaluation:
- Patient remains free of chest pain
- ECG shows no signs of ischemia
- Cardiac enzymes remain within normal limits or return to normal after treatment
- Heart rate and blood pressure remain within normal parameters
- Patient maintains normal sinus rhythm after treatment
- Coronary perfusion improves after pericardiocentesis or surgical intervention
Nursing Care Plan 9: Risk for Infection
Risk Factors:
- Invasive procedures (pericardiocentesis, central venous catheterization)
- Presence of indwelling catheters (pericardial drain, central lines)
- Compromised immune system (if applicable)
- Malnutrition due to illness
- Prolonged hospitalization
- Surgical interventions
Expected Outcomes:
- Patient will remain free from signs and symptoms of infection
- Patient will maintain normal vital signs and white blood cell count
- Patient will demonstrate proper care of catheter sites
- Patient will verbalize understanding of signs of infection to report
| Nursing Interventions | Rationales |
|---|---|
| Maintain strict aseptic technique during all invasive procedures and dressing changes | Reduces risk of introducing pathogens during invasive procedures |
| Perform hand hygiene before and after patient contact and procedures | Hand hygiene is the most effective measure for preventing healthcare-associated infections |
| Monitor temperature every 4 hours or more frequently if indicated | Fever is often the first sign of infection |
| Inspect catheter insertion sites and incisions for signs of infection (redness, warmth, swelling, purulent drainage) | Early identification of localized infection enables prompt intervention |
| Change dressings according to facility protocol using sterile technique | Prevents contamination of insertion sites and surgical wounds |
| Monitor white blood cell count and differential | Elevation may indicate developing infection |
| Administer prophylactic antibiotics as prescribed | Prevents infection in high-risk procedures or patients |
| Ensure proper management of drainage systems (maintain closed system, empty collection devices when needed) | Prevents retrograde contamination of the pericardial space |
| Provide meticulous catheter care according to facility protocol | Reduces risk of catheter-related bloodstream infections |
| Educate patient and family about signs of infection to report | Promotes early detection and reporting of potential infectious complications |
Evaluation:
- Patient remains afebrile (temperature <100.4°F or 38°C)
- Insertion sites and incisions remain clean, dry, and intact without signs of infection
- White blood cell count remains within normal limits
- No purulent drainage from catheters or incisions
- Patient can identify signs of infection requiring medical attention
- Patient maintains normal vital signs
Nursing Care Plan 10: Ineffective Peripheral Tissue Perfusion
Assessment Findings/Defining Characteristics:
- Cool extremities
- Diminished or absent peripheral pulses
- Delayed capillary refill (>3 seconds)
- Pallor or cyanosis of extremities
- Altered sensation in extremities (numbness or tingling)
- Decreased skin temperature
- Edema
Expected Outcomes:
- Patient will demonstrate adequate peripheral tissue perfusion as evidenced by warm extremities, strong peripheral pulses, and capillary refill <3 seconds
- Patient will maintain normal skin color in extremities
- Patient will report normal sensation in extremities
| Nursing Interventions | Rationales |
|---|---|
| Assess peripheral circulation every 2-4 hours or more frequently if unstable (pulses, capillary refill, skin color, temperature, sensation) | Provides ongoing evaluation of peripheral perfusion status and effectiveness of interventions |
| Document findings using consistent method (e.g., pulses on scale of 0-4+) | Ensures accurate trending of peripheral perfusion status over time |
| Position patient to avoid pressure on extremities; change position at least every 2 hours | Prevents pressure injury when peripheral circulation is already compromised |
| Avoid elevation of legs unless specifically ordered | Elevation may further compromise arterial flow in poorly perfused extremities |
| Maintain normothermia; avoid cooling extremities | Cold extremities can cause vasoconstriction, further decreasing peripheral blood flow |
| Administer IV fluids as prescribed | Volume expansion can temporarily improve cardiac output and peripheral perfusion until definitive treatment |
| Avoid constrictive clothing or devices on extremities | Prevents further compromise of peripheral circulation |
| Assist with range of motion exercises for extremities if patient is stable | Promotes circulation and prevents venous stasis |
| Prepare for pericardiocentesis or surgical intervention | Definitive treatment to improve cardiac output and restore peripheral perfusion |
| Monitor for signs of tissue ischemia (severe pain, paralysis, paresthesia, pallor, pulselessness) | These are signs of critical limb ischemia requiring immediate intervention |
Evaluation:
- Peripheral pulses become stronger and easily palpable
- Capillary refill time improves to <3 seconds
- Extremities become warm to touch
- Normal skin color returns to extremities
- Patient reports normal sensation in extremities
- Peripheral edema decreases if present
Nursing Care Plan 11: Excess Fluid Volume
Assessment Findings/Defining Characteristics:
- Jugular venous distention
- Edema (peripheral, sacral)
- Weight gain
- Increased central venous pressure
- Shortness of breath
- Decreased urine output
- Pleural effusion (if present)
- Ascites (if present)
- S3 heart sound (if heart failure develops)
Expected Outcomes:
- Patient will demonstrate improved fluid balance as evidenced by decreased edema, normal jugular venous pressure, and improved urine output
- Patient will maintain stable weight within target range
- Patient will verbalize decreased shortness of breath
| Nursing Interventions | Rationales |
|---|---|
| Monitor intake and output strictly; calculate fluid balance every shift | Provides objective measurement of fluid status and effectiveness of interventions |
| Weigh patient daily at same time, using same scale and clothing | Weight is a sensitive indicator of fluid status; 1 kg weight change represents approximately 1 L fluid |
| Assess for peripheral edema, jugular venous distention, and other signs of fluid overload every 4 hours | Early detection of worsening fluid status allows for prompt intervention |
| Monitor electrolytes, BUN, and creatinine | Fluid shifts can affect electrolyte balance; renal function affects fluid elimination |
| Position patient in semi-Fowler’s or high Fowler’s position | Improves breathing and decreases venous return to heart, reducing cardiac workload |
| Administer diuretics as prescribed | Promotes fluid excretion to reduce overall fluid volume |
| Implement sodium restriction as ordered | Sodium restriction decreases fluid retention |
| Monitor central venous pressure if central line is in place | Provides direct measurement of right atrial filling pressure and effectiveness of fluid management |
| Prepare for pericardiocentesis or surgical intervention | Definitive treatment to remove excess pericardial fluid |
| Educate patient about fluid and sodium restrictions if applicable | Promotes patient participation in fluid management |
Evaluation:
- Peripheral edema decreases or resolves
- Jugular venous distention decreases
- Weight returns to baseline or target range
- Urine output improves to >30 ml/hr
- Patient reports decreased shortness of breath
- Fluid balance shows appropriate trending toward normal
- Central venous pressure returns to normal range (2-6 mmHg)
Nursing Care Plan 12: Readiness for Enhanced Knowledge
Assessment Findings/Defining Characteristics:
- Expresses interest in learning about condition
- Asks questions about management strategies
- Seeks information about preventing recurrence
- Expresses desire to manage care at home
- Demonstrates readiness to participate in health maintenance
- Engaged in learning process
Expected Outcomes:
- Patient will demonstrate comprehensive understanding of underlying condition causing cardiac tamponade
- Patient will identify strategies to manage underlying condition
- Patient will verbalize understanding of follow-up care requirements
- Patient will demonstrate self-monitoring skills relevant to underlying condition
- Patient will utilize available resources for continued learning and support
| Nursing Interventions | Rationales |
|---|---|
| Assess knowledge of underlying condition (e.g., malignancy, autoimmune disorder, infection) that caused cardiac tamponade | Establishes baseline understanding and identifies knowledge gaps |
| Provide information about underlying condition, treatment options, and prognosis | Accurate information empowers patient to make informed decisions about healthcare |
| Teach specific management strategies for underlying condition (e.g., medication management for autoimmune disorders, follow-up care for malignancies) | Proper management of underlying condition reduces risk of tamponade recurrence |
| Provide information about warning signs of recurrent tamponade | Early recognition enables prompt intervention before severe compromise occurs |
| Teach self-monitoring techniques relevant to underlying condition | Active participation in monitoring improves early detection of complications |
| Provide information about community resources and support groups specific to underlying condition | Connects patient with additional learning opportunities and emotional support |
| Encourage patient to maintain a health journal to track symptoms and responses to treatments | Promotes self-awareness and provides valuable information for healthcare providers |
| Review follow-up appointment schedule and importance of adherence | Regular monitoring by healthcare providers is essential for managing chronic conditions that can cause tamponade |
| Provide reliable sources for additional information (websites, books, patient education materials) | Facilitates continued learning from accurate sources |
| Involve family members or support persons in education sessions | Support system knowledge enhances patient adherence and provides additional monitoring |
Evaluation:
- Patient accurately describes underlying condition and its relationship to cardiac tamponade
- Patient demonstrates understanding of management strategies for underlying condition
- Patient identifies warning signs requiring medical attention
- Patient verbalizes plan for follow-up care
- Patient demonstrates ability to access and utilize community resources
- Patient shows engagement in self-care activities
Conclusion
Cardiac tamponade is a life-threatening emergency that requires prompt recognition and intervention. Nurses play a critical role in the assessment, management, and education of patients with this condition. The 12 nursing care plans outlined in this guide provide a comprehensive approach to addressing the multifaceted needs of patients with cardiac tamponade.
Key aspects of nursing care include continuous monitoring of hemodynamic status, supporting respiratory function, managing pain and anxiety, preventing complications, and providing thorough patient education. Early detection of cardiac tamponade through recognition of Beck’s triad (hypotension, jugular venous distention, and muffled heart sounds) and other clinical manifestations is essential for timely intervention.
By implementing these evidence-based nursing care plans, nurses can significantly improve outcomes for patients with cardiac tamponade. Understanding the pathophysiology, clinical presentation, and management strategies enables nurses to provide high-quality care during this critical medical emergency and throughout the recovery process.
© 2025 Nursing Education Resource | Cardiac Tamponade Nursing Care Plans
