Active Management of Third Stage of Labour and Examination of Placenta
Comprehensive nursing guide for postpartum hemorrhage prevention
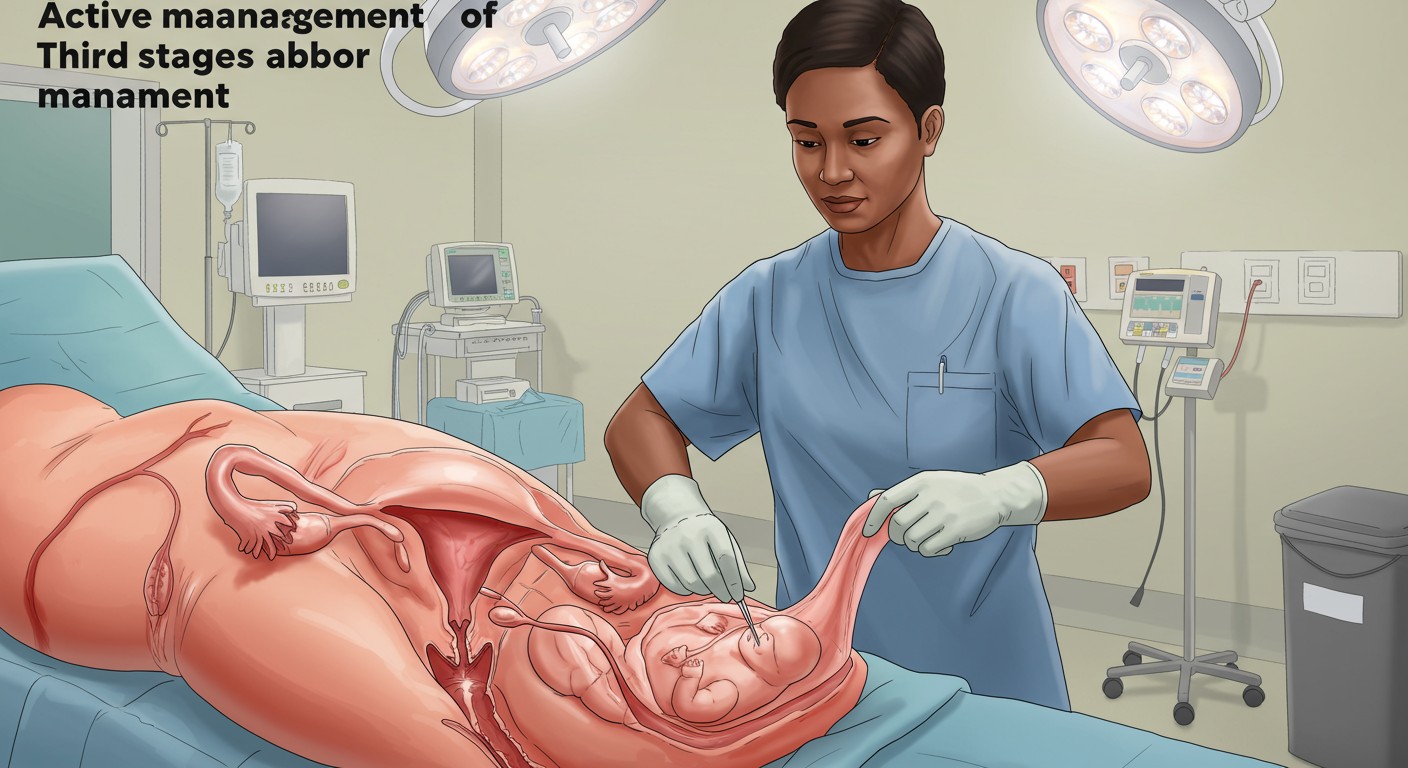
Table of Contents
1. Introduction
The third stage of labour begins after the delivery of the baby and ends with the delivery of the placenta and membranes. This stage typically lasts between 5-15 minutes but can extend up to 30 minutes. Postpartum hemorrhage (PPH) is a significant cause of maternal morbidity and mortality worldwide, with approximately 14 million cases occurring annually. More than 70% of all PPH cases are due to uterine atony (failure of the uterus to contract effectively after delivery).
Active management of the third stage of labour (AMTSL) is an evidence-based intervention that significantly reduces the risk of postpartum hemorrhage by 60-70% compared to expectant management. Understanding the components of AMTSL and proper examination of the placenta and membranes is crucial for all healthcare providers attending births.
2. Active Management of Third Stage of Labour (AMTSL)
AMTSL is a sequence of interventions designed to speed the delivery of the placenta by increasing uterine contractions and preventing PPH by averting uterine atony. It is recommended by the World Health Organization (WHO), the International Federation of Gynecology and Obstetrics (FIGO), and the International Confederation of Midwives (ICM) for all births to prevent postpartum hemorrhage.
Memory Aid: The 3 U’s of AMTSL
- Uterotonic: Administration of a uterotonic drug
- Umbilical cord: Controlled cord traction
- Uterine massage: After delivery of the placenta
3. Components of AMTSL
3.1 Administration of Uterotonic Drugs
Uterotonic drugs should be administered within 1 minute after the birth of the baby, after excluding the presence of another baby. These drugs stimulate uterine contractions, helping to prevent postpartum hemorrhage.
| Uterotonic Drug | Dosage | Route | Considerations |
|---|---|---|---|
| Oxytocin (First-line) | 10 IU | IM/IV | Requires refrigeration; shortest half-life |
| Carbetocin | 100 μg | IM/IV | Heat-stable formulation available; longer-acting than oxytocin |
| Ergometrine/Methylergometrine | 0.2 mg | IM | Contraindicated in hypertension; requires refrigeration |
| Misoprostol | 600 μg | Oral/Sublingual | Heat stable; suitable in low-resource settings; side effects include shivering and pyrexia |
3.2 Controlled Cord Traction (CCT)
Controlled cord traction involves applying gentle traction to the umbilical cord while providing counter-pressure to the uterus. This should only be performed during a contraction and after signs of placental separation are observed.
Signs of Placental Separation:
- Lengthening of the visible portion of the umbilical cord
- A small gush of blood
- The uterus becomes more globular and rises in the abdomen
- The uterus becomes firmer and smaller
Procedure for CCT:
- Clamp the cord close to the perineum
- Hold the clamped cord with one hand
- Place the other hand just above the woman’s pubic bone to stabilize the uterus and provide counter-traction during CCT
- Maintain gentle tension on the cord while waiting for a strong uterine contraction
- During the contraction, encourage the mother to push while gently pulling downward on the cord
- As the placenta descends, move the cord upward to follow the axis of the birth canal
Memory Aid: “DOWN-UP-OUT”
Remember the direction of traction for delivering the placenta:
- DOWN: Pull downwards when the placenta is still in the uterus
- UP: Pull upwards when the placenta is in the vagina
- OUT: Ease the placenta out of the vagina with gentle traction
3.3 Uterine Massage
Immediately after delivery of the placenta, the uterus should be massaged through the abdominal wall to stimulate uterine contractions and expel blood clots. This helps prevent postpartum hemorrhage by ensuring the uterus remains contracted.
Technique:
- Place one hand on the lower abdomen to support the lower uterine segment
- Place the other hand on the fundus (top) of the uterus
- Massage the fundus in a circular motion until the uterus is firm
- Check the uterus every 15 minutes for 2 hours after delivery
- Massage the uterus if it becomes soft
4. Examination of Placenta, Membranes, and Vessels
Thorough examination of the placenta, membranes, and vessels is essential to ensure complete delivery and detect potential abnormalities. Retained placental fragments increase the risk of postpartum hemorrhage, infection, and subinvolution of the uterus.
4.1 Placental Examination
Maternal Surface (Decidual Side):
- Dark red, rough appearance with 15-20 cotyledons
- Inspect for completeness and integrity
- Check for missing cotyledons or irregular areas suggesting retained fragments
- Examine for abnormal calcifications, infarcts, or hematomas
Fetal Surface (Chorionic/Amnion Side):
- Shiny, gray-white surface with visible blood vessels
- Examine the umbilical cord insertion site
- Check for abnormal cord insertion (velamentous, marginal, etc.)
- Look for any color changes, meconium staining, or abnormal lesions
4.2 Membrane Examination
Hold the placenta up by the cord, allowing membranes to hang down. The membranes should be:
- Intact or torn in a single site (where the baby emerged)
- Complete with no missing pieces
- Shiny and translucent
Reconstruct the membranes to ensure they form a complete sac. Incomplete membranes suggest retained placental tissue, which increases the risk of postpartum hemorrhage and infection.
4.3 Umbilical Cord Examination
- Normal length is approximately 40-60 cm
- Diameter is typically 1-2 cm
- Normally contains 3 vessels: 2 arteries and 1 vein
- The vein carries oxygenated blood to the fetus (larger lumen)
- The arteries carry deoxygenated blood from the fetus (smaller lumens)
- Note and document any abnormalities in the number of vessels
Memory Aid: “VAN” for Umbilical Vessels
Vein = Very large lumen
Arteries = Always two (normally)
Not normal = Single umbilical artery (associated with congenital anomalies)
5. Placental Abnormalities and Clinical Significance
| Abnormality | Description | Clinical Significance |
|---|---|---|
| Placenta Accreta Spectrum | Abnormal adherence of placental tissue to the uterine wall | High risk for severe postpartum hemorrhage; may require hysterectomy |
| Placenta Previa | Placenta implanted in lower uterine segment, covering cervical os | Risk for antepartum and postpartum hemorrhage |
| Succenturiate Lobe | Extra lobe connected to main placenta by blood vessels | Risk of retained placental tissue and postpartum hemorrhage |
| Battledore Placenta | Marginal insertion of umbilical cord | Associated with fetal growth restriction and preterm birth |
| Velamentous Cord Insertion | Cord inserts into membranes rather than placenta | Risk of vasa previa and fetal hemorrhage |
| Single Umbilical Artery | Only one artery instead of two in umbilical cord | Associated with congenital anomalies |
| Circumvallate Placenta | Membranes fold back onto fetal surface, creating a white ring | Associated with antepartum bleeding and preterm labor |
6. Best Practices and Recent Updates
Best Practice 1: Heat-Stable Carbetocin
The WHO now recommends heat-stable carbetocin (HSC) as an effective alternative to oxytocin for postpartum hemorrhage prevention, especially in settings where refrigeration is limited. HSC remains stable for up to 30 months at 30°C and 75% relative humidity, making it ideal for low-resource settings.
Best Practice 2: Delayed Cord Clamping with AMTSL
Recent guidelines recommend integrating delayed cord clamping (DCC) with AMTSL. The umbilical cord should be clamped 1-3 minutes after birth while initiating essential newborn care. Studies show DCC does not increase the risk of postpartum hemorrhage and provides significant benefits to the newborn, including improved iron status and developmental outcomes.
Best Practice 3: Uterine Massage No Longer Recommended as Prevention
Recent WHO guidelines (2018) no longer recommend sustained uterine massage as a preventive intervention for postpartum hemorrhage in women who have received prophylactic oxytocin. However, regular assessment of uterine tone remains essential for early identification of uterine atony. Uterine massage is still indicated if the uterus is soft or for treatment of established PPH.
7. Nursing Implications
7.1 Nursing Responsibilities
- Prepare and administer uterotonic drugs according to protocol
- Monitor vital signs and blood loss during the third stage
- Assist with controlled cord traction when indicated
- Perform thorough examination of the placenta and membranes
- Document findings and report abnormalities immediately
- Monitor for signs of postpartum hemorrhage (excessive bleeding, uterine atony)
- Provide patient education on postpartum warning signs
7.2 Risk Assessment and Prevention
Identify women at increased risk for postpartum hemorrhage:
- Previous PPH
- Multiple gestation
- Polyhydramnios
- Macrosomia
- Prolonged labor
- Grand multiparity (≥5 previous pregnancies)
- Placenta previa or accreta
- Pre-eclampsia
- Use of oxytocin for labor induction/augmentation
7.3 Documentation Requirements
Comprehensive documentation should include:
- Time of placental delivery
- Method used (spontaneous or CCT)
- Uterotonic drug administered (type, dose, route, time)
- Placental examination findings
- Completeness of placenta and membranes
- Number of vessels in umbilical cord
- Cord insertion type
- Any abnormal findings
- Estimated blood loss
- Uterine tone assessment
- Any complications and interventions
Key Points
AMTSL Components
- Uterotonic administration
- Controlled cord traction
- Uterine tone assessment
Placental Examination
- Maternal surface: 15-20 cotyledons
- Fetal surface: vessels, cord insertion
- Membranes: completeness check
- Umbilical cord: 3 vessels (2A, 1V)
Risk Factors for PPH
- Previous PPH history
- Multiple gestation
- Prolonged labor
- Placental abnormalities
- Grand multiparity
Quick Reference
Normal blood loss during vaginal delivery: <500 mL
Normal blood loss during cesarean delivery: <1000 mL
Primary PPH: excessive bleeding within 24 hours of birth
Secondary PPH: excessive bleeding 24 hours to 12 weeks after birth
