Abnormalities of Placenta and Cord
Comprehensive Nursing Notes
Table of Contents
Introduction
Placental abnormalities represent critical conditions in obstetric nursing that can significantly impact maternal and fetal outcomes. Understanding these complications is essential for nursing professionals to provide optimal care during pregnancy, labor, and delivery. This comprehensive guide covers the most common placental abnormalities encountered in clinical practice.
Clinical Significance
Placental abnormalities occur in approximately 1-5% of all pregnancies and are responsible for significant maternal and perinatal morbidity and mortality worldwide. Early recognition and appropriate nursing interventions are crucial for optimal outcomes.
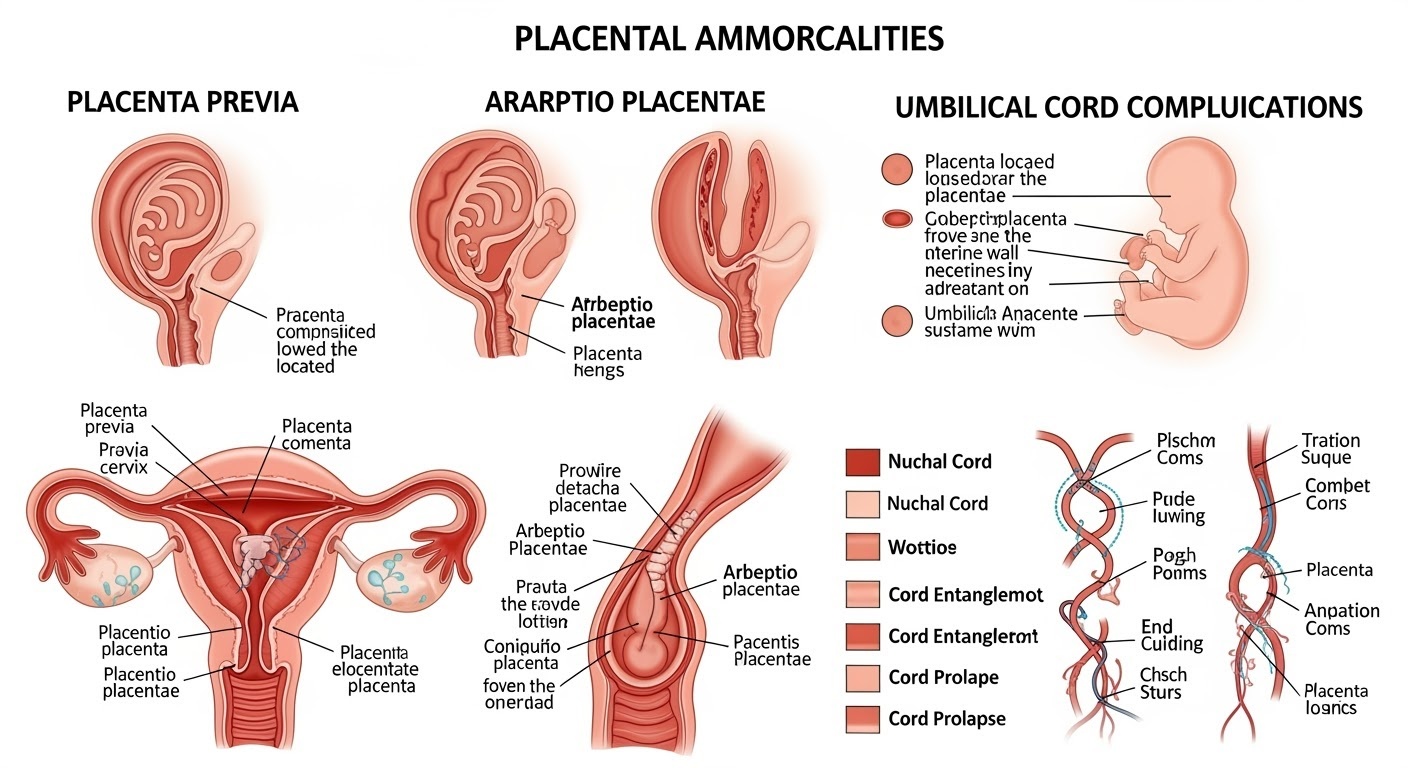
Figure 1: Overview of common placental abnormalities and umbilical cord complications
Placental Abnormalities
Placenta Previa
Definition & Types
Placenta previa occurs when the placenta implants in the lower uterine segment, partially or completely covering the internal cervical os.
Classification:
- Complete (Total): Placenta completely covers the internal os
- Partial: Placenta partially covers the internal os
- Marginal: Placental edge reaches the internal os
- Low-lying: Placenta within 2cm of internal os
Risk Factors
- Previous cesarean deliveries
- Advanced maternal age (>35 years)
- Multiparity
- Previous placenta previa
- Smoking during pregnancy
- Multiple gestations
- Previous uterine surgery or curettage
Abruptio Placentae (Placental Abruption)
Definition & Severity
Premature separation of a normally implanted placenta from the uterine wall before delivery of the fetus.
Classification by Severity:
- Grade 1 (Mild): <20% separation, minimal bleeding
- Grade 2 (Moderate): 20-50% separation, moderate bleeding
- Grade 3 (Severe): >50% separation, severe bleeding, fetal compromise
Types of Abruption
- Revealed (External): Blood escapes through cervix and vagina
- Concealed (Internal): Blood trapped behind placenta
- Mixed: Combination of both types
Placenta Accreta Spectrum
A range of placental adhesion disorders where the placenta attaches too deeply into the uterine wall.
| Type | Definition | Prevalence | Severity |
|---|---|---|---|
| Placenta Accreta | Placenta adheres to myometrium | 75-78% | Least severe |
| Placenta Increta | Placenta invades myometrium | 17% | Moderate |
| Placenta Percreta | Placenta penetrates through uterine wall | 5-7% | Most severe |
Umbilical Cord Abnormalities
Cord Prolapse
Descent of umbilical cord through the cervix alongside or ahead of the presenting part.
Emergency Situation: Requires immediate intervention to prevent fetal hypoxia and death.
Risk Factors:
- Premature rupture of membranes
- Malpresentation (breech, transverse)
- Polyhydramnios
- Multiple gestations
- Low birth weight
Nuchal Cord
Umbilical cord wrapped around the fetal neck one or more times.
Incidence: Occurs in 20-25% of all deliveries. Most cases are benign.
Management Considerations:
- Monitor fetal heart rate patterns
- Assess for variable decelerations
- Consider cesarean if severe compromise
- Prepare for cord reduction at delivery
Cord Knots
True knots in the umbilical cord formed by fetal movement through a loop of cord.
Types:
- True knots: Actual knots in cord (1% incidence)
- False knots: Vessel variations, not clinically significant
Vasa Previa
Fetal blood vessels cross the internal cervical os below the presenting part.
High Risk: Fetal mortality rate 60% if undiagnosed, <3% if diagnosed prenatally.
Associated Conditions:
- Velamentous cord insertion
- Placenta previa
- Multiple gestations
- IVF pregnancies
Pathophysiology
Placenta Previa Pathophysiology
Mechanism:
- Abnormal implantation in lower uterine segment
- Cervical effacement and dilation cause bleeding
- Lower segment lacks contractile ability
- Bleeding from exposed maternal vessels
Consequences:
- Painless vaginal bleeding
- Maternal hemorrhage risk
- Fetal hypoxia from blood loss
- Preterm delivery risk
Abruptio Placentae Pathophysiology
Mechanism:
- Vasospasm of spiral arteries
- Decidual necrosis and hemorrhage
- Hematoma formation behind placenta
- Further placental separation
Consequences:
- Painful vaginal bleeding
- Uterine tetany and pain
- Fetal distress and hypoxia
- Coagulopathy risk (DIC)
Clinical Manifestations
| Condition | Bleeding Pattern | Pain | Uterine Tone | Fetal Status |
|---|---|---|---|---|
| Placenta Previa | Painless, bright red, intermittent | Absent | Soft, non-tender | Usually normal unless severe bleeding |
| Abruptio Placentae | Dark red, continuous, may be concealed | Severe, sudden onset | Firm, board-like, tender | Often compromised, bradycardia |
| Cord Prolapse | May have bloody show | Variable | Normal initially | Severe bradycardia, variable decelerations |
| Vasa Previa | Painless bleeding with rupture of membranes | Absent | Normal | Sudden severe compromise |
Red Flag Signs
- Sudden onset of severe abdominal pain
- Rigid, board-like abdomen
- Persistent fetal bradycardia
- Maternal hypotension with tachycardia
- Absence of fetal movement
- Port-wine colored amniotic fluid
Assessment Priorities
- Continuous fetal heart rate monitoring
- Maternal vital signs every 15 minutes
- Estimate blood loss accurately
- Assess uterine activity and tone
- Monitor for signs of shock
- Laboratory studies (CBC, PT/PTT, fibrinogen)
Nursing Assessment
Primary Assessment
- Airway, Breathing, Circulation
- Level of consciousness
- Vital signs and hemodynamic status
- Oxygen saturation
- Fetal heart rate and activity
- Amount and character of bleeding
Focused Assessment
- Obstetric history and risk factors
- Onset and progression of symptoms
- Pain assessment (location, quality, intensity)
- Uterine palpation and measurement
- Leopold’s maneuvers
- Cervical examination (if safe)
Ongoing Monitoring
- Continuous electronic fetal monitoring
- Intake and output measurement
- Serial blood pressure checks
- Laboratory value trends
- Signs of coagulopathy
- Emotional and psychological status
Assessment Contraindications
Absolutely Contraindicated:
- Digital vaginal examination in suspected placenta previa
- Fundal pressure in cord prolapse
- Enemas or suppositories with placental bleeding
Use Caution:
- Abdominal palpation in suspected abruption
- Speculum examination with active bleeding
- Internal fetal monitoring placement
Nursing Interventions
Emergency Interventions
Immediate Actions:
- Assess maternal and fetal status
- Establish IV access with large bore catheter
- Position patient appropriately (left lateral)
- Administer oxygen 8-10 L/min via face mask
- Notify physician immediately
- Prepare for emergency delivery if indicated
For Cord Prolapse:
- Do NOT handle the cord
- Position in knee-chest or Trendelenburg
- Apply gentle upward pressure on presenting part
- Keep cord moist with sterile saline
- Prepare for immediate cesarean delivery
- Maintain cord viability until delivery
Supportive Care Interventions
Hemodynamic Support:
- Monitor vital signs every 15 minutes
- Maintain adequate circulating volume
- Administer blood products as ordered
- Watch for signs of shock
- Assess for coagulopathy
Fetal Monitoring:
- Continuous electronic fetal monitoring
- Document fetal heart rate patterns
- Assess for variable decelerations
- Monitor for signs of fetal distress
- Prepare for immediate delivery if needed
Comfort Measures:
- Provide emotional support
- Explain procedures to patient
- Maintain patient dignity
- Include family in care decisions
- Administer pain medication as ordered
Pharmacological Interventions
| Medication | Indication | Nursing Considerations |
|---|---|---|
| Betamethasone | Fetal lung maturation (24-34 weeks) | Monitor blood glucose, administer deep IM |
| Magnesium Sulfate | Neuroprotection, tocolysis | Monitor reflexes, respiratory rate, urine output |
| Terbutaline | Emergency tocolysis | Monitor heart rate, blood pressure |
| RhoGAM | Rh-negative mothers | Administer within 72 hours of bleeding |
Management Strategies
Conservative Management
Indications:
- Stable maternal and fetal status
- Minimal bleeding
- Preterm gestation (<34 weeks)
- No signs of labor
- Access to emergency care
Components:
- Bed rest with bathroom privileges
- Pelvic rest (no intercourse, tampons)
- Serial ultrasounds
- Fetal surveillance testing
- Corticosteroids for lung maturity
- Patient education
Surgical Management
Cesarean Delivery Indications:
- Active bleeding with hemodynamic instability
- Fetal distress or compromise
- Complete or partial placenta previa at term
- Failed conservative management
- Cord prolapse
- Placenta accreta spectrum disorders
Surgical Considerations:
- Blood and blood products available
- Anesthesia team preparation
- Neonatal resuscitation team
- Possible hysterectomy for placenta accreta
- Cell saver use when appropriate
- ICU availability if needed
Multidisciplinary Team Approach
Obstetrician
Diagnosis, management decisions, surgical intervention
Nursing Staff
Continuous monitoring, patient education, emotional support
Neonatologist
Preterm care planning, delivery room management
Blood Bank
Blood product preparation, massive transfusion protocol
Memory Aids & Mnemonics
PREVIA – Placenta Previa Assessment
- P – Painless bleeding
- R – Red, bright bleeding
- E – Examine with ultrasound (not digital)
- V – Vital signs monitoring
- I – IV access large bore
- A – Avoid vaginal exams
Key Teaching Point:
“Never perform a digital vaginal exam in suspected placenta previa – it could trigger massive hemorrhage!”
ABRUPT – Placental Abruption Signs
- A – Abdominal pain (severe, sudden)
- B – Bleeding (dark, may be concealed)
- R – Rigid, board-like uterus
- U – Uterine tenderness
- P – Preterm labor risk
- T – Tachycardia (maternal and fetal)
Clinical Pearl:
“Think abruption when you see the ‘3 Ps’: Pain, rigid uterus, and Port-wine colored amniotic fluid!”
PROLAPSE – Cord Prolapse Management
- P – Position (knee-chest or Trendelenburg)
- R – Relieve pressure on cord
- O – Oxygen to mother
- L – Lift presenting part off cord
- A – Avoid handling cord
- P – Prepare for emergency C-section
- S – Saline to keep cord moist
- E – Emergency notification
Emergency Rule:
“Time is brain! Every minute counts in cord prolapse – prepare for immediate delivery!”
RISKS – Common Risk Factors
- R – Repeat cesareans
- I – Increased maternal age
- S – Smoking and substance use
- K – Known previous complications
- S – Surgery (uterine) history
Prevention Focus:
“Identify high-risk patients early for enhanced surveillance and planning!”
Global Best Practices
World Health Organization (WHO) Recommendations
Prevention Strategies:
- Skilled birth attendance
- Emergency obstetric care access
- Blood transfusion services
- Antenatal care optimization
- Risk factor identification
- Community education programs
Quality Indicators:
- Decision-to-delivery time <30 minutes
- Blood loss estimation protocols
- Massive transfusion protocols
- Multidisciplinary team training
- Emergency drills and simulations
- Maternal mortality reviews
Nordic Countries Model of Care
Sweden, Norway, and Denmark have achieved remarkable outcomes in managing placental abnormalities through systematic approaches:
Centralized Care
- Regional referral centers
- Specialized obstetric units
- 24/7 expert availability
- Standardized protocols
Team Training
- Regular simulation exercises
- Interprofessional education
- Communication protocols
- Continuous competency assessment
Quality Assurance
- National registries
- Outcome monitoring
- Best practice sharing
- Research integration
UK MBRRACE-UK Initiative
The Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries program has identified key improvements:
Key Findings:
- Early recognition saves lives
- Communication failures are preventable
- Senior clinician involvement is crucial
- Massive transfusion protocols reduce mortality
- Family-centered care improves satisfaction
Recommended Actions:
- Structured handover protocols
- Early warning systems
- Consultant-led emergency care
- Regular case reviews
- Patient safety culture development
Australian National Approach
Australia’s comprehensive strategy focuses on rural and remote area challenges:
Innovation Highlights:
- Telehealth consultations for remote areas
- Flying Doctor Service for emergency transport
- Clinical networks linking rural and urban centers
- Shared care models between specialists and GPs
- Mobile ultrasound services for prenatal diagnosis
Universal Best Practice Principles
System-Level Factors:
- Standardized protocols and guidelines
- Regular training and simulation
- Quality improvement programs
- Multidisciplinary team approaches
- Technology integration (ultrasound, electronic records)
Individual Practice:
- Evidence-based decision making
- Continuous professional development
- Effective communication skills
- Cultural competency and sensitivity
- Family-centered care principles
Key Learning Points
Critical Nursing Actions
- • Early recognition and assessment of placental abnormalities
- • Immediate stabilization of maternal and fetal status
- • Effective communication with multidisciplinary team
- • Evidence-based interventions and monitoring
- • Emotional support and family-centered care
Safety Priorities
- • Never perform digital exam with suspected placenta previa
- • Recognize cord prolapse as obstetric emergency
- • Monitor for signs of hemorrhage and shock
- • Prepare for emergency delivery when indicated
- • Follow established protocols and guidelines
