Disorders of Uterine Action
A Comprehensive Guide for Nursing Students
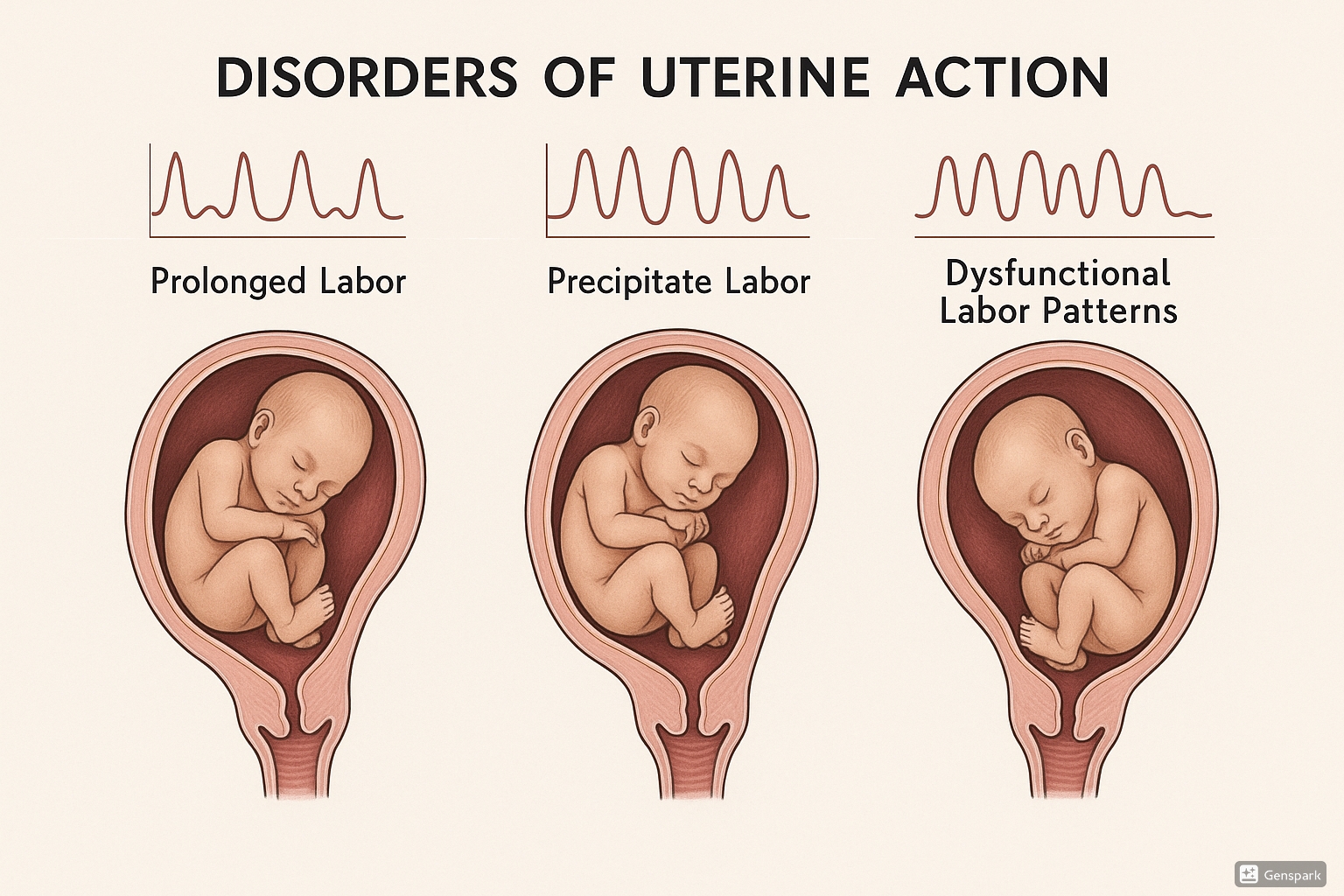
Table of Contents
Introduction to Disorders of Uterine Action
Disorders of uterine action refer to abnormalities in the contractions of the uterine muscles during labor, which can significantly impact labor progression and outcomes for both mother and baby. These disorders are common causes of challenging labor experiences and may necessitate medical interventions to ensure safe delivery.
Understanding these disorders is crucial for nursing students and healthcare professionals as they represent significant causes of maternal and fetal morbidity worldwide. Disorders of uterine action are classified into three primary categories:
- Prolonged labor – Labor that exceeds the expected duration
- Precipitate labor – Abnormally rapid labor progression
- Dysfunctional labor – Abnormal uterine contraction patterns that impede normal labor progression
Normal Labor Physiology
Before diving into disorders of uterine action, it’s essential to understand normal labor physiology as a baseline for comparison. Normal labor progresses through three distinct stages:
The Three Stages of Labor:
-
First Stage: From the onset of regular contractions to complete cervical dilation (10 cm)
- Latent phase: 0-3 cm dilation, contractions mild and infrequent
- Active phase: 4-7 cm dilation, contractions stronger and more frequent
- Transition phase: 8-10 cm dilation, contractions intense and frequent
- Second Stage: From complete cervical dilation to delivery of the baby
- Third Stage: From delivery of the baby to delivery of the placenta
Normal labor is characterized by coordinated uterine contractions that increase in frequency, intensity, and duration as labor progresses. These contractions cause progressive cervical effacement and dilation, allowing for the descent of the fetus through the birth canal.
Memory Aid: “FIRM Progress”
To remember the characteristics of normal uterine contractions, think FIRM:
- Frequency: Increases from every 10-20 minutes to every 2-3 minutes
- Intensity: Strengthens from mild to strong
- Regularity: Becomes more consistent over time
- Moving: Results in progressive cervical change and fetal descent
Prolonged Labor
Prolonged labor, also known as labor dystocia or failure to progress, occurs when labor exceeds the expected time frame. According to current guidelines, prolonged labor is diagnosed when:
- The latent phase exceeds 20 hours in nulliparous women or 14 hours in multiparous women
- The active phase progresses at less than 1.2 cm/hr in nulliparous women or less than 1.5 cm/hr in multiparous women
- The second stage exceeds 3 hours in nulliparous women with epidural analgesia (or 2 hours without epidural) or 2 hours in multiparous women with epidural (or 1 hour without epidural)
Causes and Risk Factors of Prolonged Labor
Maternal Factors
- Advanced maternal age
- Primiparity (first-time birth)
- Cephalopelvic disproportion (CPD)
- Maternal exhaustion
- Dehydration or malnutrition
- Anxiety and psychological factors
- Previous uterine surgery
- Abnormal uterine contractions
Fetal Factors
- Macrosomia (large baby)
- Malpresentation (breech, face, brow)
- Malposition (occiput posterior, transverse)
- Multiple gestation
- Fetal anomalies
Memory Aid: “5 P’s of Prolonged Labor”
Remember the major causes of prolonged labor with the 5 P’s:
- Powers: Inadequate uterine contractions
- Passenger: Fetal size, presentation, or position
- Passage: Pelvic dimensions and soft tissue obstacles
- Pain: Excessive discomfort affecting voluntary efforts
- Psyche: Psychological factors (fear, anxiety)
Diagnosis and Assessment
Diagnosis of prolonged labor involves careful monitoring of labor progress using:
- Partogram for tracking cervical dilation and descent
- Electronic fetal monitoring (EFM) to assess fetal well-being
- Pelvic examination to evaluate cervical dilation, effacement, and fetal descent
- Intrauterine pressure catheter (IUPC) when needed to measure contraction strength
Clinical Pearl
The Friedman curve has traditionally been used to evaluate labor progress, but current research suggests that labor may progress more slowly than previously thought, particularly in the early active phase (4-6 cm). The 2014 ACOG/SMFM consensus statement redefined labor arrest as:
- ≥6 cm dilation with membrane rupture and
- 4 hours of adequate contractions (>200 Montevideo units) or
- 6 hours of inadequate contractions with no cervical change
Management and Nursing Care
Management of prolonged labor focuses on identifying and addressing the underlying cause:
Non-Pharmacological Interventions
- Position changes to optimize fetal position and pelvic dimensions
- Ambulation and mobility
- Adequate hydration and nutrition
- Emotional support and anxiety reduction
- Warm baths/showers for relaxation
- Emptying bladder regularly
Medical Interventions
- Amniotomy (artificial rupture of membranes)
- Oxytocin augmentation
- Pain management (epidural, analgesics)
- Cesarean delivery when indicated
- Instrumental delivery (forceps, vacuum) when appropriate
Nursing care for patients experiencing prolonged labor includes:
- Close monitoring of maternal vital signs and fetal heart rate patterns
- Accurate documentation of contraction frequency, duration, and intensity
- Regular cervical assessments to evaluate progress
- Emotional support and anxiety reduction measures
- Pain management assistance
- Fluid balance monitoring and maintenance
- Patient education about interventions and progress
Precipitate Labor
Precipitate labor is characterized by abnormally rapid labor progression, typically defined as labor that lasts less than 3 hours from onset of contractions to delivery. While a quick labor might seem advantageous, precipitate labor carries significant risks for both mother and baby.
Causes and Risk Factors
- Multiparity (having given birth multiple times previously)
- History of previous precipitate labor
- Abnormally strong uterine contractions
- Hypertonic uterine activity
- Decreased tissue resistance in the birth canal
- Small fetal size
- Induced labor with excessive oxytocin
- Abruptio placentae (may cause hypertonicity)
Memory Aid: “RAPID”
Remember key characteristics of precipitate labor with RAPID:
- Rapid progression (<3 hours total)
- Abnormally strong contractions
- Previous history increases risk
- Increased risk of trauma
- Dangerous for both mother and baby
Maternal and Fetal Consequences
Maternal Risks
- Lacerations of the cervix, vagina, or perineum
- Uterine rupture
- Postpartum hemorrhage
- Amniotic fluid embolism
- Psychological trauma from unexpected birth experience
- Placental abruption
Fetal/Neonatal Risks
- Birth trauma (intracranial hemorrhage)
- Hypoxia due to rapid compression
- Pneumothorax
- Aspiration of amniotic fluid
- Umbilical cord rupture or avulsion
- Unattended birth leading to hypothermia
Management and Nursing Care
Management of precipitate labor focuses on minimizing complications:
- Early recognition of rapid progress
- Preparation for immediate delivery
- Side-lying position to slow rapid descent
- Controlled pushing techniques
- Monitoring for signs of uterine rupture or fetal distress
- Preparation for potential neonatal resuscitation
- Careful inspection for birth canal lacerations after delivery
- Close monitoring for postpartum hemorrhage
Clinical Pearl
In cases where precipitate labor is anticipated based on history, consider earlier admission to the hospital for monitoring. For women with a history of precipitate labor who live far from medical facilities, sometimes temporary relocation closer to the hospital near term is recommended.
Nursing care for patients experiencing precipitate labor includes:
- Staying with the patient continuously
- Providing calm reassurance and guidance
- Preparing for immediate delivery
- Assisting with controlled pushing to reduce perineal trauma
- Continuous monitoring of fetal heart rate when possible
- Thorough assessment for birth canal trauma after delivery
- Close monitoring for signs of postpartum hemorrhage
- Detailed documentation of the rapid labor process
Dysfunctional Labor
Dysfunctional labor refers to abnormal uterine contraction patterns that interfere with the normal progress of labor. It is characterized by uncoordinated uterine activity that fails to efficiently dilate the cervix or advance the fetus through the birth canal. Dysfunctional labor is generally classified into two main types:
Hypertonic Uterine Dysfunction
Hypertonic uterine dysfunction is characterized by increased resting tone of the uterus with frequent, irregular, and uncoordinated contractions that are often painful but ineffective in dilating the cervix.
Key Characteristics:
- High baseline uterine tone (>15 mmHg)
- Frequent contractions (often >5 in 10 minutes)
- Irregular contraction pattern
- Uncoordinated contractions that are painful but ineffective
- Minimal cervical dilation despite painful contractions
- Often seen in the latent phase of labor
Hypotonic Uterine Dysfunction
Hypotonic uterine dysfunction is characterized by weak, infrequent contractions that fail to progress labor effectively. This pattern most commonly occurs in the active phase of labor.
Key Characteristics:
- Low-intensity contractions (<50 mmHg by IUPC)
- Infrequent contractions (often <2-3 in 10 minutes)
- Poor coordination between upper and lower uterine segments
- Slow or arrested cervical dilation
- Lack of fetal descent despite adequate dilation
- Often seen in the active phase of labor
| Characteristic | Hypertonic Dysfunction | Hypotonic Dysfunction |
|---|---|---|
| Timing in Labor | Usually latent phase | Usually active phase |
| Contraction Intensity | Often intense and painful | Weak, ineffective |
| Contraction Frequency | Frequent, often >5 in 10 min | Infrequent, <2-3 in 10 min |
| Resting Tone | Increased (>15 mmHg) | Normal or low (<10 mmHg) |
| Pain Level | Often severe, continuous | Mild to moderate, intermittent |
| Initial Management | Therapeutic rest, hydration | Oxytocin augmentation |
Memory Aid: “HI-LOW”
Remember the differences between hypertonic and hypotonic dysfunctional labor with HI-LOW:
- HIgh frequency, HIgh pain, HIgh tone = Hypertonic
- LOW frequency, LOW intensity, LOW progress = Hypotonic
Management Approaches
Hypertonic Dysfunction Management
- Therapeutic rest with sedation
- Hydration (IV fluids)
- Pain relief (epidural analgesia may help)
- Warm bath or shower for relaxation
- Avoiding early oxytocin (may worsen condition)
- Monitoring for maternal exhaustion
- Reassessment after rest period
Hypotonic Dysfunction Management
- Oxytocin augmentation
- Amniotomy if membranes intact
- Position changes to optimize fetal position
- Adequate hydration and nutrition
- Bladder emptying
- Continuous fetal monitoring
- Consideration of cesarean if no progress
Nursing care for patients with dysfunctional labor includes:
- Accurate assessment and documentation of contraction patterns
- Monitoring of maternal vital signs and fetal heart rate
- Providing pain management appropriate to the type of dysfunction
- Supporting maternal position changes to optimize labor
- Administering IV fluids and medications as ordered
- Emotional support and education about the labor process
- Preparation for potential interventions (oxytocin, amniotomy, cesarean)
Complications of Disorders of Uterine Action
Disorders of uterine action can lead to significant complications if not properly managed. These complications include:
Maternal Complications
- Postpartum hemorrhage due to uterine atony
- Birth canal trauma (cervical, vaginal, perineal lacerations)
- Uterine rupture, particularly in precipitate labor
- Increased risk of infection with prolonged labor
- Increased cesarean section rate
- Maternal exhaustion and psychological trauma
- Increased risk of postpartum depression
Fetal/Neonatal Complications
- Fetal distress and hypoxia
- Birth trauma (cephalohematoma, subgaleal hemorrhage)
- Meconium aspiration syndrome
- Increased NICU admission rates
- Neonatal sepsis (with prolonged rupture of membranes)
- Cord prolapse or compression
- Intrauterine fetal demise in severe cases
Best Practices and Recent Updates
Best Practice #1: Updated Labor Progress Assessment
Recent research has led to revised understanding of normal labor progression. The 2014 ACOG/SMFM consensus statement and subsequent guidelines recommend:
- Not diagnosing labor arrest until at least 6 cm dilation (active phase)
- Allowing more time before intervening – at least 4 hours of adequate contractions with ruptured membranes before diagnosing arrest
- Avoiding cesarean delivery for slow but progressive labor in the latent phase
- Using the WHO partogram with a 4-hour action line rather than a 2-hour action line
Best Practice #2: Avoiding Routine Interventions
Current evidence supports a more physiologic approach to labor management:
- Avoiding routine artificial rupture of membranes
- Limiting vaginal examinations to reduce infection risk
- Allowing oral intake during labor for low-risk women
- Encouraging mobility and upright positions throughout labor
- Using intermittent auscultation when appropriate instead of continuous electronic fetal monitoring
Best Practice #3: Patient-Centered Labor Support
Evidence consistently shows that continuous labor support improves outcomes:
- Continuous one-to-one nursing support reduces labor duration and intervention rates
- Integration of doulas into the care team has shown significant benefits
- Shared decision-making involving the patient in management choices
- Use of non-pharmacological pain management techniques before or alongside medication
- Creating a supportive environment that reduces anxiety and promotes physiologic birth
Conclusion
Disorders of uterine action represent significant challenges in labor and delivery care. As a nursing student, understanding the normal physiology of labor and the pathophysiology of these disorders is crucial for providing safe, evidence-based care to laboring patients.
Remember that each labor is unique, and careful assessment is needed to distinguish between normal variations and true disorders requiring intervention. By applying current best practices and focusing on patient-centered care, nurses can play a vital role in optimizing outcomes for mothers and babies experiencing disorders of uterine action.
Continuous learning and staying updated on evidence-based guidelines will enhance your ability to provide comprehensive care in these challenging clinical situations.
