Shoulder Dystocia: Comprehensive Guide for Nursing Students
A detailed resource for identification, prevention, and management of shoulder dystocia in obstetric practice
Table of Contents
- 1. Definition and Overview
- 2. Incidence and Significance
- 3. Relevant Anatomy
- 4. Risk Factors
- 5. Identification and Diagnosis
- 6. Prevention Strategies
- 7. Management Techniques
- 8. Complications
- 9. Nursing Role and Responsibilities
- 10. Documentation Requirements
- 11. Case Scenarios
- 12. Summary and Key Points
- 13. References
1. Definition and Overview
Shoulder dystocia is an obstetric emergency that occurs when the anterior fetal shoulder becomes impacted against the maternal symphysis pubis after the delivery of the fetal head, preventing the completion of the birth with standard obstetric maneuvers. This complication requires prompt identification and management to prevent maternal and fetal morbidity and mortality.
Shoulder dystocia represents one of the most challenging and anxiety-provoking emergencies in obstetric practice. It is largely unpredictable, can occur without warning, and requires immediate coordinated intervention from the entire healthcare team.
Important Note:
Despite being frequently associated with macrosomia (large fetal size), approximately half of all shoulder dystocia cases occur in babies of normal weight. This underscores the importance of preparation and readiness to manage this emergency in all deliveries, not just those with identified risk factors.
2. Incidence and Significance
The incidence of shoulder dystocia varies depending on the population studied and the diagnostic criteria used, but generally ranges from 0.2% to 3% of all vaginal deliveries. The variation in reported incidence reflects the subjective nature of its diagnosis and documentation.
Clinical Significance
Shoulder dystocia is significant because of its association with increased maternal and fetal morbidity. It can lead to severe complications including brachial plexus injuries, fractures, hypoxic injury, and even fetal death. For the mother, it can result in postpartum hemorrhage, genital tract lacerations, and psychological trauma.
3. Relevant Anatomy
Understanding the pelvic and fetal anatomy is crucial for comprehending the mechanism of shoulder dystocia and its management.
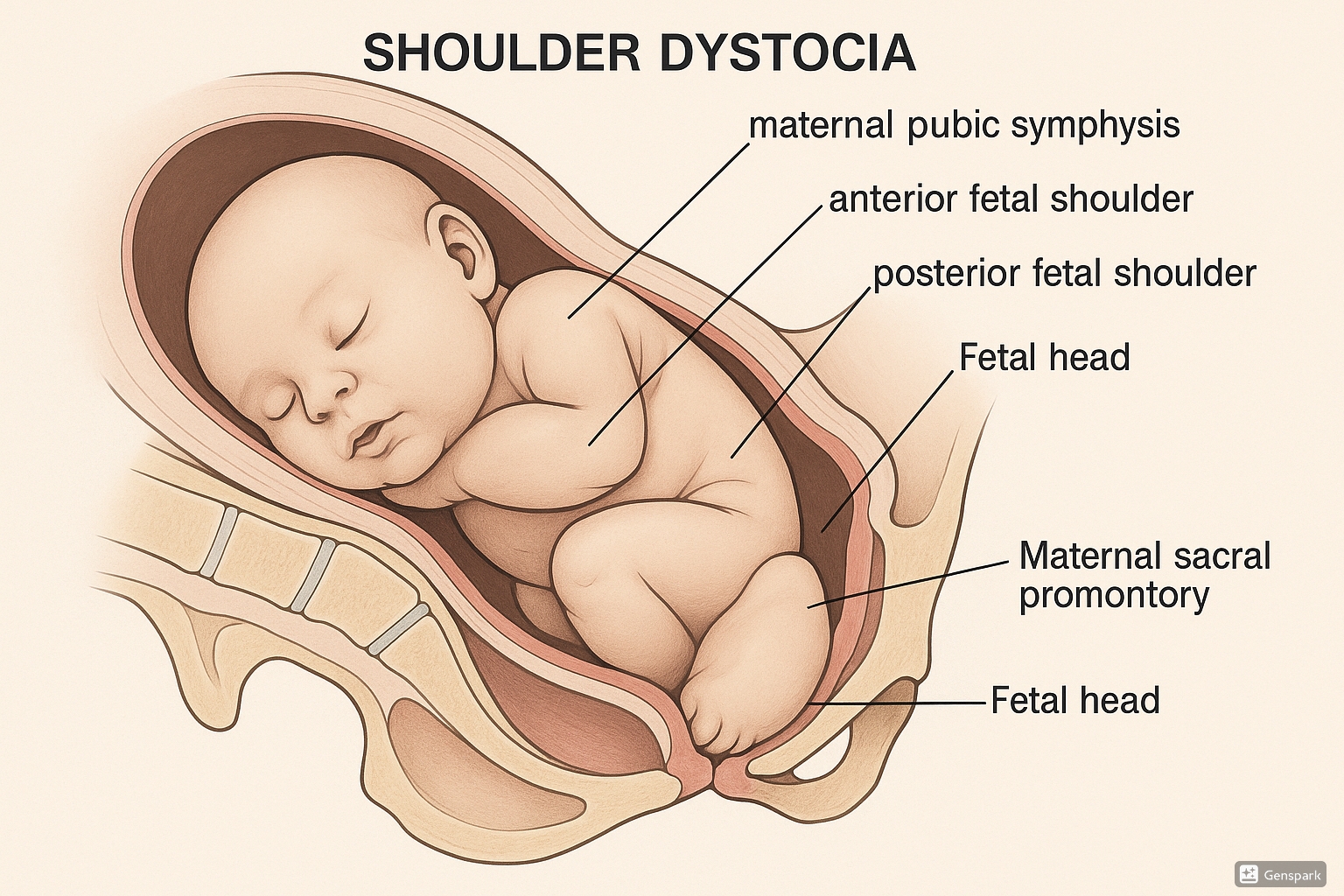
Figure 1: Anatomical illustration of shoulder dystocia showing impaction of the anterior fetal shoulder against the maternal pubic symphysis with the “turtle sign” visible.
Key Anatomical Considerations:
- Pelvic Diameters: The anteroposterior diameter of the pelvic inlet is typically the most critical dimension in shoulder dystocia.
- Pubic Symphysis: The anterior fetal shoulder frequently becomes impacted behind this structure.
- Sacral Promontory: The posterior fetal shoulder may become impacted against this structure in severe cases.
- Bony Pelvis vs. Soft Tissue: Both bony and soft tissue resistance can contribute to shoulder dystocia.
- Fetal Shoulders: The bisacromial diameter (shoulder width) is critical in determining the risk of shoulder dystocia.
4. Risk Factors
While shoulder dystocia can occur unexpectedly in women with no risk factors, several conditions have been associated with an increased risk:
| Category | Risk Factors | Level of Association |
|---|---|---|
| Maternal Factors |
• Diabetes mellitus • Obesity (BMI > 30) • Advanced maternal age • Post-term pregnancy • Excessive weight gain during pregnancy |
Strong |
| Fetal Factors |
• Macrosomia (birth weight > 4000g) • Prior macrosomic infant • Male fetal gender |
Strong |
| Obstetric History |
• Previous shoulder dystocia • Previous difficult delivery |
Strong |
| Labor & Delivery Factors |
• Prolonged second stage of labor • Instrumental delivery (especially vacuum extraction) • Oxytocin augmentation • Epidural analgesia |
Moderate |
| Pelvic Factors |
• Contracted pelvis • Pelvic abnormalities |
Moderate |
Important Consideration:
Despite these identified risk factors, approximately 50% of shoulder dystocia cases occur in the absence of any identifiable risk factors. Therefore, all delivery personnel should be prepared to manage this emergency in any vaginal delivery.
5. Identification and Diagnosis
Early recognition of shoulder dystocia is crucial for prompt management and improved outcomes.
5.1 Signs and Symptoms
Primary Signs of Shoulder Dystocia:
- Failure of delivery of the shoulders with gentle downward traction
- The “turtle sign” – retraction of the fetal head against the maternal perineum
- Failure of restitution of the fetal head
- Failure of the fetal shoulders to descend
5.2 The Turtle Sign
The “turtle sign” is a classic clinical indicator of shoulder dystocia. It refers to the retraction of the fetal head back toward the maternal perineum after it has been delivered, resembling a turtle retracting its head into its shell.
Recognizing the Turtle Sign:
- The newborn’s head appears to be pulled back against the perineum
- The chin may be pressed tightly against the perineum
- There is difficulty delivering the shoulders with gentle traction
- The head may appear congested due to compression of venous return
Note: The presence of the turtle sign should prompt immediate action and implementation of shoulder dystocia management protocols.
6. Prevention Strategies
While shoulder dystocia cannot always be prevented, certain strategies may reduce its incidence or severity:
Antepartum Strategies
- Careful management of gestational diabetes
- Monitoring fetal growth with ultrasound in high-risk pregnancies
- Consider elective cesarean delivery for estimated fetal weight > 5000g in diabetic mothers or > 5500g in non-diabetic mothers
- Appropriate maternal weight gain counseling
Intrapartum Strategies
- Avoid operative vaginal delivery when macrosomia is suspected
- Consider alternative maternal positions during delivery
- Careful use of oxytocin in high-risk patients
- Recognize warning signs of potential shoulder dystocia
Nursing Prevention Role:
As a nurse, you play a crucial role in the prevention of shoulder dystocia complications through:
- Thorough assessment and documentation of risk factors during antepartum care
- Patient education regarding modifiable risk factors
- Vigilant intrapartum monitoring for warning signs
- Ensuring emergency equipment is readily available
- Regular participation in simulation drills for shoulder dystocia management
7. Management Techniques
The management of shoulder dystocia requires a coordinated, systematic approach to maximize successful outcomes and minimize complications.
7.1 HELPERR Mnemonic
The HELPERR mnemonic, developed by the Advanced Life Support in Obstetrics (ALSO) program, provides a structured approach to managing shoulder dystocia:
HELPERR Mnemonic for Shoulder Dystocia Management
Call for additional help immediately, including primary obstetric provider, additional nursing staff, anesthesia, and pediatrics/neonatology. Assign clear roles to team members.
Consider performing an episiotomy if more room is needed for internal maneuvers, though this alone will not resolve shoulder dystocia as it is a bony obstruction issue.
Position the mother with thighs flexed against her abdomen, removing the sacral promontory as an obstruction and straightening the pelvic curve to help dislodge the anterior shoulder.
Apply firm, continuous suprapubic pressure directed obliquely from the fetal back toward the anterior shoulder. This can help dislodge the anterior shoulder from behind the symphysis pubis.
Internal maneuvers to rotate the shoulders into an oblique diameter of the pelvis:
- Rubin’s maneuver: Pressure on the posterior aspect of the anterior shoulder toward the fetal chest
- Wood’s screw maneuver: Rotation of the posterior shoulder progressively 180 degrees
Insertion of hand to locate the posterior arm, flex at the elbow, and sweep the arm across the chest and deliver it, effectively reducing the bisacromial diameter.
Turn the mother onto hands and knees (all-fours or Gaskin position), which may help dislodge the impacted shoulder by changing the pelvic dimensions and utilizing gravity.
Time is Critical!
Shoulder dystocia is a time-sensitive emergency. Each maneuver should be attempted for approximately 30-60 seconds before progressing to the next one if unsuccessful. The nurse should announce the elapsed time at regular intervals.
7.2 McRoberts Maneuver
The McRoberts maneuver is often the first intervention for managing shoulder dystocia and has been shown to be effective in resolving approximately 40-60% of cases when used alone or in combination with suprapubic pressure.
Proper Technique for McRoberts Maneuver:
- Remove any pillows from beneath the mother’s head and back
- Position the mother flat on her back
- Flex both thighs sharply onto the maternal abdomen (knees to chest)
- This movement helps to straighten the sacrum relative to the lumbar spine and rotates the symphysis pubis toward the maternal head
- The flattening of the lumbar lordosis may help dislodge the impacted shoulder
Nursing Role in McRoberts Maneuver:
Nurses typically assist with positioning the mother’s legs for the McRoberts maneuver. The legs should be hyperflexed at both the hip and knee joints and pulled toward the shoulders. It is important to provide clear instructions to the mother and adequate support for her legs.
7.3 Other Management Maneuvers
If the McRoberts maneuver and suprapubic pressure are unsuccessful, additional maneuvers may be required:
| Maneuver | Technique | Considerations |
|---|---|---|
| Rubin’s Maneuver | Pressure on the posterior aspect of the anterior shoulder, pushing toward the fetal chest | Aims to adduct the shoulders and reduce the bisacromial diameter |
| Wood’s Screw Maneuver | Applying pressure against the anterior surface of the posterior shoulder to rotate it clockwise | Works like a corkscrew to rotate the shoulders into the oblique diameter of the pelvis |
| Delivery of Posterior Arm | Inserting hand into vagina to identify and deliver the posterior arm of the fetus | Reduces shoulder diameter by removing one arm from the equation; requires adequate room and careful technique |
| Gaskin Maneuver (All-Fours) | Positioning mother on hands and knees | Changes pelvic dimensions and may facilitate delivery; can be difficult to achieve quickly or with epidural anesthesia |
| Zavanelli Maneuver | Cephalic replacement (pushing the head back in) followed by cesarean delivery | Last resort for intractable shoulder dystocia; associated with significant complications |
8. Complications
Shoulder dystocia can lead to significant complications for both mother and baby if not managed promptly and effectively.
8.1 Maternal Complications
Immediate Complications
- Postpartum hemorrhage (10-40%)
- Third or fourth-degree perineal lacerations
- Vaginal and cervical lacerations
- Uterine rupture (rare)
- Bladder injury
- Symphyseal separation or diastasis
Long-term Complications
- Pelvic floor disorders
- Rectovaginal fistula
- Psychological trauma
- Fear of future childbirth
- Post-traumatic stress disorder
8.2 Fetal Complications
Physical Injuries
- Brachial plexus injury (2-16%)
- Erb’s palsy (C5-C6)
- Klumpke’s palsy (C8-T1)
- Complete brachial plexus injury
- Clavicular fracture
- Humeral fracture
- Facial nerve injury
Neurological Complications
- Hypoxic-ischemic encephalopathy
- Cerebral palsy
- Permanent neurological damage
- Fetal death (0-2%)
Brachial Plexus Injuries – The “SNAPPED” Mnemonic
To remember the key features of brachial plexus injuries:
- S – Sensory changes in the affected limb
- N – Nerves of C5-T1 potentially affected
- A – Asymmetrical Moro reflex
- P – Position of affected limb (internal rotation, adduction)
- P – Paralysis or weakness present
- E – Erb’s palsy vs. total plexus injury
- D – Documentation of injury essential
9. Nursing Role and Responsibilities
Nurses play a crucial role in the identification, management, and documentation of shoulder dystocia. Their responsibilities span from prevention to post-delivery care.
9.1 Before Delivery
Preventive and Preparatory Role:
- Identify and document risk factors for shoulder dystocia
- Communicate risk factors to the healthcare team
- Ensure emergency equipment is readily available
- Position equipment for easy access in an emergency
- Know facility protocols for managing shoulder dystocia
- Participate in regular simulation drills
9.2 During Shoulder Dystocia
Immediate Nursing Actions:
- Recognize and announce the emergency: “We have a shoulder dystocia!”
- Activate appropriate response team: Call for additional help
- Begin timing the event: Document start time of shoulder dystocia
- Assist with maternal positioning: Help implement McRoberts maneuver
- Apply suprapubic pressure: When directed and using proper technique
- Monitor vital signs: Maintain awareness of maternal and fetal status
- Provide support to the mother: Clear communication and reassurance
- Announce elapsed time: Keep team aware of duration (e.g., “One minute since shoulder dystocia identified”)
- Document maneuvers: Note sequence and timing of interventions
- Prepare for neonatal resuscitation: Alert pediatric team if not already present
9.3 After Resolution
Post-Delivery Nursing Responsibilities:
- Monitor for postpartum hemorrhage and other maternal complications
- Assess newborn for injuries related to shoulder dystocia
- Document the event thoroughly, including:
- Time of head delivery
- Time shoulder dystocia was identified
- Sequence of maneuvers performed and their timing
- Time of complete delivery
- Total duration of shoulder dystocia
- Staff members present and their roles
- Provide emotional support to the mother and family
- Facilitate debriefing with the healthcare team
- Participate in case review for quality improvement
10. Documentation Requirements
Proper documentation of shoulder dystocia cases is essential for continuity of care, risk management, and quality improvement.
Essential Elements of Shoulder Dystocia Documentation:
- Timing:
- Time of delivery of fetal head
- Time shoulder dystocia was identified
- Time of delivery of body
- Duration of shoulder dystocia
- Maneuvers:
- Specific maneuvers used in sequential order
- Duration of each maneuver
- Healthcare provider performing each maneuver
- Response to each maneuver
- Team Response:
- Personnel present during the event
- Time additional help was called
- Roles assigned to team members
- Maternal Assessment:
- Pre-existing risk factors
- Vital signs before, during, and after the event
- Maternal injuries or complications
- Estimated blood loss
- Neonatal Assessment:
- Apgar scores
- Cord blood gases (if obtained)
- Evidence of trauma or injury
- Need for resuscitation
- Initial examination findings
Legal Considerations:
Shoulder dystocia events are frequently involved in obstetric litigation. Thorough, objective, and accurate documentation is your best defense. Avoid subjective statements or blame in the medical record. Document facts, not opinions.
11. Case Scenarios
The following case scenarios illustrate different presentations and management approaches for shoulder dystocia.
Case Scenario 1: Anticipated Shoulder Dystocia
Patient Profile: 35-year-old G2P1, BMI 33, gestational diabetes, estimated fetal weight 4500g
Scenario: Patient has progressed to complete dilation after induction of labor at 39 weeks. Given her multiple risk factors, the team anticipates possible shoulder dystocia.
Nursing Actions:
- Alert the primary provider and charge nurse about high-risk delivery
- Ensure pediatric team is available
- Verify emergency equipment is accessible
- Review shoulder dystocia protocol with team
- Document risk factors and preparations
Outcome:
Shoulder dystocia occurs during delivery but is quickly resolved with McRoberts maneuver and suprapubic pressure. Baby is delivered without injury. Prompt recognition and preparation were key factors in successful management.
Case Scenario 2: Unexpected Shoulder Dystocia
Patient Profile: 28-year-old G1P0, no significant risk factors, estimated fetal weight 3700g
Scenario: Patient has had an uncomplicated labor. After delivery of the fetal head, the turtle sign is observed, and standard traction fails to deliver the shoulders.
Nursing Actions:
- Immediately announce “shoulder dystocia” to alert team
- Call for additional help
- Begin timing the event
- Assist with McRoberts positioning
- Apply suprapubic pressure as directed
- Continue to announce elapsed time
- Document sequence of events and maneuvers
Outcome:
Initial maneuvers are unsuccessful. Wood’s screw maneuver is performed followed by delivery of the posterior arm, resulting in successful delivery after 3 minutes of shoulder dystocia. The newborn has Apgar scores of 6 and 8, with suspected Erb’s palsy requiring follow-up. This case highlights the importance of being prepared for shoulder dystocia in all deliveries, even without risk factors.
12. Summary and Key Points
Essential Takeaways for Nursing Students:
- Shoulder dystocia is an unpredictable obstetric emergency requiring immediate coordinated response
- Early recognition of the “turtle sign” and failure of the shoulders to deliver with gentle traction are diagnostic
- The HELPERR mnemonic provides a systematic approach to management
- McRoberts maneuver and suprapubic pressure are first-line interventions
- Multiple maneuvers may be required, proceeding in a logical sequence
- Time is critical – maneuvers should be attempted for 30-60 seconds before progressing
- The nurse’s role includes recognition, team activation, timing, assistance with maneuvers, and thorough documentation
- Prompt and proper management reduces the risk of maternal and neonatal complications
- Detailed documentation is essential for continuity of care and risk management
- Regular simulation drills improve team readiness for this emergency
Remember This
“In shoulder dystocia, think CALMLY but ACT QUICKLY. Every second counts, but panic only costs more time.”
13. References
- Hill, D. A., Lense, J., & Roepcke, F. (2020). Shoulder Dystocia: Managing an Obstetric Emergency. American Family Physician, 102(2), 84-90.
- Politi, S., D’Emidio, L., Cignini, P., & Giorlandino, C. (2010). Shoulder dystocia: an Evidence-Based approach. Journal of prenatal medicine, 4(3), 35-42.
- McArdle, J., Sorensen, A., Fowler, C. I., Sommerness, S., Burson, K., & Kahwati, L. (2018). Strategies to improve management of shoulder dystocia under the AHRQ Safety Program for Perinatal Care. Journal of obstetric, gynecologic, and neonatal nursing, 47(2), 191-201.
- Roth, C. K., Parfitt, S. E., Hering, S. L., & Dent, S. A. (2014). Developing protocols for obstetric emergencies. Nursing for Women’s Health, 18(5), 379-390.
- Curtis, K., & Guillien, L. (2009). Shoulder dystocia drills: how one unit prepares for potential obstetric emergencies. Nursing for Women’s Health, 13(1), 54-63.
- Royal College of Obstetricians and Gynaecologists. (2017). Shoulder Dystocia (Green-top Guideline No. 42). RCOG.
- American College of Obstetricians and Gynecologists. (2017). Practice Bulletin No. 178: Shoulder Dystocia. Obstetrics and Gynecology, 129(5), e123-e133.
- Crofts, J. F., Lenguerrand, E., Bentham, G. L., Tawfik, S., Claireaux, H. A., Odd, D., Fox, R., & Draycott, T. J. (2016). Prevention of brachial plexus injury-12 years of shoulder dystocia training: an interrupted time-series study. BJOG: An International Journal of Obstetrics & Gynaecology, 123(1), 111-118.
- Gurewitsch Allen, E. D. (2018). Shoulder Dystocia: Incidence and Risk Factors. Clinical Obstetrics and Gynecology, 61(1), 210-218.
- Baxley, E. G., & Gobbo, R. W. (2004). Shoulder dystocia. American Family Physician, 69(7), 1707-1714.
