Labor Room Organization: Triage, Birth Preparation & Positive Birth Environment
Comprehensive nursing notes designed for nursing students
Table of Contents
1. Introduction
Proper labor room organization is a fundamental aspect of providing safe, efficient, and compassionate care during childbirth. The physical layout, equipment preparedness, and overall environment of the labor room significantly impact the birth experience for the mother, her family, and healthcare providers. This comprehensive guide focuses on three critical aspects of labor room organization: triage protocols, birth preparation, and creating positive birth environments.
The labor room, often referred to as the Labor Delivery Room (LDR), serves as one of the hospital’s most versatile spaces, designed to accommodate various types of deliveries. Whether a woman is undergoing an unmedicated birth or receiving an epidural, the labor room must be fully equipped and properly organized to ensure optimal outcomes and positive experiences.
Learning Objectives
- Understand the key principles of effective labor room organization and layout
- Apply evidence-based triage protocols for obstetric patients
- Prepare delivery equipment and resources following standardized protocols
- Implement strategies to create a positive birth environment
- Identify emergency resources and establish preparedness protocols
2. Labor Room Organization & Layout
Effective labor room organization requires careful consideration of spatial design, equipment placement, and workflow optimization. A well-organized labor room facilitates efficient care delivery, promotes safety, and contributes to a positive birthing experience.
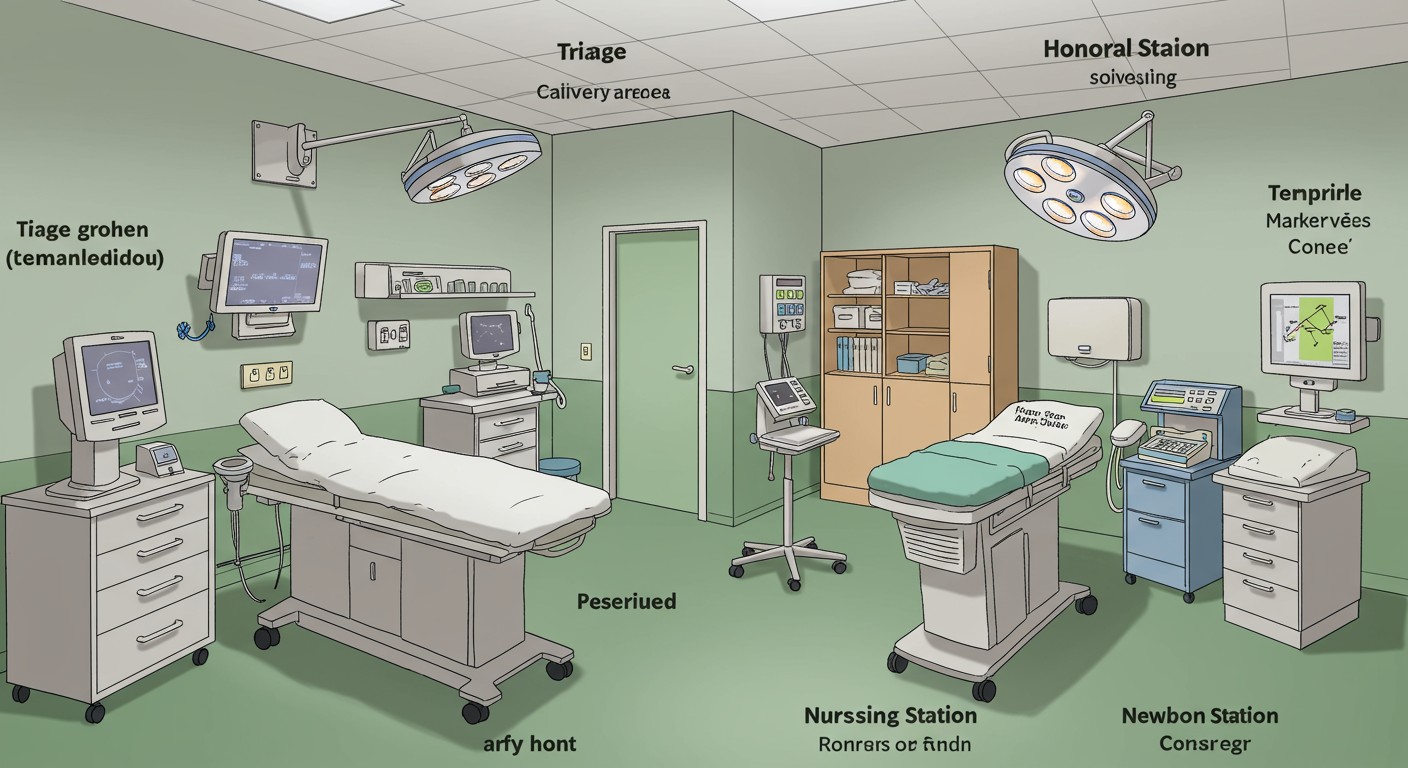
Figure 1: Standard Labor Room Organization with Triage Area, Delivery Area, and Nursing Station
Standard Labor Room Layout
According to established guidelines, a standard labor room organization includes:
- Four labor areas with one labor table each
- A central nursing station for continuous monitoring
- A dedicated newborn care area
- Two toilets and two washing areas for hygiene maintenance
- Adequate space between delivery tables to ensure privacy and infection control
Labor Area Specifications
Key Specifications for Each Labor Area
- Size: Approximately 10 × 10 feet (3 × 3 meters)
- Partitioning: Opaque partitions between consecutive labor areas extending to ceiling height (opaque up to 6.5 feet)
- Equipment: One labor table per area with specifications as per standards
- Seating: One stool for birth companion
- Climate control: Adequate lighting, ventilation, and ceiling/wall-mounted fan
- Privacy: Two curtains extending from doorway to partition walls
Functional Zones in Labor Room
A well-organized labor room incorporates distinct functional zones to facilitate efficient workflow:
| Zone | Purpose | Key Features |
|---|---|---|
| Triage Area | Initial assessment and prioritization | Examination bed, monitoring equipment, privacy screens |
| Delivery Area | Active labor and birth | Delivery table, equipment trays, emergency supplies |
| Nursing Station | Monitoring and documentation | Computers, monitoring displays, communication systems |
| Newborn Care Corner | Immediate newborn care | Radiant warmer, resuscitation equipment, examination area |
| Storage Zone | Equipment and supply storage | Cabinets, shelving, easily accessible essential supplies |
| Family Area | Support person accommodation | Seating, personal item storage, amenities for comfort |
The ideal labor room organization balances clinical efficiency with patient comfort. Proper lighting (500 Lx for labor areas), adequate ventilation, and temperature control (24-26°C) are essential environmental considerations that contribute to both staff productivity and patient experience.
3. Triage Protocols
Triage is a critical component of labor room organization that ensures patients receive care according to acuity rather than arrival time. Effective triage protocols streamline patient flow, optimize resource allocation, and improve clinical outcomes.
Definition of Obstetric Triage
Obstetric triage is a systematic process of assessing pregnant patients to determine the urgency of care required and appropriate resource allocation. It serves as the entry point to labor and delivery services for many women, with triage volume typically exceeding overall birth volume by 20-50%.
3.1 Triage Assessment
The initial triage assessment should be performed by qualified personnel designated by hospital policy, which may include registered nurses, certified nurse-midwives, nurse practitioners, physician assistants, or physicians. The assessment includes:
Initial Assessment Components
- Chief complaint evaluation
- Brief medical and obstetric history
- Vital signs (maternal temperature, blood pressure, pulse, respiratory rate, pain level)
- Fetal heart rate assessment
- Contraction pattern evaluation
- Assessment for rupture of membranes
- Vaginal bleeding assessment
Common Triage Presentations
- Labor (term or preterm)
- Decreased fetal movement
- Vaginal bleeding
- Rupture of membranes
- Hypertension/preeclampsia
- Acute abdominal pain
- Trauma
- General pregnancy concerns
Mnemonic: “MATERNAL”
Key components of obstetric triage assessment:
- M – Maternal vital signs
- A – Abdominal evaluation (contractions, pain)
- T – Timing (of contractions, symptoms)
- E – Environment assessment for safety
- R – Rupture of membranes evaluation
- N – Neonatal status (fetal heart rate, movement)
- A – Additional symptoms assessment
- L – Labor progress evaluation
3.2 Triage Acuity Systems
Evidence-based triage acuity tools improve the efficiency and quality of obstetric triage by prioritizing patients according to urgency rather than arrival time. The Maternal-Fetal Triage Index (MFTI) is a validated five-level classification system:
| Priority Level | Response Time | Clinical Conditions |
|---|---|---|
| Level 1: Stat | Immediate | Prolapsed cord, seizure, shoulder dystocia, umbilical cord prolapse, severe vaginal bleeding, maternal cardiac arrest |
| Level 2: Urgent | ≤ 10 minutes | Active labor, moderate vaginal bleeding, severe hypertension, decreased fetal movement with non-reassuring fetal heart tones |
| Level 3: Prompt | ≤ 30 minutes | Early labor, mild preeclampsia, ROM with clear fluid, controlled diabetes |
| Level 4: Non-Urgent | ≤ 60 minutes | Latent labor, mild pregnancy symptoms, routine NST, BP check |
| Level 5: Scheduled | ≤ 120 minutes | Scheduled procedures, non-urgent visits |
Implementing standardized acuity tools as part of labor room organization has been shown to reduce time-to-provider evaluation and improve patient outcomes, particularly for high-acuity cases.
3.3 Triage Workflow
An efficient triage workflow is essential for proper labor room organization and optimizing patient care. The recommended workflow includes:
- Initial Contact: Patient arrives or calls labor and delivery unit
- Registration: Quick registration process while maintaining privacy
- Primary Assessment: Rapid evaluation by triage nurse to determine acuity
- Acuity Assignment: Categorization using standardized acuity tool
- Detailed Assessment: Complete maternal-fetal assessment based on presenting concerns
- Provider Evaluation: Assessment by appropriate healthcare provider within timeframe determined by acuity level
- Plan Development: Creation of care plan (admit, observe, discharge)
- Execution: Implementation of care plan with clear communication
EMTALA Considerations in Obstetric Triage
Labor and delivery units must adhere to Emergency Medical Treatment and Labor Act (EMTALA) requirements, including:
- Providing appropriate medical screening examination to determine if an emergency medical condition exists
- Considering both maternal and fetal health in assessment
- Stabilizing the patient or arranging appropriate transfer when necessary
- Never delaying screening or treatment to inquire about payment method or insurance
A woman in labor is considered unstable from latent phase through placenta delivery if there is inadequate time for safe transfer or if transfer poses a threat to maternal or fetal health.
4. Birth Preparation
Effective birth preparation is a crucial element of labor room organization, ensuring that all necessary equipment and supplies are readily available, properly arranged, and in optimal working condition. Thorough preparation facilitates smooth delivery processes and enables rapid response to emergencies.
4.1 Delivery Table Setup
Proper setup of the delivery table is fundamental to birth preparation in labor room organization. The following steps should be followed:
- Hand hygiene: Thorough handwashing following standard protocols
- Personal protective equipment: Don cap, gown, mask as per hospital policy
- Surface preparation: Place sterile delivery pack on a flat surface above waist level
- Asepsis maintenance: Maintain strict aseptic technique throughout setup
- Delivery table preparation: Place mackintosh sheet on the delivery table
- Equipment verification: Check all equipment functionality
Mnemonic: “STERILE”
For delivery table setup:
- S – Scrub hands thoroughly
- T – Table position check (appropriate height and inclination)
- E – Equipment verification
- R – Ready sterile field
- I – Instruments arranged in order of use
- L – Linens and mackintosh placement
- E – Ensure all items are within reach
4.2 Essential Equipment & Supplies
A well-organized labor room must be equipped with all necessary supplies and equipment, systematically arranged for quick access. The following equipment categories are essential components of proper labor room organization:
| Category | Essential Items |
|---|---|
| Bed and Furniture | Delivery table with leg supports, bedside trolley, IV stand, stainless steel stool, Kelly’s pad |
| Monitoring Equipment | Doppler (fetal heart rate) machine, ECG machine with accessories, blood pressure apparatus, thermometer |
| Emergency Equipment | Defibrillator with accessories, adult resuscitation set, newborn resuscitation set, oxygen cylinder with accessories |
| Delivery Sets | Normal delivery instruments, episiotomy set, incisional set, dressing trolley with articles |
| Infection Control | BMW set, GW set, spillage set, sterilization equipment |
| Specialized Kits | Eclampsia first aid kit, PPH management kit, emergency drug tray/crash cart |
| Lighting and Suction | Focus light, manual suction machine, central suction supply port |
Examination Tray Contents
- Bowl with cotton swabs
- Sterile gloves
- Antiseptic solution
- Measuring tape
- Stethoscope/fetoscope
- Blood pressure apparatus
- Thermometer
- Blood and urine collection supplies
Essential Surgical Instruments
- Vaginal speculum – for examination
- Artery forceps – for clamping vessels and holding sutures
- Needle holders – for grasping needles during suturing
- Sponge holders – for applying antiseptic solutions
- Thumb forceps – for tissue manipulation
- Scissors (straight and curved) – for cutting sutures and tissues
- Cord ties – for securing the umbilical cord
- Retractors – for improved visualization
Newborn Care Corner Equipment
- Radiant warmer
- Neonatal Ambu bag
- Mucus extractor
- Infant tray with clean cloth
- Oxygen supply with appropriate attachments
- Nasal catheter
- Laryngoscope
- Pediatric stethoscope
4.3 Emergency Preparedness
Emergency preparedness is a vital aspect of labor room organization, ensuring rapid response to critical situations. Key components include:
Emergency Drug Tray Contents
- Oxytocin injection – For labor induction and postpartum hemorrhage management
- Methylergometrine – For management of postpartum hemorrhage
- Diazepam injection – For anxiety management and eclampsia treatment
- Magnesium sulfate – For preeclampsia/eclampsia management
- Calcium gluconate – Antidote for magnesium toxicity
- Hydralazine/Labetalol – For hypertension management
- Epinephrine – For anaphylaxis and cardiac resuscitation
- IV fluids – Normal saline, Ringer’s lactate
Emergency Response Planning
A well-organized labor room must incorporate clear emergency protocols:
- Designated emergency signal system
- Clearly displayed emergency protocols for common obstetric emergencies
- Regular drills for emergency scenarios (hemorrhage, shoulder dystocia, eclampsia)
- Clear delegation of team member roles during emergencies
- Established communication protocols with other departments
- Accessible emergency equipment with regular verification of functionality
Mnemonic: “PREPARE”
For emergency readiness in labor room:
- P – Protocols clearly displayed
- R – Resuscitation equipment checked
- E – Emergency drugs readily available
- P – Practice emergency drills
- A – Assign team roles
- R – Review equipment daily
- E – Ensure communication systems function
5. Creating a Positive Birth Environment
Creating a positive birth environment is an increasingly recognized component of quality maternity care and optimal labor room organization. Research demonstrates that the physical environment can significantly impact birthing outcomes, maternal satisfaction, and physiological labor progress.
Benefits of a Positive Birth Environment
- Reduced stress and anxiety
- Enhanced natural oxytocin production
- Decreased perception of pain
- Improved progress of labor
- Reduced need for medical interventions
- Increased maternal satisfaction
- Improved initial bonding experiences
5.1 Environmental Factors
Several environmental factors contribute to a positive birth experience as part of effective labor room organization:
| Factor | Recommendations | Physiological Impact |
|---|---|---|
| Lighting | Dimmable lights, option for natural light, ability to create low-light environments | Bright lights can inhibit oxytocin release and increase stress hormones |
| Privacy | Soundproofing, privacy screens, limited entry/exit, knocking policies | Privacy promotes hormonal balance conducive to labor progression |
| Temperature | Adjustable room temperature (24-26°C), available blankets, portable fans | Thermal comfort reduces stress and promotes relaxation |
| Spaciousness | Room for movement and various positions, space for support persons | Freedom of movement facilitates fetal descent and maternal comfort |
| Room Layout | Bed not central focus, home-like elements, space for active labor | Non-medical appearance reduces anxiety and promotes normality |
| Aesthetics | Calming colors, nature elements, minimal clinical appearance when possible | Visual environment affects stress levels and emotional state |
Research indicates that birthing rooms with calming design elements can contribute to reduced cesarean rates, decreased use of augmentation, and improved maternal satisfaction.
5.2 Sensory Considerations
A comprehensive approach to labor room organization addresses all sensory aspects of the environment:
Visual Elements
- Calming artwork, particularly nature scenes
- Soft, adjustable lighting
- Minimized medical equipment visibility when not in use
- Birth affirmation cards or positive imagery
- Personal items from home (photos, mementos)
Auditory Elements
- Sound systems for personal music
- Noise reduction measures
- White noise options
- Quiet conversations and minimal disruptions
- Nature sounds or guided relaxations
Olfactory Elements
- Essential oil diffusers (following safety guidelines)
- Lavender, chamomile, or peppermint for relaxation
- Minimized clinical smells
- Personal comfort scents from home
Tactile Elements
- Variety of surfaces and textures
- Personal pillows and blankets
- Birth balls and comfort tools
- Warm blankets and compresses
- Water therapy options where available
Mnemonic: “SENSES”
For creating a positive sensory birth environment:
- S – Sound management (music, quiet voices)
- E – Environmental control (temperature, air quality)
- N – Natural elements integration (imagery, sounds)
- S – Scent consideration (aromatherapy, minimized clinical odors)
- E – Eye-friendly lighting (dimmable, natural)
- S – Supportive textures and surfaces
5.3 Support Systems
Human support is a critical component of a positive birth environment and should be facilitated through proper labor room organization:
Birth Companions
- Space and seating for support persons
- Clear policies supporting companion presence
- Amenities for companions (seating, refreshments, rest areas)
- Information resources for companions on supportive behaviors
Healthcare Provider Approach
- Respectful, calm communication
- Informed consent and shared decision-making
- Minimized disruptions and interventions
- Supportive presence rather than constant monitoring
- Positive language and encouragement
WHO Recommendations for Positive Birth Experience
The World Health Organization emphasizes that a positive childbirth experience should:
- Meet a woman’s personal and sociocultural beliefs and expectations
- Result in the birth of a healthy baby in a clinically and psychologically safe environment
- Include practical and emotional support from birth companions and kind, technically competent staff
- Allow women to maintain a sense of personal control through involvement in decision-making
6. Global Best Practices
Different regions around the world have developed innovative approaches to labor room organization that promote both clinical excellence and positive birth experiences:
Netherlands Model
- Integration of home-like environments within hospital settings
- Clear distinction between low and high-risk care spaces
- Labor rooms designed to promote active birth
- Strong midwifery-led care models
- Family-centered approach with accommodation for partners
Scandinavian Approach
- Nature-inspired design elements
- Innovative labor room equipment supporting various positions
- Integration of water birth facilities
- Technology discreetly incorporated into home-like environments
- Focus on continuity of care within the same space
Early Labor Lounges
- Dedicated spaces for women in early labor
- Comfortable, non-clinical environments
- Resources for comfort and distraction
- Reduces unnecessary admissions and interventions
- Promotes active management of early labor
Labor and Delivery Recovery Postpartum (LDRP) Rooms
- Single-room maternity care
- Mother stays in same room throughout entire process
- Reduces transitions and promotes continuity
- Rooms convert from labor to postpartum configuration
- Enhanced privacy and personalization
Evidence-Based Design Elements from Global Research
- Concealed medical equipment that can be accessed when needed
- Movable furniture allowing room reconfiguration
- Integration of nature elements and views
- Balance between privacy and safety through thoughtful design
- Multiple options for labor positions (balls, stools, beds, bars, ropes)
- Easy access to bathrooms with labor-supportive features
7. Mnemonics for Labor Room Organization
Mnemonics can be valuable tools for nursing students to remember key aspects of labor room organization. The following mnemonics summarize critical components:
Mnemonic: “ORGANIZED”
Key elements for labor room setup:
- O – Oxygen and suction equipment ready
- R – Resuscitation equipment for mother and baby
- G – Gloves and personal protective equipment
- A – Appropriate lighting and temperature
- N – Necessary instruments arranged
- I – IV supplies and solutions prepared
- Z – Zero clutter and clean environment
- E – Emergency medications readily available
- D – Documentation materials prepared
Mnemonic: “TRIAGE”
For obstetric triage assessment:
- T – Time of symptom onset
- R – Risk assessment (medical and obstetric)
- I – Initial vital signs
- A – Acuity determination
- G – Gather additional data
- E – Evaluate fetal wellbeing
Mnemonic: “BIRTHING”
For positive birth environment creation:
- B – Breathing room (spacious environment)
- I – Individualized care approach
- R – Reduced noise and disruptions
- T – Temperature control
- H – Homely atmosphere
- I – Intimate lighting options
- N – Nurturing support persons
- G – Gentle, respectful communication
Mnemonic: “LABOR ROOM”
For complete labor room assessment:
- L – Layout appropriate for workflow
- A – Access to emergency equipment
- B – Birth support tools available
- O – Organized supplies and instruments
- R – Ready for complications
- R – Respectful environment
- O – Optimal lighting and temperature
- O – Oxygen and suction verified
- M – Medications checked and accessible
8. Conclusion
Effective labor room organization is a multifaceted endeavor that balances clinical requirements with patient-centered care. The integration of efficient triage protocols, thorough birth preparation, and attention to creating positive birth environments leads to improved maternal outcomes, enhanced patient experiences, and more effective use of healthcare resources.
As nursing professionals, understanding the principles of labor room organization enables you to contribute to safer births, more positive experiences, and better outcomes for mothers and babies. The physical environment, equipment readiness, and workflow processes all play crucial roles in supporting physiological birth and addressing complications when they arise.
By implementing evidence-based approaches to labor room organization, healthcare facilities can create spaces that not only meet clinical needs but also support the psychological and emotional aspects of the birth experience. This holistic approach represents the future of maternity care, where clinical excellence and compassionate, woman-centered care coexist within thoughtfully designed birth environments.
9. References
- American College of Obstetricians and Gynecologists. (2016). Hospital-based triage of obstetric patients. Committee Opinion No. 667. Obstet Gynecol, 128, e16-e19.
- Nilsson, C., Wijk, H., Höglund, L., et al. (2020). Effects of birthing room design on maternal and neonate outcomes: A systematic review. Health Environments Research & Design Journal, 13(3), 198-214.
- Setola, N., Naldi, E., Cocina, G.G., et al. (2019). The impact of the physical environment on intrapartum maternity care: identification of eight crucial building spaces. Health Environments Research & Design Journal, 12(4), 67-98.
- Ruhl, C., Scheich, B., Onokpise, B., & Bingham, D. (2015). Content validity testing of the maternal fetal triage index. Journal of Obstetric, Gynecologic & Neonatal Nursing, 44(6), 701-709.
- Bell, A.M., Bohannon, J., Porthouse, L., et al. (2016). Process improvement to enhance quality in a large volume labor and birth unit. MCN: The American Journal of Maternal/Child Nursing, 41(6), 340-348.
- Paul, J.A., Yount, S.M., Breman, R.B., et al. (2017). Use of an early labor lounge to promote admission in active labor. Journal of Midwifery & Women’s Health, 62(2), 204-209.
- World Health Organization. (2018). WHO recommendations: Intrapartum care for a positive childbirth experience. World Health Organization.
- Goldkuhl, L., Gyllensten, H., Begley, C., et al. (2023). Impact of birthing room design on maternal childbirth experience: results from the Room4Birth randomized trial. Health Environments Research & Design Journal, 16(1), 176-192.
- Angelini, D., & Howard, E. (2014). Obstetric triage: A systematic review of the past fifteen years: 1998-2013. MCN: The American Journal of Maternal/Child Nursing, 39(5), 284-297.
- Cincinnati Birth Center. (2023). 10 ideas to create a calm and relaxing birth environment. Retrieved from https://www.cincinnatibirthcenter.com/blog/10-ideas-to-create-a-calm-and-relaxing-birth-environment
