Fetal Development, Growth, Circulation, and Nutrition
Comprehensive Nursing Notes
Introduction
Understanding fetal development is crucial for nursing students specializing in maternal and child health. These notes provide a comprehensive overview of fetal growth, development, circulation, and nutrition from conception to birth. The knowledge of normal fetal development helps nurses recognize abnormalities, provide appropriate counseling, and deliver optimal care for pregnant women and their developing babies.
Learning Tip:
Throughout this resource, look for color-coded information about blood oxygenation in fetal circulation:
- Oxygenated blood (red)
- Deoxygenated blood (blue)
- Mixed blood (purple)
Table of Contents
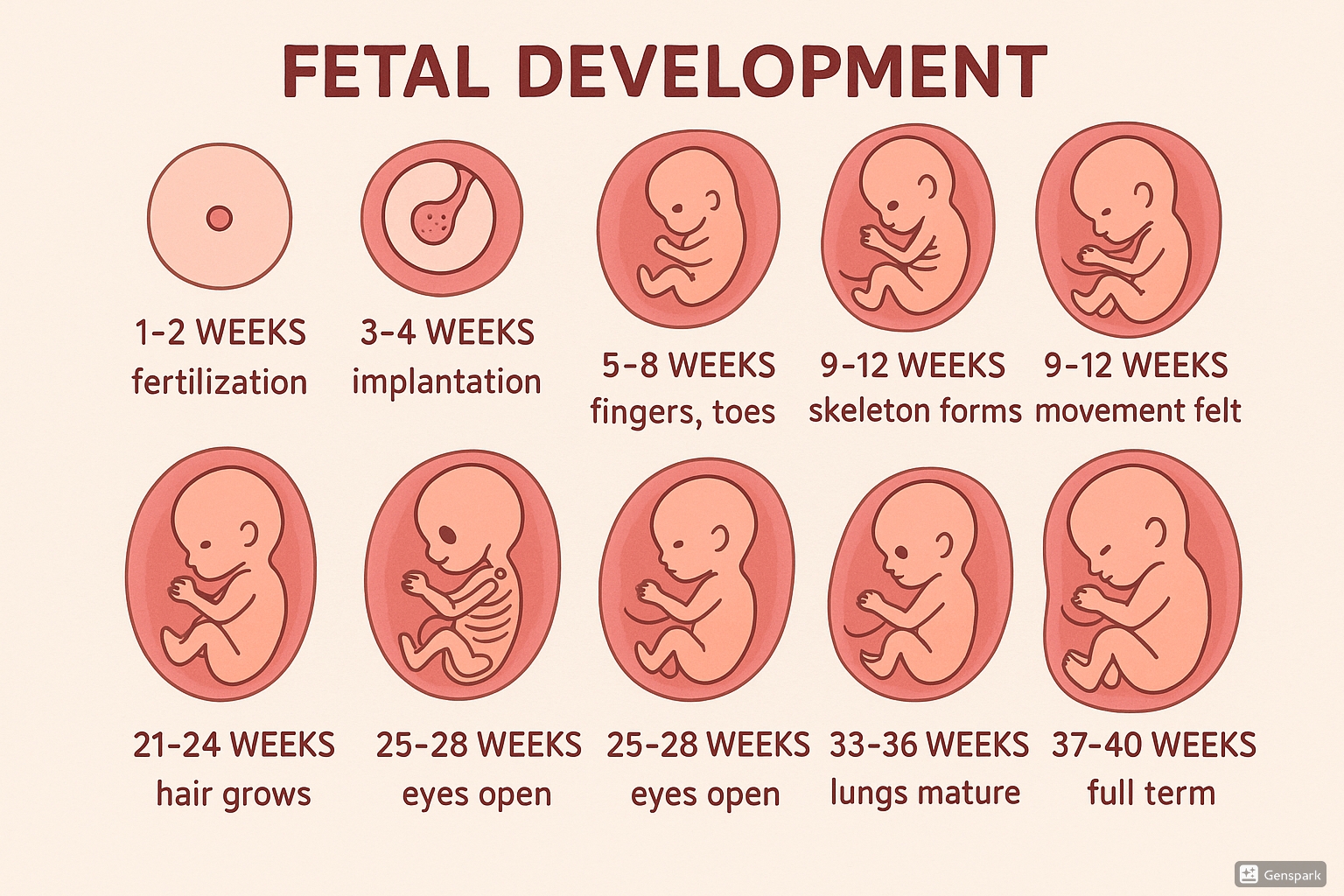
Figure 1: Stages of fetal development from weeks 1-40 showing key developmental milestones.
Stages of Fetal Development
Fetal development is a continuous process that begins at fertilization and ends at birth. It can be divided into three main stages:
| Stage | Duration | Key Events |
|---|---|---|
| Germinal | Fertilization to Week 2 | Fertilization, cell division (cleavage), blastocyst formation, implantation |
| Embryonic | Weeks 3-8 | Gastrulation, formation of three germ layers, organogenesis, basic body structure forms |
| Fetal | Week 9 to Birth | Continued growth and development of organs, systems maturation, preparation for extrauterine life |
During the germinal stage, after fertilization, the zygote undergoes rapid cell division as it travels through the fallopian tube toward the uterus. By day 5-6, a blastocyst forms, consisting of an inner cell mass (which becomes the embryo) and outer trophoblast cells (which contribute to placenta formation). Implantation begins around day 6-7 when the blastocyst attaches to the uterine lining.
Key Point: The germinal stage establishes the foundation for further development. Any disruptions during this period may result in failure of implantation or early pregnancy loss.
Embryonic Development (Weeks 3-8)
The embryonic period is characterized by rapid development and is the most critical time for organ formation. During this phase, the embryo is most vulnerable to teratogens that can cause congenital anomalies.
Organogenesis
Organogenesis begins in week 3 with gastrulation, which establishes the three primary germ layers:
- Ectoderm: Forms the nervous system, sensory organs, skin epidermis, hair, nails
- Mesoderm: Develops into muscles, bones, circulatory system, kidneys, gonads
- Endoderm: Creates the lining of digestive and respiratory tracts, liver, pancreas, thyroid
Mnemonic: “EEM” – Remember what each germ layer forms
Ectoderm → External coverings & nervous system
Endoderm → Enteric (gut) & respiratory linings
Mesoderm → Muscles, bones & Middle structures
Critical Periods of Development
Each organ system has a critical period during which it is most susceptible to disruption. The timeline below highlights key developmental events during the embryonic period:
Week 3
Neural tube formation begins (precursor to brain and spinal cord)
Heart tube begins to form and starts beating by the end of week
Week 4
Four limb buds appear
Heart now has four chambers and is beating
Basic facial features begin to form
Week 5
Eyes, ears, and nose start forming
Limb buds grow longer and have distinct hand and foot regions
Week 6
Fingers and toes begin to form (still webbed)
Brain differentiates into five areas
Primitive intestines relocate from yolk sac to embryo
Week 7
Digits separate and are no longer webbed
All essential organs have begun to form
Week 8
All major organs and external structures are formed
Embryo now has distinct human characteristics
End of embryonic period; now called a fetus
Clinical Alert:
The embryonic period (weeks 3-8) is when the embryo is most susceptible to teratogens that can cause structural birth defects. Exposure to certain medications, alcohol, radiation, or infections during these critical weeks can significantly impact organ development.
Fetal Growth and Maturation (Weeks 9-40)
After week 8, the embryo is referred to as a fetus. The fetal period is characterized by rapid growth, refinement of organ systems, and preparation for extrauterine life. During this period, the fetus grows from about 3 cm to approximately 50 cm in length.
First Trimester (Weeks 9-12)
- External genitalia begin to differentiate
- Kidneys begin producing urine
- Fetal heartbeat detectable via Doppler (around week 10-12)
- Reflexive movements begin but are too small to be felt by mother
- By week 12, the fetus is about 7.5 cm long and weighs approximately 28 grams
Second Trimester (Weeks 13-27)
- Sex can be distinguished via ultrasound (usually by week 16-20)
- Quickening occurs (mother feels fetal movement, typically weeks 16-20)
- Vernix caseosa (waxy coating) and lanugo (fine hair) develop on skin
- Eyebrows and eyelashes form
- Fingerprints and footprints develop
- By week 24, the fetus weighs about 600 grams and measures 28-30 cm
- Lungs begin producing surfactant (crucial for breathing after birth)
Third Trimester (Weeks 28-40)
- Periods of sleep and wakefulness become more defined
- Eyes can open and close
- Brain growth accelerates dramatically
- Subcutaneous fat deposits increase (important for thermoregulation)
- Lungs continue to mature
- Fetus assumes birth position (usually head down by weeks 36-38)
- At birth (week 40), average weight is 3400 grams and length is 48-52 cm
Growth Assessment Tip:
Remember the Rule of 4’s for average fetal growth in the second half of pregnancy:
- 16 weeks: ~16 cm, ~160 grams
- 20 weeks: ~20 cm, ~400 grams
- 24 weeks: ~24 cm, ~600 grams
- 28 weeks: ~28 cm, ~1000 grams
- Growth accelerates after 28 weeks
| Developmental Milestone | Timing (Weeks) | Clinical Significance |
|---|---|---|
| Heartbeat detectable via ultrasound | 6-7 weeks | Confirms viable pregnancy |
| Heartbeat detectable via Doppler | 10-12 weeks | Routine prenatal assessment |
| Quickening | 16-20 weeks | Confirms active fetus |
| Viability threshold | 24 weeks | Potential survival outside uterus with intensive care |
| Surfactant production | 24-28 weeks | Crucial for respiratory function |
| Major organ systems mature | 37 weeks | Considered full-term |
Fetal Circulation
Fetal development depends on a specialized circulatory system that differs significantly from postnatal circulation. The fetal circulation is designed to bypass the non-functioning lungs and optimize oxygenation via the placenta.
Fetal Shunts
Three major vascular shunts distinguish fetal circulation from postnatal circulation:
| Shunt | Location | Function | Post-Birth Change |
|---|---|---|---|
| Ductus Venosus | Connects umbilical vein to inferior vena cava | Allows oxygenated blood to bypass the liver | Closes within a week after birth, becomes ligamentum venosum |
| Foramen Ovale | Opening between right and left atria | Allows blood to bypass the pulmonary circulation | Functional closure at birth, anatomical closure within 3 months, becomes fossa ovalis |
| Ductus Arteriosus | Connects pulmonary artery to aorta | Diverts blood away from non-functioning lungs | Functional closure within 24-48 hours, anatomical closure within 2-3 weeks, becomes ligamentum arteriosum |
Mnemonic: “DVD FLAP” – Remember Fetal Shunts and Their Post-Birth Fate
Ductus Venosus → becomes Dead (Ligamentum venosum)
Foramen Ovale → becomes Fossa ovalis
Ductus Arteriosus → becomes Ligamentum Arteriosum Permanently
Blood Flow Pathway
The pathway of blood flow through the fetal circulation is as follows:
- Oxygenated blood from the placenta enters the fetus via the umbilical vein
- About 50% of this blood bypasses the liver through the ductus venosus and enters the inferior vena cava
- Blood enters the right atrium and is preferentially directed through the foramen ovale into the left atrium
- From the left atrium, blood enters the left ventricle and is pumped into the ascending aorta, supplying the brain and upper body with relatively oxygen-rich blood
- Deoxygenated blood returning from the upper body enters the right atrium via the superior vena cava
- This blood flows into the right ventricle and out through the pulmonary artery
- Most of this blood bypasses the lungs by flowing through the ductus arteriosus into the descending aorta, creating mixed oxygenation blood
- Blood returns to the placenta for reoxygenation via two umbilical arteries
Key Concept: The fetus receives the most highly oxygenated blood to its brain, heart, and upper body, while the lower body receives blood with lower oxygen content. This preferential circulation is crucial for proper brain and cardiac development.
Circulatory Changes at Birth
At birth, dramatic circulatory changes occur as the newborn transitions to extrauterine life:
- First breath: Lung expansion decreases pulmonary vascular resistance and increases pulmonary blood flow
- Umbilical cord clamping: Eliminates placental circulation, increasing systemic vascular resistance
- Foramen ovale closure: Increased left atrial pressure functionally closes this shunt
- Ductus arteriosus closure: Increased arterial oxygen triggers constriction within 24-48 hours
- Ductus venosus closure: Occurs within a week after birth
Clinical Alert:
Persistent fetal circulation pathways can lead to significant health issues:
- Patent ductus arteriosus (PDA) can cause left-to-right shunting and heart failure
- Patent foramen ovale (PFO) may be asymptomatic but can increase risk of paradoxical emboli
- Premature infants are at higher risk for persistent fetal circulation due to immature cardiovascular development
Fetal Nutrition
Proper fetal development depends on adequate nutrition supplied through the placenta. The placenta serves as the interface between maternal and fetal circulation, facilitating nutrient transfer and waste removal.
Placental Function
The placenta performs numerous critical functions throughout pregnancy:
| Function | Description |
|---|---|
| Gas Exchange | Provides oxygen and removes carbon dioxide via diffusion across the placental membrane |
| Nutrient Transfer | Facilitates transport of glucose, amino acids, fatty acids, vitamins, and minerals from mother to fetus |
| Waste Elimination | Removes metabolic waste products from fetal circulation |
| Endocrine Function | Produces hormones including human chorionic gonadotropin (hCG), estrogen, progesterone, human placental lactogen (hPL) |
| Immune Protection | Transfers maternal IgG antibodies to fetus; serves as barrier against many pathogens |
| Metabolic Activity | Metabolizes some substances before they reach the fetus; synthesizes glycogen, cholesterol, and fatty acids |
Development Timeline: The placenta begins forming shortly after implantation but isn’t fully functional until around week 12. Before this time, the developing embryo receives nutrients through diffusion from the endometrial glands and maternal blood.
Nutrient Transfer Mechanisms
The placenta uses several transport mechanisms to transfer nutrients from maternal to fetal circulation:
- Simple Diffusion: Passive movement of oxygen, carbon dioxide, water, and some lipid-soluble substances
- Facilitated Diffusion: Carrier-mediated transport that doesn’t require energy; used for glucose transport via GLUT transporters
- Active Transport: Energy-dependent process that moves substances against concentration gradients; used for amino acids, some ions
- Receptor-Mediated Endocytosis: Transfers large molecules like maternal antibodies (IgG) and lipoproteins
- Vesicular Transport: Movement of substances within membrane-bound vesicles
Mnemonic: “SAFER” – Remember Placental Transport Mechanisms
Simple diffusion (gases, water, lipid-soluble substances)
Active transport (amino acids, ions)
Facilitated diffusion (glucose)
Endocytosis (antibodies, lipoproteins)
Receptor-mediated transport (specific proteins)
Key Nutrients for Fetal Development
| Nutrient | Importance in Fetal Development | Transfer Mechanism |
|---|---|---|
| Glucose | Primary energy source for fetus | Facilitated diffusion via GLUT transporters |
| Amino Acids | Protein synthesis, neurodevelopment | Active transport; concentrations higher in fetus than mother |
| Fatty Acids | Brain development, myelin formation, adipose tissue | Diffusion and carrier-mediated transport |
| Iron | Hemoglobin synthesis, oxygen transport, brain development | Active transport via transferrin receptors |
| Calcium | Bone mineralization, cellular functions | Active transport; increases in third trimester |
| Folate | DNA synthesis, cell division, neural tube development | Active transport; concentrated in fetal circulation |
| Vitamin D | Calcium metabolism, bone development | Simple diffusion of metabolites |
Nutritional Considerations for Nurses:
Maternal nutritional status directly impacts fetal growth and development. Specific concerns include:
- Inadequate folate intake: Increased risk of neural tube defects
- Iron deficiency: Can lead to fetal anemia and growth restriction
- Protein deficiency: Associated with intrauterine growth restriction
- Vitamin D deficiency: Poor bone mineralization, increased risk of neonatal hypocalcemia
Clinical Implications for Nursing
Understanding normal fetal development helps nurses identify potential abnormalities and provide appropriate care and education to pregnant women.
Assessment and Monitoring
- Fundal Height Measurement: Should correlate with gestational age in centimeters from 20-36 weeks
- Fetal Movement Counting: Women should feel at least 10 movements in a 2-hour period
- Auscultation of Fetal Heart Rate: Normal range is 110-160 beats per minute
- Ultrasound Assessment: Used to confirm dating, assess anatomy, monitor growth, and evaluate well-being
Patient Education
- Nutrition: Counsel on adequate intake of protein, iron, calcium, folate, and other essential nutrients
- Teratogens: Educate about avoiding alcohol, tobacco, recreational drugs, and certain medications
- Fetal Movement: Teach importance of monitoring and when to report changes
- Warning Signs: Instruct on signs that require immediate medical attention (vaginal bleeding, decreased fetal movement, severe abdominal pain)
Common Pathological Conditions
Knowledge of normal development helps nurses identify abnormal conditions:
| Condition | Description | Nursing Considerations |
|---|---|---|
| Intrauterine Growth Restriction (IUGR) | Fetal weight below 10th percentile for gestational age | Frequent monitoring, education about optimal nutrition, assessment for underlying causes |
| Macrosomia | Birth weight >4000g or above 90th percentile | Screen for gestational diabetes, prepare for potential birth complications |
| Congenital Anomalies | Structural or functional abnormalities present at birth | Emotional support, referral to specialists, education about management |
| Placental Insufficiency | Inadequate placental function affecting fetal growth and well-being | Monitoring of fetal growth, movement, and heart rate patterns; preparation for possible early delivery |
| Fetal Anemia | Abnormally low hemoglobin in fetus | Monitor for hydrops fetalis, prepare for potential intrauterine transfusion |
| Oligohydramnios | Decreased amniotic fluid volume | Monitor for fetal distress, assess for maternal hydration, prepare for possible early delivery |
Global Best Practices
Several evidence-based approaches to optimize fetal development and outcomes have been implemented worldwide:
Finland’s Neuvola System
Finland has one of the lowest infant mortality rates globally, partly due to its comprehensive prenatal care system called “Neuvola”:
- Free prenatal care for all pregnant women
- First visit before 8 weeks gestation
- 10-15 visits during pregnancy with a dedicated nurse
- Comprehensive screening and monitoring
- Focus on maternal nutrition and well-being
- Home visits after delivery
CenteringPregnancy® Model
This group-based model of prenatal care has shown positive outcomes in various countries:
- Combines health assessment, education, and support
- Groups of 8-12 women with similar due dates meet regularly
- Improved birth weights and decreased preterm births
- Enhanced maternal knowledge about fetal development
- Greater satisfaction with prenatal care
Chile’s Prenatal Care Program
Chile dramatically reduced maternal and infant mortality through its comprehensive approach:
- Universal access to prenatal care
- Fortification of flour with folic acid to prevent neural tube defects
- Maternal nutritional supplementation program
- Early detection of high-risk pregnancies
- Professional attendance at birth
Implementation Tip for Nurses:
Elements from these global best practices can be incorporated into nursing care:
- Emphasize early and regular prenatal care
- Provide detailed education about fetal development milestones
- Conduct thorough nutritional assessments and counseling
- Consider group-based education when possible
- Pay special attention to vulnerable populations
Conclusion
Understanding the intricacies of fetal development, circulation, and nutrition is essential for nursing students specializing in maternal and child health. This knowledge provides the foundation for assessment, monitoring, patient education, and early detection of abnormalities.
The remarkable journey from a single cell to a fully formed infant involves complex processes that are vulnerable to disruption. Nurses play a vital role in supporting optimal conditions for development through education, monitoring, and timely intervention when needed.
By applying this knowledge in clinical practice, nurses can contribute significantly to maternal and fetal health, ultimately improving outcomes for the next generation.
References
- Cleveland Clinic. (2022). Fetal Development: Stages of Growth. https://my.clevelandclinic.org/health/articles/7247-fetal-development-stages-of-growth
- Mayo Clinic. (n.d.). Fetal development: The first trimester. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20045302
- American Heart Association. (n.d.). Fetal Circulation. https://www.heart.org/en/health-topics/congenital-heart-defects/symptoms–diagnosis-of-congenital-heart-defects/fetal-circulation
- National Center for Biotechnology Information. (2020). Physiology, Fetal Circulation. https://www.ncbi.nlm.nih.gov/books/NBK539710/
- National Center for Biotechnology Information. (2020). Embryology, Placenta. https://www.ncbi.nlm.nih.gov/books/NBK551634/
- National Center for Biotechnology Information. (2022). Embryology, Weeks 6-8. https://www.ncbi.nlm.nih.gov/books/NBK563181/
- NCBI PubMed. (n.d.). Maternal–Fetal Nutrient Transport in Pregnancy Pathologies. https://pmc.ncbi.nlm.nih.gov/articles/PMC4200776/
- NCBI PubMed. (n.d.). Understanding placental nutrient transfer. https://pmc.ncbi.nlm.nih.gov/articles/PMC2742272/
