Perineal Tear Assessment and Postpartum IUCD Insertion
Comprehensive Guide for Nursing Students
Introduction
Perineal trauma is a common occurrence during vaginal delivery, affecting up to 85% of women giving birth. Assessment and management of perineal tear assessment is a critical nursing skill, while postpartum IUCD insertion represents an important contraceptive option during the immediate postpartum period. This guide provides comprehensive information for nursing students on both topics.
Perineal Tear Assessment
Thorough perineal tear assessment is essential for proper classification, management, and prevention of complications. The nurse’s role includes not only assisting with assessment but also providing support, education, and follow-up care.
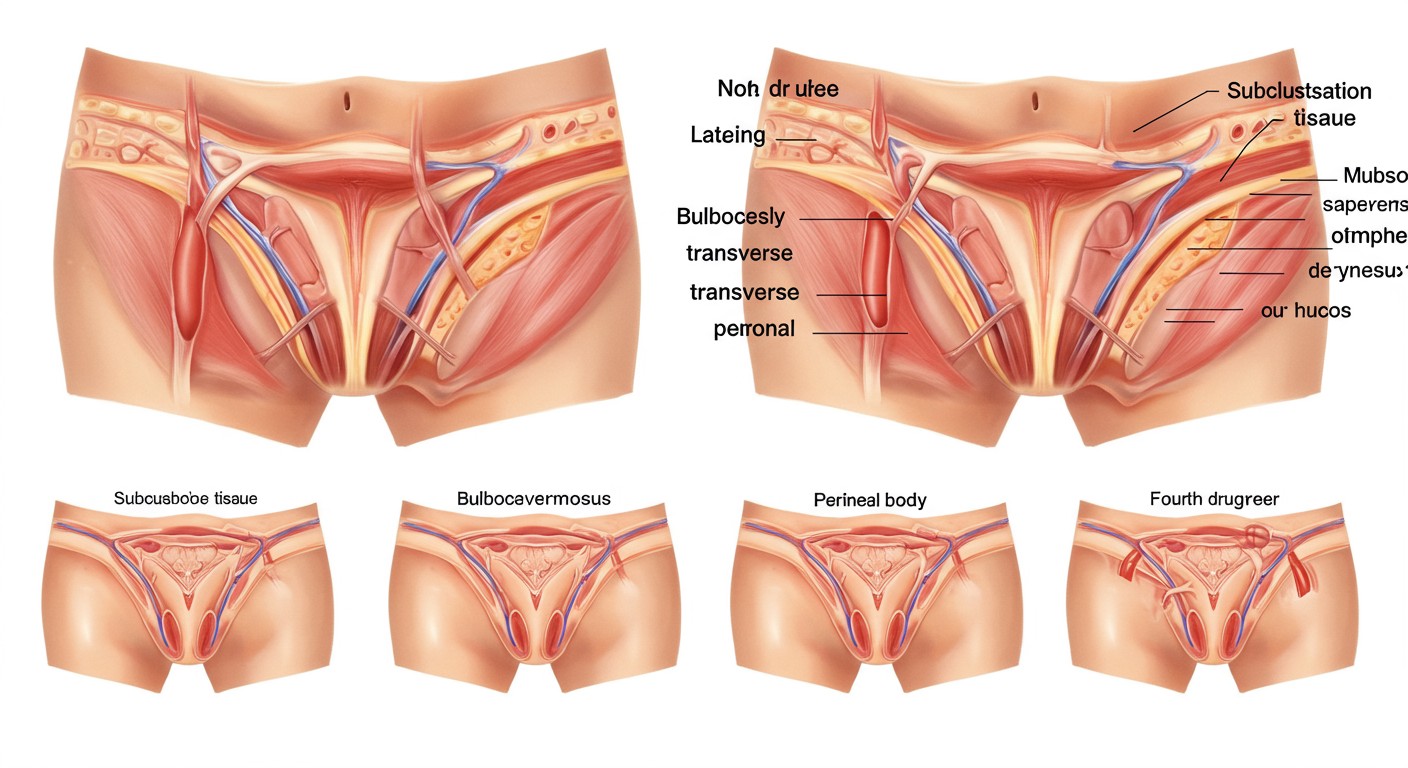
Classification of Perineal Tears
| Degree | Description | Structures Involved | Management |
|---|---|---|---|
| First-Degree | Superficial tear | Skin of perineum and vaginal mucosa only | May not require suturing if hemostasis is achieved |
| Second-Degree | Deeper tear | Skin, vaginal mucosa, and perineal muscles | Requires suturing in layers |
| Third-Degree | Extends to anal sphincter | All above structures plus anal sphincter complex (partial or complete) | Requires careful repair by experienced clinician |
| Fourth-Degree | Complete tear | All above structures plus rectal mucosa | Requires specialized repair in operating room |
Memory Aid: MAST
Mucosa – 1st degree
And muscles – 2nd degree
Sphincter – 3rd degree
Through to rectum – 4th degree
Assessment Techniques
Proper perineal tear assessment requires good lighting, positioning, equipment, and a systematic approach:
Preparation
- Ensure adequate lighting (directed light source)
- Position patient in lithotomy position
- Maintain privacy and dignity
- Use sterile gloves and equipment
- Explain procedure and obtain consent
Systematic Assessment (LAVANT)
- Look at the perineum for visible tears, bruising, and swelling
- Assess for bleeding and hematoma formation
- Visualize the full extent of tear using gentle traction
- Anal sphincter integrity assessment (ask patient to squeeze)
- Note any extensions into surrounding structures
- Test for rectal involvement (with gloved finger in rectum)
Suturing Techniques
After proper perineal tear assessment, appropriate suturing technique must be employed:
| Tear Type | Suture Material | Technique |
|---|---|---|
| First-Degree | Absorbable (2-0 Vicryl) | Continuous subcuticular |
| Second-Degree | Absorbable (2-0 Vicryl) | Three-layer closure (vaginal mucosa, muscle layer, perineal skin) |
| Third-Degree | Fine absorbable (3-0 PDS) | End-to-end repair of sphincter with interrupted sutures |
| Fourth-Degree | Fine absorbable (4-0 Vicryl) | Layered closure starting with rectal mucosa (interrupted) |
Important Nursing Considerations
- Ensure adequate analgesia before suturing (lidocaine 1%)
- Count all needles and swabs before and after procedure
- Document extent of tear, suturing technique, and materials used
- Monitor for bleeding during and after repair
- Third and fourth-degree tears require antibiotics prophylaxis
Postpartum Care for Perineal Tears
Following perineal tear assessment and repair, proper postpartum care is essential:
Immediate Care (24-48 hours)
- Regular ice packs (20 min on, 20 min off)
- Adequate pain management (NSAIDs, acetaminophen)
- Perineal hygiene education
- Pelvic floor exercises instruction
- Regular assessment for signs of infection
Long-Term Care
- Sitz baths 2-3 times daily
- Avoid constipation (stool softeners, adequate hydration)
- Continue pelvic floor exercises
- Follow-up assessment at 6-week postpartum visit
- Referral to pelvic floor physiotherapist if needed
Postpartum IUCD Insertion
Postpartum intrauterine contraceptive device (IUCD) insertion offers immediate, effective, and reversible contraception following childbirth. Nurses play a vital role in counseling, assisting with insertion, and providing follow-up care.
Timing of Postpartum IUCD Insertion
| Timing | Description | Considerations |
|---|---|---|
| Immediate Postplacental | Within 10 minutes of placental delivery | Highest convenience, lowest return rate, slightly higher expulsion rate |
| Early Postpartum | Within 48 hours of delivery | Moderate expulsion rate, requires trained provider |
| Interval | ≥ 4 weeks postpartum | Lowest expulsion rate, requires additional visit |
| Trans-cesarean | During cesarean section | Lowest expulsion rate, placed before uterine closure |
Memory Aid: POET for IUCD Insertion Timing
Postplacental – Within 10 minutes
Operating room – During cesarean
Early postpartum – Within 48 hours
Tardily (Interval) – After 4 weeks
Postpartum IUCD Insertion Technique
Proper technique during insertion is critical to reduce the risk of expulsion and other complications:
Preparation
- Confirm patient consent and eligibility
- Use Cu T 380A or levonorgestrel IUD (both WHO MEC Category 1)
- Ensure sterile technique and equipment
- Empty patient’s bladder
- Check vital signs and uterine tone
Insertion Steps (Ring Forceps Technique)
- Load IUCD onto ring forceps (held horizontally at strategic point)
- Perform bimanual examination to assess uterine position
- Visualize cervix with speculum
- Cleanse cervix with antiseptic solution
- Grasp anterior lip of cervix with ring forceps
- Insert loaded forceps through cervix to uterine fundus
- Open forceps to release IUCD at fundus
- Move forceps to side wall before closing and removing
- Leave strings uncut or trim minimally
- Document insertion details in patient record
Contraindications for Postpartum IUCD
Absolute Contraindications
- Puerperal sepsis
- Chorioamnionitis
- Unresolved postpartum hemorrhage
- Rupture of membranes > 18 hours
- Extensive genital trauma
Relative Contraindications
- Uterine anomalies
- Previous postpartum endometritis
- HIV with advanced disease (WHO MEC Category 2/3)
- Severe anemia
- High risk for STIs
Follow-up Care After IUCD Insertion
Proper follow-up is essential for early detection of complications and ensuring continued satisfaction:
Follow-up Schedule
- Before discharge: Review warning signs, care instructions
- First visit: 4-6 weeks postpartum to check for expulsion
- Second visit: 3 months after insertion
- Routine care: Annual check-ups thereafter
Patient Education Points (PAINS)
Instruct patients to seek care immediately if they experience:
- Period late, pregnancy concerns
- Abdominal pain, severe cramping
- Infection symptoms or fever
- Not feeling well, unusual discharge
- String problems (missing, shorter, longer)
Best Practices & Recent Updates
1. Enhanced Recovery Protocols
Recent guidelines recommend multimodal analgesia for perineal tear assessment and repair, including infiltration with long-acting local anesthetics like 0.5% bupivacaine with adrenaline. Studies show this reduces opioid requirements and improves maternal satisfaction postpartum.
2. IUCD Type Recommendations
2023 WHO updates recommend the levonorgestrel-releasing IUD for immediate postpartum insertion in breastfeeding women (changed from Category 2 to Category 1), as evidence shows no negative impact on breastfeeding outcomes or infant development.
3. Trauma Prevention Strategies
Updated ACOG guidelines (2022) recommend warm compress application to the perineum during the second stage of labor, combined with perineal massage and controlled delivery of the fetal head to reduce severe perineal trauma by up to 40%.
Nursing Clinical Pearl
When performing perineal tear assessment, always conduct a rectal examination to rule out buttonhole defects that might be missed on vaginal examination alone. These occult injuries can lead to rectovaginal fistulas if undetected and unrepaired.
References
- World Health Organization. (2023). Medical eligibility criteria for contraceptive use (6th ed.). WHO.
- American College of Obstetricians and Gynecologists. (2022). Practice Bulletin No. 198: Prevention and Management of Obstetric Lacerations at Vaginal Delivery.
- Royal College of Obstetricians and Gynaecologists. (2023). Green-top Guideline No. 29: The Management of Third- and Fourth-degree Perineal Tears.
- International Federation of Gynecology and Obstetrics. (2023). Post-pregnancy contraception: Clinical recommendations.
- Lopez LM, et al. (2022). Immediate postpartum insertion of intrauterine devices. Cochrane Database of Systematic Reviews, 2022(5).
