Obstetrical Shock: Comprehensive Guide for Nursing Students
Understanding the critical aspects of obstetrical shock and the essential nursing interventions to improve maternal outcomes
Table of Contents
1. Introduction to Obstetrical Shock
Obstetrical shock represents a life-threatening emergency characterized by inadequate tissue perfusion and oxygenation, resulting in cellular dysfunction and potential organ failure in pregnant, laboring, or recently delivered women. As one of the leading causes of maternal mortality worldwide, obstetrical shock requires prompt recognition and aggressive management by healthcare providers, particularly nurses who are often at the frontline of obstetric care.
Understanding the unique physiological changes during pregnancy is essential to comprehending how obstetrical shock differs from shock in non-pregnant patients. Pregnancy induces significant cardiovascular adaptations, including increased blood volume, cardiac output, and reduced systemic vascular resistance. These normal physiological changes can mask early signs of shock, making timely recognition challenging.
This comprehensive guide aims to equip nursing students with essential knowledge regarding the pathophysiology, classification, clinical manifestations, diagnostic evaluation, management principles, and nursing interventions related to obstetrical shock. By mastering this knowledge, nurses can significantly contribute to reducing maternal morbidity and mortality through timely recognition and intervention.
2. Definition and Significance
Obstetrical shock is defined as an acute, life-threatening condition characterized by inadequate tissue perfusion resulting from circulatory failure in pregnant or recently delivered women. This critical condition represents the body’s inability to deliver sufficient oxygen and nutrients to vital organs, leading to cellular dysfunction and potentially irreversible organ damage if not promptly addressed.
The significance of obstetrical shock cannot be overstated in maternal healthcare:
- It contributes to approximately 25% of maternal deaths globally
- Obstetrical shock represents a preventable cause of maternal mortality in many cases
- Early recognition and intervention can dramatically improve outcomes
- It poses risks to both mother and fetus, with potential long-term consequences
- Understanding obstetrical shock is fundamental for all healthcare providers working in obstetric settings
While obstetrical shock shares fundamental pathophysiological mechanisms with other forms of shock, its unique aspects relate to the physiological adaptations of pregnancy, which can both mask early signs and complicate management. The dual-patient consideration (mother and fetus) further distinguishes obstetrical shock from other shock states and necessitates specialized approaches to care.
3. Epidemiology and Risk Factors
Global Burden
Obstetrical shock remains a significant contributor to maternal mortality worldwide, with substantial regional variations. In low-resource settings, the incidence of obstetrical shock is approximately 1 in 100 deliveries, while in high-resource settings, it occurs in approximately 1 in 300-500 deliveries. This disparity reflects differences in access to prenatal care, skilled birth attendants, and emergency obstetric services.
Risk Factors for Obstetrical Shock
| Category | Risk Factors | Associated Shock Type |
|---|---|---|
| Maternal Characteristics |
– Advanced maternal age (>35 years) – Grand multiparity (≥5 deliveries) – Adolescent pregnancy – Pre-existing medical conditions (hypertension, diabetes, cardiac disease) – History of postpartum hemorrhage |
Various |
| Pregnancy-Related Factors |
– Multiple gestation – Polyhydramnios – Placental abnormalities (placenta previa, placenta accreta spectrum) – Prolonged labor – Macrosomia |
Primarily Hypovolemic |
| Delivery-Related Factors |
– Cesarean delivery (especially emergency) – Instrumental delivery – Uterine atony – Genital tract trauma – Retained placental tissue |
Hypovolemic |
| Infectious Causes |
– Chorioamnionitis – Endometritis – Prolonged rupture of membranes – Urinary tract infections – Poor aseptic techniques during procedures |
Septic |
| Medication-Related |
– Oxytocin overdose – Anesthetic agents – Tocolytic medications – Medication allergies |
Anaphylactic, Cardiogenic |
| Healthcare System Factors |
– Limited access to prenatal care – Lack of skilled birth attendants – Delayed referral systems – Inadequate emergency obstetric care – Lack of blood banking facilities |
Various |
Recognizing these risk factors is crucial for nurses providing obstetric care. Risk assessment should be performed during prenatal visits, upon admission to labor and delivery units, and continuously throughout the intrapartum and postpartum periods. Identified risk factors should trigger heightened surveillance and preparedness for potential obstetrical shock, with appropriate preventive measures implemented proactively.
4. Pathophysiology of Obstetrical Shock
Normal Physiologic Changes in Pregnancy
To understand obstetrical shock, it’s essential to first recognize the normal cardiovascular adaptations that occur during pregnancy:
Cardiovascular Changes
- Blood volume increases by 40-50% (1500-2000 mL)
- Plasma volume increases disproportionately to RBC mass
- Cardiac output increases by 30-50%
- Heart rate increases by 10-20 bpm
- Systemic vascular resistance decreases
- Blood pressure slightly decreases in the second trimester
Hematologic Changes
- Physiologic anemia of pregnancy (hemodilution)
- Hypercoagulable state develops
- White blood cell count increases
- Fibrinogen and clotting factors increase
- Enhanced inflammatory response
- Decreased fibrinolysis
Pathophysiologic Mechanisms of Obstetrical Shock
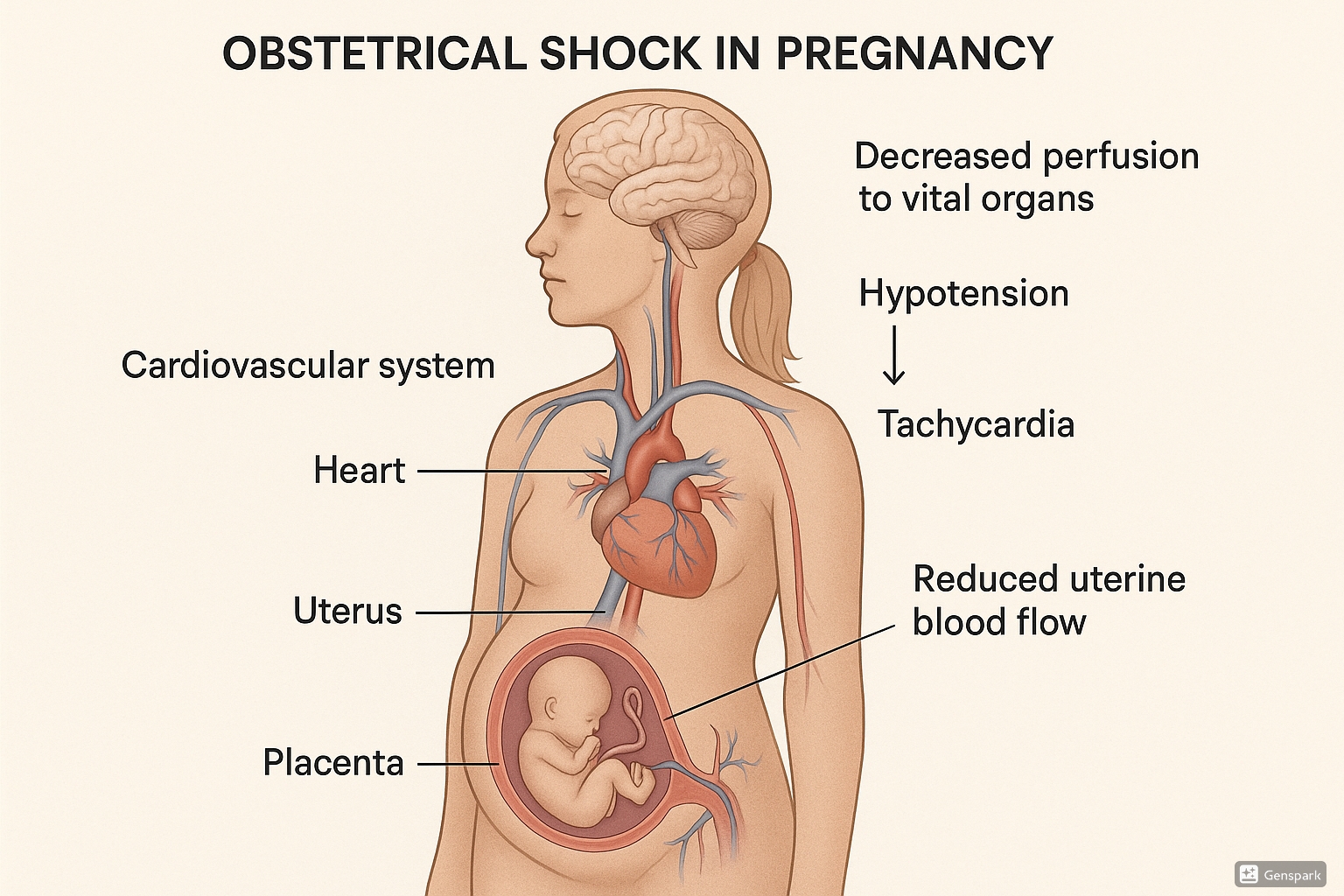
Figure 1: Physiological changes in obstetrical shock showing decreased perfusion to vital organs, hypotension, tachycardia, and reduced uterine blood flow
The general pathophysiology of obstetrical shock follows the common pathway of other shock states but with important distinctions due to pregnancy:
- Initial Insult: A precipitating event (e.g., hemorrhage, sepsis) disrupts normal cardiovascular function, leading to decreased tissue perfusion.
-
Compensatory Mechanisms: The body responds with:
- Sympathetic nervous system activation (increased heart rate, vasoconstriction)
- Renin-angiotensin-aldosterone system activation
- Release of antidiuretic hormone
- Redistribution of blood flow (away from non-vital organs including the uterus)
-
Cellular Dysfunction: As shock progresses, cellular metabolism shifts from aerobic to anaerobic, resulting in:
- Lactic acid production and metabolic acidosis
- ATP depletion
- Cellular membrane dysfunction
- Release of inflammatory mediators
-
Multiple Organ Dysfunction: Without timely intervention, progressive organ failure develops:
- Renal failure (decreased glomerular filtration)
- Hepatic dysfunction
- Respiratory failure (ARDS)
- Cardiovascular collapse
- Uteroplacental insufficiency
- Coagulopathy (DIC)
Unique Aspects of Shock in Pregnancy
Pregnancy-Specific Considerations:
- Increased baseline blood volume masks early signs of hypovolemia (can lose 30-35% of blood volume before clinical signs appear)
- Supine hypotensive syndrome (aortocaval compression) can exacerbate decreased cardiac output
- Uteroplacental circulation lacks autoregulation and suffers early in shock states
- Fetal compromise serves as an early indicator of maternal decompensation
- Physiologic hypercoagulability increases risk for DIC and thrombotic complications
- Enhanced inflammatory response can accelerate progression in septic shock
Progression of Obstetrical Shock
(Reversible)
(Irreversible)
Understanding the pathophysiology of obstetrical shock is crucial for nurses to recognize early signs, implement timely interventions, and prevent progression to irreversible stages. The knowledge of normal physiological adaptations in pregnancy helps nurses distinguish between normal findings and early manifestations of shock, which can be subtle and easily missed.
5. Classification of Obstetrical Shock
Obstetrical shock is classified based on the underlying pathophysiologic mechanism. Each type presents with distinct etiologies, clinical manifestations, and management approaches. Understanding these classifications is essential for accurate diagnosis and appropriate intervention.
| Type of Shock | Primary Mechanism | Common Obstetrical Causes | Frequency in Obstetrical Practice |
|---|---|---|---|
| Hypovolemic Shock | Decreased intravascular volume | Postpartum hemorrhage, placental abruption, placenta previa, uterine rupture | Most common (75-80% of obstetrical shock cases) |
| Septic Shock | Systemic inflammatory response to infection | Chorioamnionitis, endometritis, septic abortion, pyelonephritis | Second most common (15-20% of cases) |
| Cardiogenic Shock | Pump failure | Peripartum cardiomyopathy, myocardial infarction, valvular disease, amniotic fluid embolism | Rare (3-5% of cases) |
| Anaphylactic Shock | Severe allergic reaction | Medication reactions (antibiotics, anesthetics), latex allergy | Very rare (<1% of cases) |
| Neurogenic Shock | Loss of sympathetic tone | Spinal/epidural anesthesia complications, spinal cord injury | Extremely rare (<0.5% of cases) |
5.1 Hypovolemic Shock
Hypovolemic shock is the most common type of obstetrical shock, characterized by inadequate intravascular volume resulting in reduced cardiac output and tissue perfusion. During pregnancy, a woman can lose up to 30-35% of her blood volume before showing overt signs of shock due to the increased physiological blood volume.
Primary Obstetrical Causes:
- Postpartum hemorrhage: Accounts for approximately 80% of hypovolemic shock cases in obstetrics
- Placental abruption: Premature separation of placenta leading to concealed or visible hemorrhage
- Placenta previa: Abnormal placental implantation over or near the cervical os
- Uterine rupture: Disruption of uterine integrity, often at the site of previous cesarean scar
- Ectopic pregnancy: Implantation outside the uterine cavity, most commonly in fallopian tubes
- Coagulopathies: DIC, HELLP syndrome
Stages of Hypovolemic Shock:
| Parameter | Class I (≤15% loss) |
Class II (15-30% loss) |
Class III (30-40% loss) |
Class IV (>40% loss) |
|---|---|---|---|---|
| Blood Loss (mL)* | ≤750 | 750-1500 | 1500-2000 | >2000 |
| Heart Rate | <100 | 100-120 | 120-140 | >140 |
| Blood Pressure | Normal | Normal/Slight ↓ | ↓ | Severely ↓ |
| Respiratory Rate | 14-20 | 20-30 | 30-40 | >40 |
| Capillary Refill | Normal | Delayed | Delayed | Absent |
| Urine Output | Normal | 20-30 mL/hr | 5-15 mL/hr | Negligible |
| Mental Status | Alert | Mild anxiety | Confused, agitated | Lethargic/coma |
*Based on 5000 mL estimated blood volume for a 70 kg pregnant woman at term
Mnemonic: “4 T’s for PPH”
The common causes of postpartum hemorrhage can be remembered using the “4 T’s”:
- Tone: Uterine atony (70-80% of cases)
- Trauma: Lacerations, hematomas, inversions, rupture (15-20%)
- Tissue: Retained placental tissue (5-10%)
- Thrombin: Coagulation disorders (rare, 1-2%)
Management Priorities:
- Rapid identification of the source of hemorrhage
- Volume resuscitation (crystalloids, colloids, blood products)
- Oxygen supplementation to improve tissue oxygenation
- Positioning (left lateral to minimize aortocaval compression)
- Hemostatic interventions specific to the cause
- Continuous maternal and fetal monitoring (if antepartum)
5.2 Septic Shock
Septic shock in obstetrics is a severe manifestation of infection characterized by a systemic inflammatory response, vasodilation, increased capillary permeability, and eventual organ dysfunction. The physiological changes of pregnancy, including decreased cell-mediated immunity and increased susceptibility to certain pathogens, can accelerate the progression to septic shock.
Primary Obstetrical Causes:
- Chorioamnionitis: Infection of the amniotic fluid and fetal membranes
- Endometritis: Inflammation and infection of the endometrium, typically postpartum
- Septic abortion: Infection following incomplete abortion or retained products of conception
- Pyelonephritis: Kidney infection, more common during pregnancy
- Necrotizing fasciitis: Severe soft tissue infection, rare but can occur post-cesarean
- Toxic shock syndrome: Associated with retained foreign bodies (e.g., tampons, sponges)
Common Pathogens in Obstetrical Sepsis:
- Group A Streptococcus: Highly virulent, associated with rapid progression
- E. coli: Common in urinary tract infections and chorioamnionitis
- Bacteroides species: Anaerobic bacteria associated with endometritis
- Listeria monocytogenes: Can cause intrauterine infection
- Clostridium species: Associated with septic abortion and gas gangrene
Clinical Progression in Septic Shock:
| Stage | Clinical Findings | Pathophysiology |
|---|---|---|
| SIRS (Systemic Inflammatory Response Syndrome) |
– Temperature >38°C or <36°C – Heart rate >90 bpm – Respiratory rate >20/min – WBC >12,000 or <4,000 or >10% bands |
Inflammatory mediator release, early compensatory mechanisms |
| Sepsis | SIRS + confirmed or suspected infection | Ongoing inflammation, cytokine cascade |
| Severe Sepsis | Sepsis + organ dysfunction (e.g., oliguria, altered mental status, hypoxemia) | Tissue hypoperfusion, microvascular dysfunction |
| Septic Shock | Severe sepsis + persistent hypotension despite adequate fluid resuscitation | Profound vasodilation, myocardial depression, endothelial damage |
| Multiple Organ Dysfunction Syndrome (MODS) | Progressive failure of ≥2 organ systems | End-stage septic shock, widespread cellular injury |
Mnemonic: “SEPSIS”
Key components of septic shock management:
- Source control (identify and eliminate infection source)
- Early antibiotics (broad-spectrum within 1 hour)
- Perfusion optimization (fluids and vasopressors)
- Support organ function (respiratory, renal)
- Intensive monitoring (hemodynamic, laboratory)
- Survival bundles implementation (evidence-based protocols)
Management Priorities:
- Prompt initiation of broad-spectrum antibiotics within 1 hour of recognition
- Source control (e.g., evacuation of infected products, drainage of abscesses)
- Aggressive fluid resuscitation (30 mL/kg crystalloid within 3 hours)
- Vasopressor support if hypotension persists after fluid resuscitation
- Serum lactate measurement and monitoring
- Consideration for delivery if antepartum (especially beyond 34 weeks)
5.3 Cardiogenic Shock
Cardiogenic shock in the obstetrical setting results from primary cardiac dysfunction leading to inadequate cardiac output and tissue hypoperfusion. While relatively rare in obstetrics, it carries a high mortality rate and requires prompt recognition and specialized management.
Primary Obstetrical Causes:
- Peripartum cardiomyopathy: Heart failure in the last month of pregnancy or within 5 months postpartum
- Amniotic fluid embolism: Entry of amniotic fluid into the maternal circulation leading to cardiovascular collapse
- Myocardial infarction: Increasing incidence due to advanced maternal age and comorbidities
- Valvular disease: Mitral stenosis may decompensate during pregnancy due to increased cardiac output demands
- Cardiomyopathy associated with preeclampsia: Severe preeclampsia can occasionally lead to cardiac dysfunction
Hemodynamic Profile:
| Parameter | Non-pregnant Values | Normal Pregnancy | Cardiogenic Shock in Pregnancy |
|---|---|---|---|
| Cardiac Output | 4-6 L/min | 6-8 L/min | <4 L/min |
| Stroke Volume | 60-100 mL | 70-120 mL | Decreased |
| Pulmonary Capillary Wedge Pressure | 6-12 mmHg | 6-12 mmHg | >18 mmHg |
| Systemic Vascular Resistance | 800-1200 dyn·s/cm5 | 600-800 dyn·s/cm5 | Elevated |
| Left Ventricular Ejection Fraction | >55% | >55% | <40% |
Clinical Features:
Cardiogenic shock in pregnancy presents with:
- Dyspnea, orthopnea, paroxysmal nocturnal dyspnea
- Hypotension unresponsive to fluid administration
- Signs of pulmonary edema (crackles, hypoxemia)
- Jugular venous distention
- S3 gallop, murmurs in valvular disease
- Peripheral edema and cool extremities
- Altered mental status due to cerebral hypoperfusion
Management Considerations:
- Position patient in left lateral position to reduce aortocaval compression
- Oxygen supplementation to maintain SpO2 >95%
- Judicious fluid management (often restriction rather than bolus)
- Inotropic support (dobutamine, milrinone) to improve cardiac contractility
- Vasopressors with inotropic properties (norepinephrine)
- Management of pulmonary edema (diuretics, preload/afterload reduction)
- Consideration for mechanical circulatory support in severe cases
- Multidisciplinary approach involving cardiology, maternal-fetal medicine, and critical care
5.4 Anaphylactic Shock
Anaphylactic shock is a severe, life-threatening systemic hypersensitivity reaction characterized by bronchospasm, vasodilation, increased vascular permeability, and eventual cardiovascular collapse. While rare in obstetrics, it requires immediate recognition and treatment to prevent maternal and fetal morbidity and mortality.
Common Triggers in Obstetrical Settings:
- Medications:
- Antibiotics (particularly β-lactams, sulfonamides)
- Local anesthetics
- Neuromuscular blocking agents (during cesarean delivery)
- NSAIDs
- Oxytocic agents (rarely)
- Latex: Exposure during examinations, procedures, or delivery
- Colloid solutions: Dextrans, gelatins, or albumin
- Blood products: Transfusion reactions
Clinical Presentation:
| System | Manifestations |
|---|---|
| Cutaneous | Urticaria, angioedema, flushing, pruritus |
| Respiratory | Dyspnea, bronchospasm, stridor, laryngeal edema, respiratory arrest |
| Cardiovascular | Tachycardia, hypotension, arrhythmias, cardiovascular collapse |
| Gastrointestinal | Nausea, vomiting, abdominal cramps, diarrhea |
| Neurological | Anxiety, sense of impending doom, confusion, loss of consciousness |
| Obstetrical | Uterine contractions, fetal distress |
Emergency Management – ABCDE Approach:
- Airway: Assess and secure airway; be prepared for intubation if laryngeal edema present
- Breathing: Administer oxygen, monitor oxygen saturation, treat bronchospasm
- Circulation: Establish IV access, administer epinephrine, position patient in left lateral position
- Disability: Assess neurological status, monitor level of consciousness
- Exposure: Remove allergen if possible, assess for cutaneous manifestations
Mnemonic: “AAAAA” for Anaphylaxis Management
- Awareness and early recognition
- Adrenaline (epinephrine) 0.3-0.5 mg IM (1:1000)
- Airway management and oxygen
- Additional therapies (antihistamines, corticosteroids, β-agonists)
- Advanced life support if needed
Pharmacological Interventions:
| Medication | Dose | Route | Frequency | Mechanism |
|---|---|---|---|---|
| Epinephrine | 0.3-0.5 mg (1:1000) | IM (anterolateral thigh) | Every 5-15 min as needed | α and β adrenergic effects: vasoconstriction, bronchodilation, increased cardiac output |
| Diphenhydramine | 25-50 mg | IV/IM | Every 6 hours | H₁ antagonist: reduces histamine-mediated symptoms |
| Ranitidine | 50 mg | IV | Every 8 hours | H₂ antagonist: augments H₁ blockade |
| Methylprednisolone | 125 mg | IV | Once, then as needed | Prevents biphasic or protracted reactions |
| Albuterol | 2.5-5 mg in 3 mL NS | Nebulized | Every 20 min as needed | β₂-agonist: bronchodilation |
Following successful management of anaphylactic shock in pregnancy, detailed documentation of the reaction, causative agent, and management should be provided for future reference. Consultation with an allergist is recommended during the postpartum period for confirmatory testing and prevention strategies.
5.5 Neurogenic Shock
Neurogenic shock is a rare form of distributive shock in obstetrics resulting from disruption of sympathetic nervous system pathways. It is characterized by vasodilation without the compensatory tachycardia typically seen in other forms of shock due to concurrent loss of sympathetic cardiac innervation.
Obstetrical Causes:
- Spinal/epidural anesthesia: High or total spinal anesthesia causing sympathetic blockade
- Spinal cord injury: Trauma during pregnancy or delivery
- Central nervous system lesions: Rare causes affecting brainstem or spinal pathways
Distinctive Clinical Features:
Classic Triad in Neurogenic Shock:
- Hypotension: Due to loss of sympathetic tone and vasodilation
- Bradycardia: Due to unopposed vagal tone (differentiates from other shock types)
- Warm, dry skin: Due to peripheral vasodilation without compensatory vasoconstriction
Management Principles:
- Positioning: Left lateral position to reduce aortocaval compression
- Fluid resuscitation: Crystalloids to support intravascular volume
- Vasopressors:
- Phenylephrine: α₁-adrenergic agonist (preferred in pregnancy)
- Norepinephrine: For refractory cases
- Atropine: For symptomatic bradycardia
- Trendelenburg position: May help temporarily redistribute blood volume
- Treatment of underlying cause: May include reducing level of spinal anesthesia when possible
Prevention in Regional Anesthesia:
- Adequate prehydration before spinal/epidural anesthesia
- Careful titration of local anesthetic dose
- Slow incremental dosing in epidural anesthesia
- Vigilant monitoring during and after regional anesthesia placement
- Immediate availability of resuscitation equipment and vasopressors
6. Clinical Manifestations
Recognizing the clinical manifestations of obstetrical shock is critical for early intervention. The presenting signs and symptoms vary depending on the type of shock, its severity, and individual patient factors. Due to the physiological adaptations of pregnancy, early signs may be subtle or masked until significant decompensation has occurred.
General Signs and Symptoms
| System | Early Signs | Late Signs |
|---|---|---|
| Cardiovascular |
– Tachycardia (>100 bpm) – Narrow pulse pressure – Orthostatic hypotension |
– Hypotension (SBP <90 mmHg) – Weak, thready pulse – Arrhythmias |
| Respiratory |
– Tachypnea (>20 breaths/min) – Mild dyspnea |
– Respiratory distress – Hypoxemia – Pulmonary edema (cardiogenic) |
| Renal |
– Decreased urine output (<30 mL/hr) – Concentrated urine |
– Oliguria/anuria (<0.5 mL/kg/hr) – Elevated BUN/creatinine |
| Neurological |
– Anxiety, restlessness – Confusion – Irritability |
– Lethargy – Obtundation – Coma |
| Skin |
– Cool extremities – Delayed capillary refill (>3 seconds) – Pallor |
– Cyanosis – Mottling – Cold, clammy skin |
| Obstetrical/Fetal |
– Uterine tenderness (abruption) – Non-reassuring fetal heart rate – Minimal vaginal bleeding |
– Severe hemorrhage – Fetal bradycardia – Absent fetal movement |
Specific Manifestations by Shock Type
Hypovolemic Shock:
- Visible hemorrhage (vaginal bleeding, hematuria)
- Signs of concealed bleeding (increasing abdominal girth, Cullen’s sign)
- Extreme thirst
- Compensatory tachycardia and vasoconstriction
- Small, collapsing pulse
- Postural hypotension progressing to supine hypotension
Septic Shock:
- Fever (>38°C) or hypothermia (<36°C)
- Warm, flushed skin (early)
- Hyperdynamic state initially (warm shock): increased cardiac output, decreased systemic vascular resistance
- Later progression to cold shock: decreased cardiac output, vasoconstriction
- Specific signs related to infection source:
- Uterine tenderness and malodorous discharge in endometritis
- Flank pain and costovertebral angle tenderness in pyelonephritis
- Erythema and local tenderness in wound infections
- Altered mental status disproportionate to fever
Cardiogenic Shock:
- Pulmonary edema with crackles on auscultation
- Jugular venous distention
- S3 gallop on cardiac auscultation
- Peripheral edema
- Chest pain (in myocardial infarction)
- Prominent cardiac murmurs (in valvular disease)
- Increased work of breathing, orthopnea
Anaphylactic Shock:
- Rapid onset following exposure to trigger
- Urticaria, angioedema, cutaneous flushing
- Stridor, wheezing, respiratory distress
- Oropharyngeal or laryngeal edema
- Gastrointestinal symptoms (nausea, vomiting, abdominal pain)
- Sense of impending doom
Neurogenic Shock:
- Bradycardia with hypotension (distinguishing feature)
- Warm, dry skin due to vasodilation
- Sharp line of demarcation between warm and normal skin corresponding to level of sympathetic denervation
- Sensory and motor deficits below level of injury
Mnemonic: “SHOCK” Signs
Critical signs to monitor in obstetrical shock:
- Systolic pressure (decreased)
- Heart rate (increased, except in neurogenic shock)
- Oxygen saturation (decreased)
- Capillary refill (delayed)
- Kidney output (decreased urine production)
Important Consideration – Compensatory Mechanisms:
Pregnancy-induced physiological changes can mask shock until significant decompensation has occurred. A pregnant woman can lose up to 30-35% of her blood volume before showing overt signs of hypotension due to:
- Increased baseline blood volume (40-50% above non-pregnant state)
- Enhanced baroreceptor sensitivity
- Increased sympathetic tone
- Redistribution of blood flow away from non-essential organs
This physiologic reserve protects the mother but may delay shock recognition. Therefore, rely on trends in vital signs rather than absolute values, and maintain a high index of suspicion in at-risk patients.
Fetal Manifestations
The fetus is highly sensitive to maternal shock states due to its dependence on adequate uteroplacental perfusion. Monitoring fetal response can provide early indication of maternal compromise:
- Early signs:
- Increased baseline fetal heart rate
- Decreased fetal heart rate variability
- Absence of accelerations
- Late signs:
- Late decelerations
- Prolonged decelerations
- Fetal bradycardia
- Sinusoidal pattern
Recognition of the diverse clinical manifestations of obstetrical shock enables nurses to identify early warning signs and initiate timely interventions. A systematic approach to assessment, focusing on both maternal and fetal indicators, is crucial for improving outcomes in this life-threatening condition.
7. Diagnostic Evaluation
Prompt and accurate diagnostic evaluation of obstetrical shock is essential for guiding appropriate management strategies. Diagnostic approaches should be tailored to the suspected etiology while maintaining a broad perspective to identify any underlying or concurrent conditions.
Initial Assessment
Vital Sign Monitoring:
- Continuous monitoring of blood pressure, heart rate, respiratory rate, and oxygen saturation
- Temperature monitoring (particularly important in septic shock)
- Urine output measurement via indwelling catheter
- Continuous fetal monitoring when applicable
Physical Examination:
- Comprehensive evaluation focusing on potential sources of shock
- Assessment of mental status, skin perfusion, and capillary refill
- Evaluation for vaginal bleeding, abdominal tenderness, and uterine tone
- Cardiac and pulmonary examination for signs of fluid overload or cardiac dysfunction
- Inspection of surgical sites or invasive procedure locations for signs of infection
Point-of-Care Testing:
- Bedside glucose measurement
- Urine dipstick analysis
- Capillary blood gas analysis
- Point-of-care hemoglobin/hematocrit measurement
- Lactate measurement (portable analyzers)
Laboratory Studies
| Category | Tests | Clinical Significance |
|---|---|---|
| Complete Blood Count | Hemoglobin, hematocrit, white blood cell count with differential, platelet count |
– Decreased Hgb/Hct in hemorrhagic shock – Elevated or decreased WBC in septic shock – Thrombocytopenia may indicate DIC or HELLP syndrome |
| Coagulation Studies | PT/INR, PTT, fibrinogen, D-dimer |
– Prolonged clotting times suggest coagulopathy – Decreased fibrinogen and elevated D-dimer indicate DIC – Critical in obstetric hemorrhage management |
| Chemistry Panel | Electrolytes, BUN, creatinine, glucose, liver function tests |
– Elevated BUN/creatinine suggests renal hypoperfusion – Elevated liver enzymes may indicate HELLP syndrome or hypoperfusion – Electrolyte abnormalities common in shock states |
| Arterial Blood Gas | pH, PaO₂, PaCO₂, HCO₃⁻, lactate |
– Metabolic acidosis with elevated lactate indicates tissue hypoperfusion – Respiratory alkalosis may be an early sign of sepsis – Mixed acid-base disorders common in advanced shock |
| Inflammatory Markers | C-reactive protein, procalcitonin |
– Elevated in inflammatory conditions, particularly sepsis – Can help differentiate infectious from non-infectious causes |
| Cardiac Markers | Troponin, BNP |
– Elevated in cardiogenic shock or myocardial strain – BNP elevated in heart failure or peripartum cardiomyopathy |
| Microbiology | Blood cultures, urine culture, vaginal/cervical cultures, wound cultures |
– Critical for identifying causative organisms in septic shock – Should be obtained before antibiotic administration when possible |
Imaging Studies
Ultrasound:
- Bedside obstetric ultrasound:
- Assessment of placental location and integrity
- Fetal viability and presentation
- Amniotic fluid assessment
- Detection of concealed abruption or hemoperitoneum
- FAST examination (Focused Assessment with Sonography in Trauma):
- Detection of free fluid in abdominal and pelvic spaces
- Assessment of pericardial effusion
- Evaluation of pleural spaces for hemothorax
- Echocardiography:
- Assessment of cardiac function and ejection fraction
- Evaluation of valvular function and wall motion
- Detection of pericardial effusion
- Estimation of central venous pressure
Radiographic Studies:
- Chest X-ray: Evaluation for pulmonary edema, pneumonia, or ARDS
- CT scan: When indicated for specific diagnoses (pulmonary embolism, hemorrhage source)
- MRI: Limited role in acute settings but may be useful for specific conditions
Radiation Safety Consideration:
While diagnostic imaging can provide valuable information, radiation exposure should be minimized during pregnancy. However, in life-threatening situations, necessary radiological studies should not be withheld. Proper shielding should be used when possible, and the benefits must outweigh the risks.
Advanced Monitoring
In severe or refractory obstetrical shock, advanced hemodynamic monitoring may be indicated:
Hemodynamic Monitoring Options:
| Monitoring Technique | Parameters Measured | Indications |
|---|---|---|
| Central Venous Pressure (CVP) |
– Right heart filling pressure – Central venous oxygen saturation |
– Guide fluid resuscitation – Central venous access for vasopressors – Monitor response to treatment |
| Arterial Line |
– Continuous blood pressure monitoring – Arterial blood sampling – Arterial waveform analysis |
– Hemodynamic instability – Frequent blood sampling needs – Vasopressor titration |
| Non-invasive Cardiac Output Monitoring |
– Cardiac output/index – Stroke volume/index – Systemic vascular resistance |
– Differentiate types of shock – Guide fluid vs. vasopressor therapy – Less invasive than pulmonary artery catheter |
| Pulmonary Artery Catheter |
– Pulmonary artery pressure – Pulmonary capillary wedge pressure – Mixed venous oxygen saturation – Cardiac output (thermodilution) |
– Complex shock states – Refractory shock – Cardiogenic shock – Pulmonary hypertension |
Diagnostic Approach by Shock Type
Hypovolemic Shock:
- Serial hemoglobin/hematocrit measurements
- Coagulation studies to assess for DIC
- Ultrasound to identify bleeding source
- Assessment of fluid responsiveness
Septic Shock:
- Comprehensive cultures before antibiotic administration
- Serum lactate measurements
- Inflammatory markers (CRP, procalcitonin)
- Imaging to identify infection source
Cardiogenic Shock:
- ECG to assess for ischemia or arrhythmias
- Echocardiography to evaluate cardiac function
- Cardiac biomarkers (troponin, BNP)
- Central hemodynamic measurements if available
Anaphylactic Shock:
- Tryptase levels (ideally within 1-3 hours of reaction)
- IgE testing when appropriate (delayed follow-up)
- Clinical diagnosis based on temporal relationship to exposure
Neurogenic Shock:
- Assessment of sensory and motor function
- Evaluation of sympathetic blockade level
- Imaging of spine if traumatic etiology suspected
Mnemonic: “DIAGNOSE Shock”
Essential diagnostic evaluations in obstetrical shock:
- Detailed history and physical examination
- Imaging appropriate for suspected etiology
- Arterial blood gas with lactate
- Glucose and other basic chemistry tests
- Note coagulation studies
- Obtain blood count and type/crossmatch
- Source identification for infection
- Evaluation of cardiac function when indicated
8. Management Principles
The management of obstetrical shock requires a systematic, multidisciplinary approach with simultaneous attention to both maternal stabilization and fetal well-being. Early recognition and intervention are critical to prevent progression to irreversible shock and end-organ damage.
General Principles
Initial Resuscitation – The “VIP” Approach:
-
Ventilation and Oxygenation:
- Ensure patent airway
- Administer oxygen to maintain SpO₂ >95%
- Consider early intubation in deteriorating patients
- Target oxygen delivery to tissues rather than just oxygen saturation
-
Infusion and Volume Resuscitation:
- Establish at least two large-bore IV access sites (16-18 gauge)
- Consider central venous access in severe cases
- Initiate crystalloid infusion (warmed if available)
- Early blood product administration in hemorrhagic shock
- Monitor response to fluid challenges
-
Positioning:
- Left lateral position or manual displacement of uterus to reduce aortocaval compression
- 30° left lateral tilt if CPR is required
- Avoid Trendelenburg position except in specific circumstances
Critical Interventions:
Maternal Priorities
- Continuous vital sign monitoring
- Strict input/output measurement
- Frequent reassessment of response to interventions
- Laboratory monitoring to guide resuscitation
- Temperature maintenance to prevent hypothermia
- Identification and treatment of the underlying cause
- Early involvement of specialists (obstetrics, critical care, anesthesia)
Fetal Considerations
- Continuous fetal monitoring when gestational age is viable
- Recognition that fetal distress often precedes maternal decompensation
- Awareness that maternal resuscitation is the priority for fetal well-being
- Preparation for emergency delivery if indicated
- Consideration of corticosteroids for fetal lung maturity if time permits
- Neonatal team preparation if delivery is anticipated
Delivery Considerations:
In severe obstetrical shock, delivery may be necessary to optimize maternal resuscitation by:
- Improving venous return by relieving aortocaval compression
- Reducing oxygen demand (pregnancy increases oxygen consumption by 20%)
- Facilitating access to sources of hemorrhage
- Improving ability to perform essential interventions
The decision for emergency delivery should consider gestational age, maternal condition, and response to initial resuscitation efforts.
Specific Management by Shock Type
Hypovolemic Shock Management
| Element | Intervention |
|---|---|
| Fluid Resuscitation |
– Initial crystalloid bolus: 1-2 L warmed fluid – Reassess after each 500 mL – Transition to blood products early in hemorrhagic shock |
| Blood Product Administration |
– Packed RBCs: Maintain hemoglobin >7-8 g/dL – Plasma: Consider 1:1 or 1:2 ratio with RBCs in massive transfusion – Platelets: Maintain count >50,000/μL (>100,000/μL for CNS/ocular bleeding) – Cryoprecipitate/Fibrinogen concentrate: Maintain fibrinogen >200 mg/dL – Consider activation of massive transfusion protocol |
| Hemorrhage Control |
For postpartum hemorrhage: – Uterine massage and bimanual compression – Uterotonics (oxytocin, methylergonovine, prostaglandins) – Tranexamic acid (1g IV over 10 min within 3 hours of birth) – Intrauterine balloon tamponade – Surgical interventions (B-Lynch suture, uterine artery ligation) – Interventional radiology (uterine artery embolization) – Hysterectomy for refractory cases For antepartum hemorrhage: – Targeted management based on cause – Consider expedited delivery in severe cases |
| Prevention of Complications |
– Active warming to prevent hypothermia – Correction of acidosis – Calcium replacement with massive transfusion – Monitoring for and treating hyperfibrinolysis – Prevention of abdominal compartment syndrome |
Mnemonic: “HEMORRHAGE”
Management priorities in hemorrhagic shock:
- Help (activate team response)
- Establish IV access (two large-bore)
- Monitor vitals continuously
- Oxygen administration
- Resuscitate with fluids/blood
- Reverse coagulopathy
- Halt bleeding (find source)
- Assess response
- Gauze packing/surgical control
- Evaluate need for transfer/additional resources
Septic Shock Management
| Element | Intervention |
|---|---|
| Early Goal-Directed Therapy |
– Initial fluid resuscitation: 30 mL/kg crystalloid within 3 hours – Vasopressors if hypotension persists after fluid resuscitation – Target MAP ≥65 mmHg – Maintain ScvO₂ >70% if central line placed – Normalize lactate |
| Antimicrobial Therapy |
– Obtain cultures before antibiotics when possible – Administer broad-spectrum antibiotics within 1 hour – Consider combination therapy for multidrug-resistant organisms – Focus therapy based on culture results – Typically broader coverage than standard obstetric prophylaxis |
| Source Control |
– Identify and eliminate infectious source – Evacuation of retained products of conception – Drainage of abscesses – Debridement of infected/necrotic tissue – Removal of infected devices (catheters, IUDs) – Consider delivery in antepartum sepsis |
| Supportive Care |
– Stress-dose corticosteroids for refractory shock – Glycemic control (target 140-180 mg/dL) – Deep vein thrombosis prophylaxis – Lung-protective ventilation if intubated – Nutritional support |
Cardiogenic Shock Management
- Optimize Preload: Careful fluid administration guided by hemodynamic monitoring
- Improve Contractility:
- Inotropic support: Dobutamine (5-20 μg/kg/min)
- Milrinone for refractory cases (loading dose 50 μg/kg over 10 min, then 0.375-0.75 μg/kg/min)
- Reduce Afterload:
- Vasodilators if blood pressure allows (nitroglycerin, nitroprusside)
- Careful use in pregnancy with attention to uteroplacental perfusion
- Manage Arrhythmias: Treat underlying rhythm disturbances
- Mechanical Support: Consider in refractory cases
- Intra-aortic balloon pump
- Extracorporeal membrane oxygenation (ECMO)
- Ventricular assist devices
- Etiology-Specific Management:
- Peripartum cardiomyopathy: Standard heart failure therapy (modified for pregnancy status)
- Myocardial infarction: Consider urgent revascularization
- Valvular disease: Medical management, possible valvuloplasty in critical stenosis
- Amniotic fluid embolism: Supportive care, correction of coagulopathy
Anaphylactic Shock Management
- Remove Trigger: Discontinue suspected agent or exposure
- Epinephrine Administration:
- First-line therapy: 0.3-0.5 mg (0.3-0.5 mL of 1:1000) IM in anterolateral thigh
- May repeat every 5-15 minutes if needed
- IV epinephrine (0.1 mg over 5 min) for refractory cases under monitoring
- Fluid Resuscitation: Aggressive crystalloid administration (1-2 L rapidly)
- Position: Left lateral position to prevent aortocaval compression
- Adjunctive Therapies:
- H₁ antihistamines: Diphenhydramine 25-50 mg IV
- H₂ blockers: Ranitidine 50 mg IV
- Corticosteroids: Methylprednisolone 125 mg IV
- Albuterol nebulization for bronchospasm
- Continuous Monitoring: For biphasic reactions (up to 72 hours)
- Documentation: Careful documentation of reaction and causative agent
Neurogenic Shock Management
- Fluid Resuscitation: Judicious crystalloid administration
- Vasopressors:
- Phenylephrine (preferred in pregnancy): 100-180 μg/min, titrate to effect
- Norepinephrine for refractory cases: 0.1-0.3 μg/kg/min
- Atropine: For symptomatic bradycardia (0.5-1 mg IV)
- Positional Management: Left lateral position with slight head-down tilt if needed
- Management of Underlying Cause:
- For high spinal anesthesia: Support ventilation, reduce anesthetic level if possible
- For spinal cord injury: Immobilization, neurological consultation
9. Nursing Process in Obstetrical Shock
The nursing process provides a systematic framework for delivering comprehensive care to patients experiencing obstetrical shock. Each phase of this process is critical for ensuring optimal patient outcomes through early recognition, appropriate interventions, and ongoing evaluation.
9.1 Assessment
Initial Rapid Assessment
ABCDE Approach:
- Airway: Assess patency, presence of secretions or obstructions
- Breathing: Respiratory rate, depth, effort, oxygen saturation
- Circulation: Heart rate, blood pressure, capillary refill, pulse quality
- Disability: Level of consciousness, pupillary response, Glasgow Coma Scale
- Exposure: Visual inspection for bleeding, rash, or other physical signs
Comprehensive Assessment Parameters
| Assessment Component | Parameters to Evaluate | Significance in Obstetrical Shock |
|---|---|---|
| Vital Signs |
– Blood pressure – Heart rate – Respiratory rate – Temperature – Oxygen saturation – Pain level |
– Early tachycardia may be only initial sign – Hypotension may be late sign due to compensatory mechanisms – Fever suggests septic etiology – Hypothermia may indicate decompensated septic shock |
| Cardiovascular |
– Capillary refill – Jugular venous distention – Peripheral pulses – Heart sounds – ECG findings |
– Delayed capillary refill (>3 seconds) suggests hypoperfusion – JVD may indicate cardiogenic shock or volume overload – Weak, thready pulses suggest decreased stroke volume |
| Respiratory |
– Respiratory pattern – Use of accessory muscles – Lung sounds – Arterial blood gases |
– Tachypnea often precedes other signs of shock – Crackles may indicate pulmonary edema in cardiogenic shock – Metabolic acidosis indicates tissue hypoperfusion |
| Neurological |
– Level of consciousness – Orientation – Pupillary response – Motor function |
– Altered mental status may be early sign of inadequate cerebral perfusion – Confusion or agitation can precede hypotension – Lethargy indicates severe shock |
| Renal/Fluid Balance |
– Urine output – Urine color/concentration – Intake/output balance – Electrolyte values |
– Oliguria (<0.5 mL/kg/hr) indicates renal hypoperfusion – Concentrated, dark urine suggests dehydration – Electrolyte imbalances affect cardiac function |
| Obstetric-Specific |
– Uterine tone – Vaginal bleeding assessment – Fundal height – Lochia (postpartum) – Fetal heart rate/pattern – Placental assessment (if delivered) |
– Boggy uterus suggests atony – Visual estimation often underestimates blood loss – Non-reassuring fetal heart patterns may precede maternal decompensation – Placental abnormalities provide diagnostic clues |
| Integumentary |
– Skin color – Temperature – Moisture – Petechiae, ecchymosis |
– Pallor suggests anemia/blood loss – Cyanosis indicates severe hypoxia – Mottling suggests advanced shock state – Petechiae may suggest DIC |
| Laboratory Values |
– Hemoglobin/hematocrit – Coagulation studies – Lactate – Kidney/liver function – Blood cultures |
– Serial Hgb/Hct tracks blood loss – Coagulation abnormalities suggest DIC or severe hemorrhage – Lactate >4 mmol/L indicates tissue hypoperfusion – BUN/creatinine elevation suggests kidney injury |
Risk Factor Assessment
Identifying patients at risk for obstetrical shock enables preventive interventions and heightened surveillance:
Antepartum Risk Factors
- Placental abnormalities (previa, accreta)
- Multiple gestation
- Polyhydramnios
- Pre-eclampsia/HELLP syndrome
- Chorioamnionitis
- Previous cesarean deliveries
- Maternal comorbidities
Intrapartum Risk Factors
- Prolonged labor
- Precipitous delivery
- Augmented labor
- Instrumental delivery
- Emergency cesarean section
- Intrauterine fetal demise
- Maternal exhaustion
Postpartum Risk Factors
- Uterine atony
- Retained placental fragments
- Genital tract trauma
- Postpartum infection
- Amniotic fluid embolism
- Coagulopathies
Mnemonic: “SHOCK ASSESS”
Key assessment areas in obstetrical shock:
- Skin (color, temperature, moisture)
- Heart rate and blood pressure
- Oxygen saturation and respiratory status
- Consciousness level
- Kidney function (urine output)
- Abdomen (uterine tone, tenderness)
- Source of bleeding or infection
- Systems affected (multiple organ assessment)
- Embryo/fetus status
- Serial labs and trends
- Significant comorbidities
9.2 Nursing Diagnosis
Based on the comprehensive assessment data, several nursing diagnoses are applicable to patients with obstetrical shock. These diagnoses guide the development of the nursing care plan and interventions.
