Infection Prevention for Newborns
Asepsis, Hand Washing, and Immunization
Comprehensive Nursing Notes
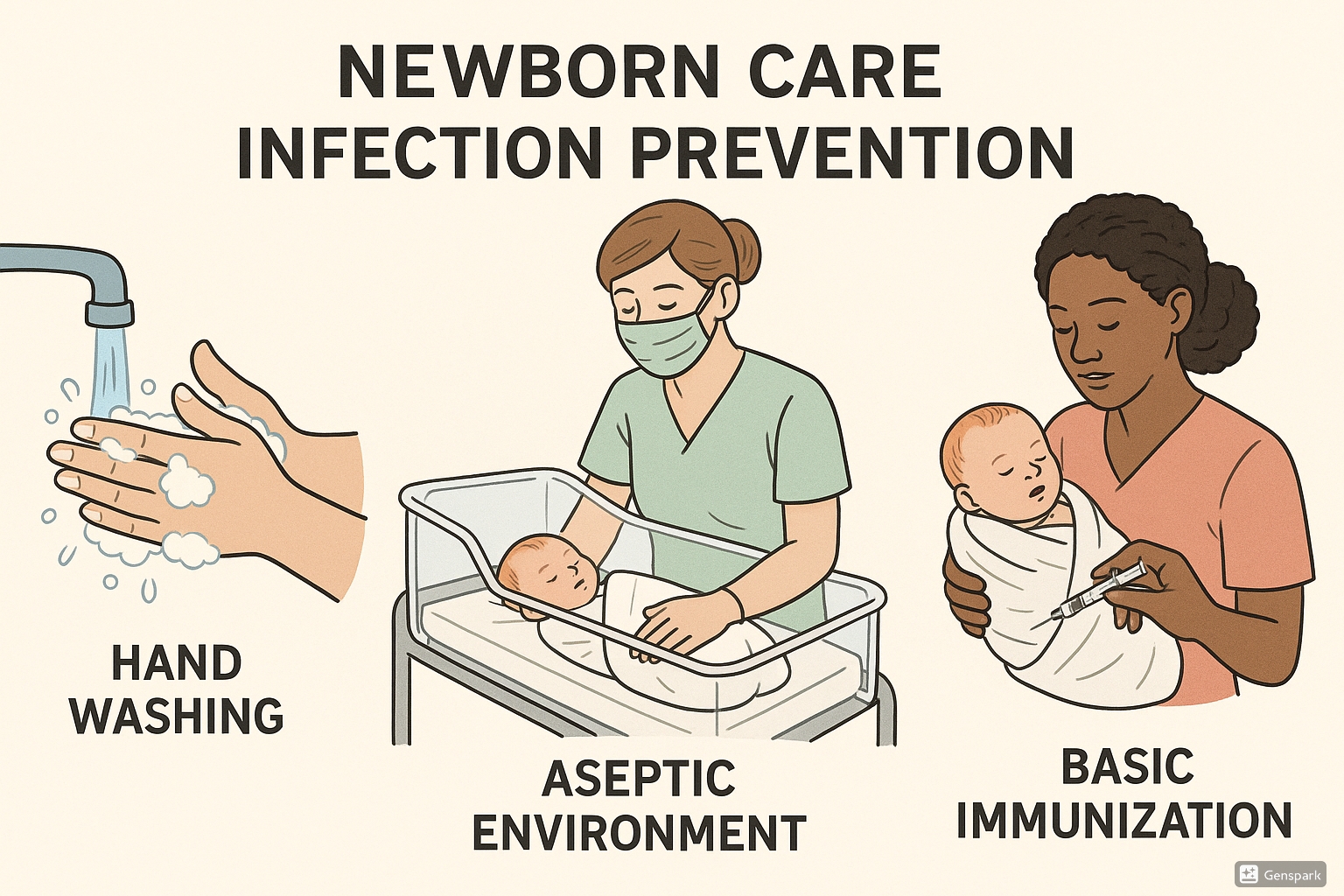
Figure 1: Key elements of newborn infection prevention including hand hygiene, aseptic technique, and immunization
Introduction
Newborn infection prevention is a critical aspect of neonatal care that directly impacts infant morbidity and mortality rates. Newborns are particularly vulnerable to infections due to their immature immune systems and limited protective flora. This comprehensive guide provides essential knowledge about preventing infections in newborns through proper aseptic techniques, hand washing protocols, and timely immunizations.
Did you know?
Neonatal infections account for approximately 1.6 million deaths globally each year. Effective newborn infection prevention measures can reduce these numbers by up to 70%.
Table of Contents
1. Understanding Infection Risk in Newborns
Why Newborns Are Vulnerable
Newborn infection prevention begins with understanding why neonates are particularly susceptible to infections. Their vulnerability stems from several physiological factors:
| Factor | Description | Infection Prevention Implication |
|---|---|---|
| Immature Immune System | Reduced quantities of immunoglobulins; limited inflammatory response | Requires strict aseptic techniques and minimal exposure to pathogens |
| Thin, Permeable Skin | Immature skin barrier function; increased permeability | Necessitates gentle cleansing and careful handling |
| Absent Protective Flora | Limited colonization of beneficial bacteria | Increases susceptibility to colonization by pathogenic organisms |
| Limited Maternal Antibodies | Only IgG crosses placenta; all other antibodies must be acquired | Highlights importance of maternal immunization and breast milk |
Common Infection Sources in Neonates
Maternal Sources
- Maternal genital tract infections
- Chorioamnionitis
- Maternal bloodstream infections
- Vertical transmission during delivery
Environmental Sources
- Healthcare worker hands
- Medical equipment and devices
- Hospital surfaces and linens
- Cross-contamination between patients
2. Asepsis Techniques for Newborn Care
Asepsis refers to practices that prevent contamination by eliminating infectious agents. In newborn infection prevention, both medical and surgical aseptic techniques are essential.
Medical vs. Surgical Asepsis
Medical Asepsis (Clean Technique)
Practices that reduce the number and transmission of pathogens:
- Regular hand hygiene
- Environmental cleaning
- Clean gloves for routine care
- Proper waste disposal
- Routine disinfection of surfaces
Used for routine newborn care activities like feeding, diaper changes, and bathing.
Surgical Asepsis (Sterile Technique)
Practices that eliminate all microorganisms:
- Sterile gloves and equipment
- Sterile field maintenance
- Sterile barrier precautions
- Surgical hand scrub
- Meticulous clean-to-dirty workflow
Used for invasive procedures like umbilical catheter insertion, lumbar punctures, and central line placement.
Key Aseptic Practices in Newborn Units
1. Environmental Asepsis
Regular cleaning and disinfection of incubators, cribs, and surrounding environment with hospital-approved disinfectants. All surfaces should be cleaned at least once per shift, with terminal cleaning between patients.
2. Equipment Asepsis
Dedicated equipment for each newborn whenever possible. Shared equipment must be properly cleaned and disinfected between patient use. High-touch surfaces require more frequent disinfection.
3. Skin Care Asepsis
Gentle cleansing with warm sterile water for premature newborns. Full-term newborns can receive bathing with mild soap after stabilization of temperature. Antiseptic solutions should be carefully selected based on gestational age.
4. Umbilical Cord Care
Clean technique with chlorhexidine 4% in high-risk settings or dry cord care in low-risk settings. Avoid alcohol which delays cord separation. Keep the cord clean and dry, exposing it to air when possible.
5. Feeding Asepsis
Proper hand hygiene before handling breast milk or formula. Sterilization of all feeding equipment. Breast milk storage following evidence-based guidelines. Formula preparation in a clean dedicated area.
Critical Alert:
A breach in aseptic technique during invasive procedures can lead to devastating infections in newborns. If sterility is compromised, discard all contaminated items and restart with new sterile supplies.
3. Hand Washing Protocols for Newborn Care
Hand hygiene is the single most important intervention in newborn infection prevention. Proper hand washing removes transient flora and reduces resident flora on the hands, preventing pathogen transmission to vulnerable newborns.
The WHO 5 Moments for Hand Hygiene in Neonatal Care
- Before touching a newborn – Perform hand hygiene before any direct contact with the infant
- Before clean/aseptic procedures – Perform hand hygiene immediately before any procedure requiring aseptic technique (IV insertion, medication preparation)
- After body fluid exposure risk – Perform hand hygiene immediately after exposure to any body fluids (diaper changes, suctioning)
- After touching a newborn – Perform hand hygiene after touching the infant, even when the contact involved no body fluids
- After touching newborn surroundings – Perform hand hygiene after touching any objects or furniture in the immediate vicinity of the newborn
Hand Washing Techniques
Routine Hand Washing (40-60 seconds)
Steps:
- Wet hands with clean, running water
- Apply enough soap to cover all hand surfaces
- Rub hands palm to palm
- Right palm over left dorsum with interlaced fingers and vice versa
- Palm to palm with fingers interlaced
- Backs of fingers to opposing palms with fingers interlocked
- Rotational rubbing of left thumb clasped in right palm and vice versa
- Rotational rubbing, backward and forward with clasped fingers of right hand in left palm and vice versa
- Rinse hands with water
- Dry thoroughly with a single-use towel
- Use towel to turn off faucet
When to Use:
- Upon entering the neonatal unit
- Before and after routine newborn care
- After using the restroom
- After contact with bodily fluids
- When hands are visibly soiled
- Before preparing feeding
- After diaper changes
- Before going home
Alcohol-Based Hand Rub (20-30 seconds)
Steps:
- Apply a palm-full of alcohol-based hand rub
- Cover all surfaces of the hands
- Rub hands until dry
- Follow the same hand movements as with soap and water
When to Use:
- Between patient contacts
- Before handling medications
- After touching surfaces in the patient zone
- Before donning and after removing gloves
- When hands are not visibly soiled
Surgical Hand Scrub (2-5 minutes)
When to Use:
Before any sterile invasive procedures on newborns:
- Central line insertion
- Umbilical catheter placement
- Lumbar puncture
- Chest tube insertion
Family Hand Hygiene Education
Teaching parents and family members proper hand hygiene is a crucial component of newborn infection prevention. Provide demonstrations and visual aids to ensure compliance. Encourage hand hygiene before every infant interaction.
4. Newborn Immunization
Immunization is a cornerstone of newborn infection prevention, providing protection against serious infectious diseases. The first vaccines are administered shortly after birth, initiating the infant’s immunization schedule.
Birth Dose Vaccines
| Vaccine | Timing | Route | Dose | Special Considerations |
|---|---|---|---|---|
| Hepatitis B (HepB) | Within 24 hours of birth | Intramuscular | 0.5 mL | Should be given regardless of birth weight. For infants of HBsAg-positive mothers, administer HepB vaccine and HBIG within 12 hours of birth. |
| Bacille Calmette-Guérin (BCG) | At birth or soon after | Intradermal | 0.05 mL | Given in countries with high TB prevalence. Not routinely given in the US. May be delayed in preterm or low birth weight infants. |
| Oral Polio Vaccine (OPV) | At birth (in some countries) | Oral | 2 drops | Birth dose is given in polio-endemic countries or high-risk areas. Not given at birth in the US and many developed countries. |
Recommended Immunization Schedule: First 6 Months
| Age | Recommended Vaccines |
|---|---|
| Birth | HepB (1st dose) |
| 1-2 Months | HepB (2nd dose) |
| 2 Months | DTaP (1st dose), IPV (1st dose), Hib (1st dose), PCV13 (1st dose), RV (1st dose) |
| 4 Months | DTaP (2nd dose), IPV (2nd dose), Hib (2nd dose), PCV13 (2nd dose), RV (2nd dose) |
| 6 Months | DTaP (3rd dose), Hib (3rd dose), PCV13 (3rd dose), RV (3rd dose if needed), Annual influenza vaccine (during flu season) |
Vaccine Abbreviations:
- HepB: Hepatitis B
- DTaP: Diphtheria, Tetanus, acellular Pertussis
- Hib: Haemophilus influenzae type b
- IPV: Inactivated Polio Vaccine
- PCV13: Pneumococcal Conjugate Vaccine
- RV: Rotavirus
- BCG: Bacille Calmette-Guérin
- OPV: Oral Polio Vaccine
Immunization Administration Techniques
General Principles for Safe Administration
Before Administration:
- Verify correct patient (using two identifiers)
- Check vaccine expiration date and lot number
- Inspect vaccine for particulate matter or discoloration
- Verify correct vaccine, dose, route, and timing
- Review contraindications and precautions
- Practice proper hand hygiene
- Prepare clean administration site
During Administration:
- Position and comfort infant appropriately
- Select appropriate needle size based on route
- Use proper technique for route of administration
- For IM injections in infants: use anterolateral thigh
- Insert needle quickly at correct angle
- Inject vaccine slowly
- Apply gentle pressure with gauze after withdrawal
Pain Management During Immunization
To reduce pain and distress during newborn infection prevention immunizations:
- Administer sweet-tasting solution (sucrose) 1-2 minutes before injection
- Encourage breastfeeding during or immediately after vaccination
- Hold infant securely in parent’s arms or skin-to-skin
- Administer most painful vaccine last when multiple vaccines are given
- Use distraction techniques appropriate for newborns
5. Helpful Mnemonics for Infection Prevention
Mnemonics can help healthcare providers remember key aspects of newborn infection prevention. Here are several useful memory aids:
C.L.E.A.N.
For remembering essential components of newborn infection prevention:
- C – Consistent hand hygiene before and after every patient contact
- L – Limit visitors and screen for illness
- E – Environment must be cleaned regularly
- A – Aseptic technique for all procedures
- N – Needles and sharps must be handled safely
W.A.S.H.
For proper hand washing technique:
- W – Wet hands thoroughly under running water
- A – Apply enough soap to cover all surfaces
- S – Scrub all surfaces for at least 20 seconds
- H – Rinse and dry thoroughly with clean towel
I.M.M.U.N.I.Z.E.
Key principles for safe newborn immunization:
- I – Identify patient correctly using two identifiers
- M – Medication verification (right vaccine, dose, route)
- M – Monitor for adverse reactions
- U – Use proper administration technique
- N – Note contraindications before administering
- I – Inform parents about benefits and side effects
- Z – Zero tolerance for unsafe practices
- E – Educate parents about vaccination schedule
S.P.O.T. Infection
For early recognition of infection signs in newborns:
- S – Skin changes (color, rash, temperature)
- P – Poor feeding or activity
- O – Oxygen requirement changes or respiratory distress
- T – Temperature instability (hypothermia or fever)
6. Global Best Practices in Newborn Infection Prevention
Different regions have developed innovative approaches to newborn infection prevention that have proven successful. These practices can inspire improvements in neonatal care worldwide:
Kangaroo Mother Care (KMC)
Origin: Colombia
Prolonged skin-to-skin contact between mother and infant reduces infection rates while promoting bonding and breastfeeding. KMC has been shown to reduce neonatal mortality by 40% in preterm infants and significantly lower infection rates.
Implementation: Educate mothers on proper skin-to-skin positioning, maintaining for at least 1-3 hours per session, multiple times daily.
Chlorhexidine Cord Care
Origin: Nepal, Bangladesh, Pakistan
Application of 4% chlorhexidine to the umbilical cord stump has reduced neonatal mortality by 23% and omphalitis by 27-56% in community settings with high infection rates.
Implementation: Single application within 24 hours of birth, or daily application for 7 days in high-risk settings.
Clean Birth Kits
Origin: Tanzania, India
Distribution of clean birth kits to mothers and traditional birth attendants for home deliveries has reduced neonatal infection rates by providing basic sterile supplies.
Implementation: Kits typically include soap, clean blade for cord cutting, clean cord ties, plastic sheet, and gloves.
Early Essential Newborn Care (EENC)
Origin: Western Pacific Region (WHO)
A package of simple interventions including delayed cord clamping, immediate skin-to-skin contact, exclusive breastfeeding, and non-separation of mother and newborn.
Implementation: Has reduced infections and hypothermia in over 10 countries across the Western Pacific Region.
Infection Prevention Checklists
Origin: Japan, Sweden
Standardized checklists for all aspects of newborn infection prevention have reduced central line-associated bloodstream infections in NICUs by up to 70% in some facilities.
Implementation: Daily checks of all line sites, regular bundle compliance monitoring, and timeout procedures before invasive procedures.
7. Conclusion and Key Takeaways
Newborn infection prevention represents one of the most critical aspects of neonatal care. The proper implementation of aseptic techniques, meticulous hand washing protocols, and timely immunizations can dramatically reduce morbidity and mortality among newborns.
Key Takeaways
- Newborns have unique vulnerability to infections due to their immature immune systems
- Hand hygiene is the single most effective newborn infection prevention measure
- Both medical and surgical aseptic techniques are essential in neonatal care
- Immunization schedules should begin shortly after birth and continue according to established guidelines
- Family education is crucial for maintaining infection prevention practices beyond the healthcare setting
- Global best practices can provide valuable insights for improving local newborn infection prevention protocols
As healthcare providers, our vigilance in adhering to infection prevention protocols protects the most vulnerable patients in our care. By consistently implementing evidence-based practices for newborn infection prevention, we can significantly improve outcomes for newborns worldwide.
References
- World Health Organization. (2022). WHO recommendations on newborn health: guidelines approved by the WHO Guidelines Review Committee. Geneva: WHO.
- Centers for Disease Control and Prevention. (2023). Recommended Child and Adolescent Immunization Schedule for ages 18 years or younger. Atlanta: CDC.
- World Health Organization. (2021). WHO Guidelines on Hand Hygiene in Health Care. Geneva: WHO.
- Polin, R.A., & Denson, S. (2020). Strategies for prevention of healthcare-associated infections in the NICU. Pediatrics, 145(2), e20193256.
- American Academy of Pediatrics. (2022). Red Book: Report of the Committee on Infectious Diseases, 32nd Edition.
- Mullany, L.C., et al. (2021). Topical applications of chlorhexidine to the umbilical cord for prevention of omphalitis and neonatal mortality in southern Nepal: a community-based, cluster-randomised trial. The Lancet, 367(9514), 910-918.
- UNICEF & WHO. (2023). Protecting, promoting and supporting breastfeeding: The Baby-friendly Hospital Initiative for small, sick and preterm newborns.
- Association of Women’s Health, Obstetric and Neonatal Nurses. (2022). Neonatal Skin Care Evidence-Based Clinical Practice Guideline.
