Recognition and Management of Postnatal Urinary Complications
“Understanding postnatal urinary complications is essential for providing holistic nursing care to new mothers and promoting optimal recovery following childbirth.”
Introduction
Postnatal urinary complications are common yet often overlooked conditions affecting women after childbirth. These complications can significantly impact a mother’s recovery, comfort, and overall well-being during the postpartum period. As nursing professionals, understanding the recognition, assessment, and management of these complications is crucial for providing comprehensive care and preventing long-term consequences.
The postpartum period represents a time of significant physiological adjustment for new mothers. Hormonal fluctuations, physical trauma during delivery, and changes in the pelvic floor structure all contribute to potential urinary system dysfunction. Studies indicate that up to 20-30% of women experience some form of postnatal urinary complication, with higher rates observed following instrumental deliveries and cesarean sections.
This educational resource aims to provide nursing students with comprehensive knowledge about postnatal urinary complications, their assessment, management, and prevention. By mastering this content, nurses will be equipped to identify potential issues early, implement appropriate interventions, and educate patients effectively, ultimately improving maternal health outcomes and quality of life during the postpartum period.
Anatomy and Physiology of the Postpartum Urinary System
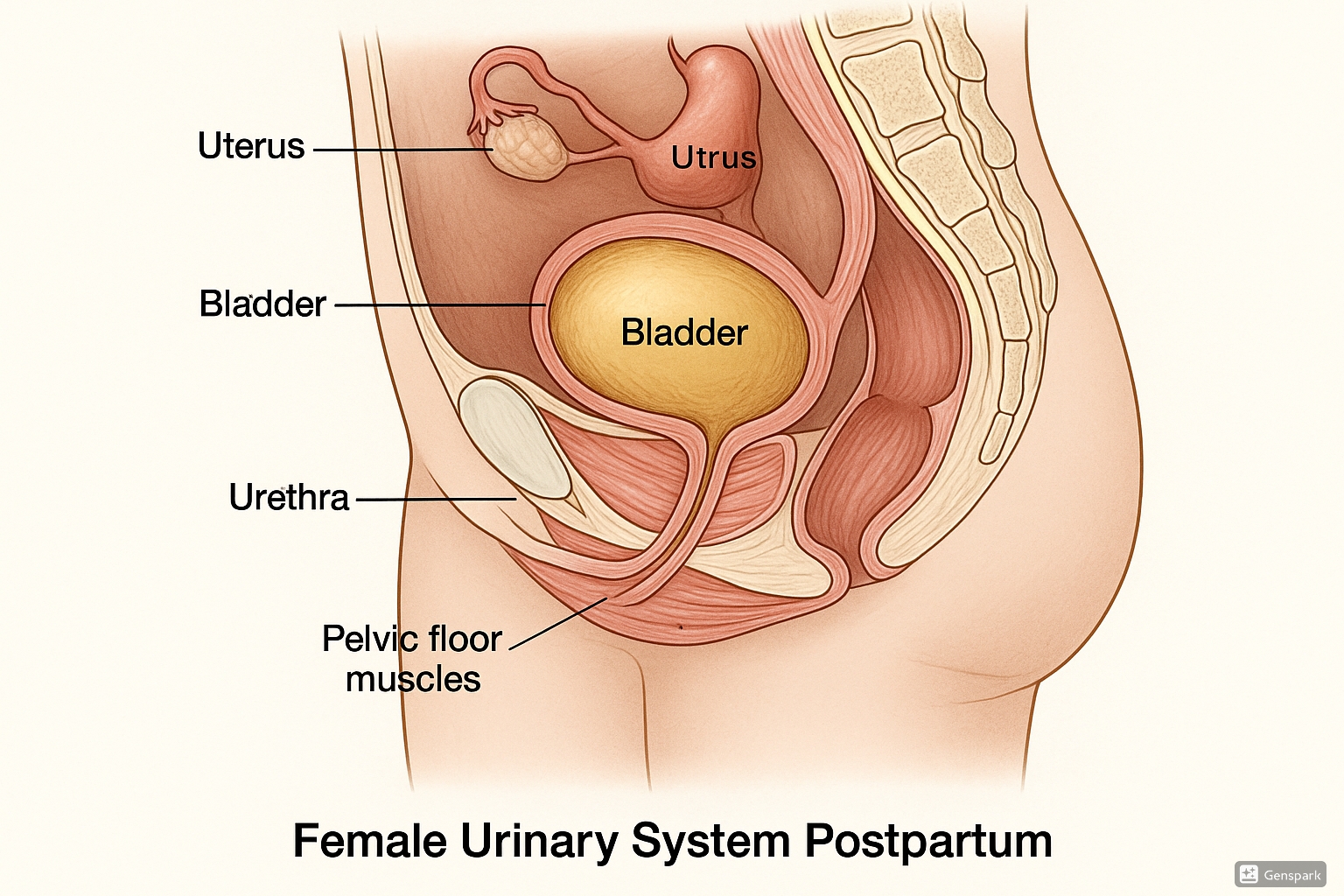
Fig 1. Female urinary system postpartum showing bladder, urethra and pelvic floor muscles
To understand postnatal urinary complications, it’s essential to appreciate the anatomical and physiological changes that occur in the urinary system during pregnancy and the postpartum period:
Physiological Changes During Pregnancy
- Increased renal blood flow and glomerular filtration rate (40-50% higher)
- Bladder capacity increases from 500ml to approximately 1000ml
- Hormonal changes (progesterone) cause relaxation of smooth muscle in the urinary tract
- Mechanical pressure from the enlarging uterus causes:
- Displacement and compression of the bladder
- Urethral elongation
- Increased intravesical pressure
Postpartum Physiological Readjustments
- Rapid diuresis within 12-24 hours after delivery
- Gradual return of bladder position as the uterus involutes
- Recovery of bladder sensation and tone can be delayed
- Pelvic floor muscles may be weakened or damaged during vaginal delivery
- Neural pathways controlling micturition can be temporarily disrupted
Key Point
The physiological changes of pregnancy don’t immediately reverse after delivery. The bladder continues to experience decreased sensation and altered function for several days postpartum, predisposing women to complications like urinary retention and overflow incontinence.
Urinary Control Mechanisms
Normal urination involves a complex interplay between the central nervous system, autonomic nervous system, and the musculature of the bladder and urethra:
Neural Control
- Parasympathetic stimulation (S2-S4) – detrusor contraction
- Sympathetic inhibition (T10-L2) – bladder relaxation
- Somatic control (pudendal nerve) – external sphincter
Muscular Components
- Detrusor muscle – smooth muscle of bladder wall
- Internal urethral sphincter – involuntary control
- External urethral sphincter – voluntary control
- Pelvic floor muscles – support and additional control
Following delivery, these control mechanisms can be affected by several factors:
- Regional anesthesia (epidural) temporarily blocks nerve pathways
- Physical trauma can damage nerve endings
- Edema can compress neural pathways
- Pain and perineal discomfort can inhibit voluntary voiding
- Postpartum medications may affect bladder function
Types of Postnatal Urinary Complications
Understanding the different types of postnatal urinary complications is essential for effective assessment and management. These complications can be broadly categorized into three main types:
1. Urinary Retention
Postnatal urinary retention (PUR) is defined as the inability to void spontaneously within 6 hours after vaginal delivery or within 6 hours after removal of an indwelling catheter following cesarean section. It is one of the most common postnatal urinary complications, affecting approximately 3-10% of women after childbirth.
Types of Postnatal Urinary Retention:
Overt Retention
Complete inability to void despite having the urge to urinate. The woman feels discomfort but cannot initiate or maintain urine flow.
Covert Retention
Incomplete emptying of the bladder without symptoms. The woman voids but retains significant post-void residual volume (>150ml).
Persistent Retention
Continuing difficulty emptying the bladder beyond 3 days postpartum, which may indicate a more severe underlying condition.
Risk Factors for Postnatal Urinary Retention:
Delivery-Related Factors
- Prolonged labor (>24 hours)
- Instrumental delivery (forceps/vacuum)
- Episiotomy or extensive perineal tears
- Macrosomic infant (>4000g)
- Epidural anesthesia
- Cesarean section
Pre-existing Factors
- Primiparity (first childbirth)
- History of urinary retention
- Pre-existing neurological conditions
- Previous pelvic surgery
- Age >35 years
Clinical Manifestations:
- Inability to void despite feeling the urge
- Suprapubic discomfort or pain
- Palpable or percussible bladder
- Frequent small voids (<150ml)
- Sense of incomplete emptying
- Overflow incontinence (in severe cases)
Potential Complications of Untreated Urinary Retention
- Bladder overdistension and detrusor damage
- Urinary tract infections due to stagnant urine
- Development of overflow incontinence
- Long-term voiding dysfunction
- Hydronephrosis (in severe cases)
2. Urinary Incontinence
Postnatal urinary incontinence refers to the involuntary leakage of urine after childbirth. It affects approximately 33% of women in the immediate postpartum period, with rates declining but remaining significant at 3 months (15-20%) and 12 months (6-10%) postpartum.
Types of Postnatal Urinary Incontinence:
Stress Incontinence
Leakage of urine during activities that increase intra-abdominal pressure, such as coughing, laughing, sneezing, or physical exertion. Most common form in the postpartum period due to weakened pelvic floor muscles.
Urge Incontinence
Involuntary leakage accompanied by or immediately preceded by urgency (sudden compelling desire to pass urine). Associated with detrusor muscle overactivity.
Mixed Incontinence
Combination of both stress and urge incontinence symptoms. Common in postpartum women, especially those with previous deliveries.
Overflow Incontinence
Leakage due to bladder overdistension, often secondary to urinary retention. Presents as constant dribbling or frequent small voids.
Risk Factors for Postnatal Urinary Incontinence:
Obstetric Factors
- Vaginal delivery (especially instrumental)
- Prolonged second stage of labor
- Perineal trauma (3rd or 4th-degree tears)
- High birth weight baby
- Multiple vaginal deliveries
Maternal Factors
- Pre-pregnancy incontinence
- Obesity (BMI >30)
- Advanced maternal age
- Chronic constipation
- Family history of incontinence
- Connective tissue disorders
Important Note
While urinary incontinence is common in the early postpartum period, persistence beyond 3 months should prompt further evaluation and intervention to prevent long-term complications.
3. Urinary Tract Infections
Urinary tract infections (UTIs) are another common postnatal urinary complication, affecting approximately 2-4% of women after childbirth. The risk is higher in women who had catheterization during labor or postpartum, and in those with urinary retention.
Types of Postnatal UTIs:
| Type | Description | Common Symptoms |
|---|---|---|
| Cystitis | Infection of the bladder, most common form | Dysuria, frequency, urgency, suprapubic pain, cloudy or foul-smelling urine |
| Pyelonephritis | Infection of the kidneys, more serious | Flank pain, fever, chills, nausea/vomiting, costovertebral angle tenderness |
| Urethritis | Infection of the urethra | Dysuria, urethral discharge, meatal irritation |
| Asymptomatic Bacteriuria | Presence of bacteria in urine without symptoms | None – detected on routine screening |
Risk Factors for Postnatal UTIs:
- Catheterization during labor or postpartum period
- Urinary retention
- History of UTIs
- Operative delivery
- Diabetes mellitus
- Immunosuppression
- Poor perineal hygiene
- Dehydration
Causative Organisms:
The most common pathogens causing postnatal UTIs include:
- Escherichia coli (80-90%)
- Klebsiella pneumoniae
- Proteus mirabilis
- Staphylococcus saprophyticus
- Enterococcus species
Warning
Untreated UTIs in the postpartum period can progress to pyelonephritis and sepsis. Early detection and treatment are essential to prevent serious complications.
Assessment and Diagnosis of Postnatal Urinary Complications
Thorough assessment is crucial for the early identification and appropriate management of postnatal urinary complications. A comprehensive approach should include:
Clinical History
Obtaining a detailed history is the first step in assessment:
Obstetric History
- Mode of delivery (vaginal, instrumental, cesarean)
- Duration of labor, especially second stage
- Birth weight of the baby
- Perineal trauma (episiotomy, lacerations)
- Anesthesia used during delivery (epidural, spinal)
Urinary History
- Time since last void
- Volume and frequency of voids
- Difficulties initiating or maintaining urine stream
- Sensations of incomplete emptying
- Presence of urinary incontinence
- Dysuria, urgency, or frequency
- Previous urinary problems (before or during pregnancy)
Medication History
- Current analgesics, which may affect sensation
- Other medications affecting bladder function
Physical Examination
Physical examination should focus on assessing for signs of urinary complications:
Abdominal Assessment
- Inspection for lower abdominal distension
- Palpation for suprapubic tenderness or bladder distension
- Percussion to assess bladder fullness
Perineal Assessment
- Inspection for perineal trauma, edema, or hematoma
- Assessment of perineal pain
- Evaluation of perineal hygiene
Diagnostic Tools and Assessments
Bladder Diary
A bladder diary is a valuable tool for assessing urinary patterns and identifying problems:
- Records time and volume of each void
- Documents fluid intake
- Notes episodes of incontinence and associated activities
- Captures urgency and other symptoms
- Typically maintained for 3-7 days
Laboratory Tests
| Test | Purpose | Findings in Complications |
|---|---|---|
| Urinalysis | Screening for infection, hematuria | Presence of leukocytes, nitrites, blood, protein |
| Urine Culture | Identify causative organisms in UTI | ≥10^5 CFU/ml indicates significant bacteriuria |
| Creatinine Clearance | Assess kidney function | Decreased in case of renal involvement |
Post-Void Residual (PVR) Assessment
Measuring the volume of urine remaining in the bladder after voiding is critical for diagnosing urinary retention:
Ultrasound Bladder Scanning
- Non-invasive method
- Provides immediate results
- Accuracy within 10-15% of actual volume
- Can be performed by trained nursing staff
Catheterization
- Most accurate method
- More invasive with infection risk
- Can be therapeutic as well as diagnostic
Interpretation of PVR Results
- Normal: <50ml
- Borderline: 50-150ml – requires monitoring
- Significant retention: >150ml – requires intervention
- Severe retention: >400ml – urgent intervention needed
Advanced Diagnostic Tests
For persistent or complex cases, additional investigations may be required:
- Urodynamic Studies: Evaluates bladder function, capacity, and compliance
- Cystoscopy: Direct visualization of bladder and urethra
- Renal Ultrasound: To assess for upper urinary tract complications
Common Nursing Diagnoses for Postnatal Urinary Complications
| NANDA Diagnosis | Related To | As Evidenced By |
|---|---|---|
| Impaired Urinary Elimination | Mechanical trauma during delivery, effects of anesthesia, edema | Frequency, urgency, hesitancy, retention, dysuria |
| Urinary Retention | Decreased sensation, inhibition due to pain, high sphincter pressure | Bladder distension, small frequent voiding, inability to empty bladder |
| Stress Urinary Incontinence | Weakened pelvic floor muscles, tissue trauma | Leakage with increased abdominal pressure (coughing, laughing) |
| Urge Urinary Incontinence | Detrusor overactivity, bladder irritation | Inability to reach toilet in time, urgency |
| Risk for Infection | Urinary stasis, catheterization, perineal trauma | Presence of risk factors |
| Deficient Knowledge | Lack of exposure to information about postnatal urinary care | Questions, misconceptions, improper techniques |
Management Approaches for Postnatal Urinary Complications
Effective management of postnatal urinary complications requires a comprehensive approach tailored to the specific condition and its severity. Early intervention is crucial to prevent long-term consequences.
Management of Urinary Retention
The approach to managing postnatal urinary retention follows a stepwise protocol:
Conservative Measures
- Early mobilization after delivery
- Privacy and comfortable position during voiding
- Running water sound (tap water)
- Warm water over perineum
- Warm shower or bath
- Adequate analgesia for perineal pain
- Pouring warm water over vulva during voiding attempts
- Double voiding technique (void, wait a few minutes, then void again)
Catheterization
If conservative measures fail or if the bladder is significantly distended:
Intermittent Catheterization
- Preferred initial approach
- Lower risk of UTI than indwelling catheter
- Allows normal bladder filling/emptying cycle
- Frequency based on PVR volumes:
- PVR 150-300ml: every 4-6 hours
- PVR >300ml: every 3-4 hours
- Continue until 2 consecutive PVRs <150ml
Indwelling Catheterization
- Used for severe retention or when intermittent catheterization is not feasible
- Typically inserted for 24-48 hours
- Trial without catheter (TWOC) protocol:
- Remove catheter (preferably in morning)
- Encourage normal voiding
- Measure PVR after first void
- Reinsert if PVR remains >150ml
Pharmacological Intervention
Medications may be considered in selected cases:
- Parasympathomimetics: Bethanechol (Urecholine) – stimulates detrusor contraction
- Alpha-adrenergic blockers: Tamsulosin – reduces urethral resistance
- Note: Limited evidence supports routine use in postpartum period
Follow-up and Referral
For persistent urinary retention beyond 3-5 days:
- Referral to urology or urogynecology
- Further urodynamic studies
- Evaluation for neurological complications
- Long-term management plan may include clean intermittent self-catheterization (CISC)
Bladder Retraining Protocol
For women with persistent difficulties, a structured bladder retraining program may be beneficial:
- Scheduled voiding every 2-3 hours during waking hours
- Gradually increasing intervals between voids
- Double voiding technique at each attempt
- PVR monitoring to track progress
- Maintain adequate hydration but avoid excessive fluid intake
Management of Urinary Incontinence
Management strategies for postpartum urinary incontinence focus on strengthening pelvic floor muscles and modifying contributing factors:
Pelvic Floor Muscle Training (PFMT)
- First-line intervention for all types of urinary incontinence
- Should be initiated as soon as comfortable after delivery
- Proper technique instruction is essential
- Daily exercises for at least 3 months
- May be combined with biofeedback for better results
Behavioral Modifications
- Timed voiding schedule
- Bladder training to increase capacity
- Weight management for overweight women
- Fluid management (adequate hydration without excess)
- Avoidance of bladder irritants (caffeine, alcohol, acidic foods)
- Constipation management
Pharmacological Treatment
Medications are typically a second-line treatment if conservative measures fail:
- Anticholinergics: For urge incontinence (oxybutynin, solifenacin)
- Beta-3 adrenergic agonists: Mirabegron for overactive bladder
- Note: Consider breastfeeding status when prescribing
Supportive Devices
- Vaginal Pessaries: For stress incontinence with pelvic organ prolapse
- Vaginal Cones: Weighted devices to strengthen pelvic floor
- Absorbent Products: For symptom management during recovery
Additional Therapies
- Electrical Stimulation: For women unable to contract pelvic floor muscles
- Percutaneous Tibial Nerve Stimulation (PTNS): For urge incontinence
Referral Criteria
Consider referral to a urogynecologist, women’s health physiotherapist, or continence nurse specialist if:
- Incontinence persists beyond 3 months postpartum
- Symptoms significantly impact quality of life
- Associated pelvic organ prolapse is present
- Conservative measures have been unsuccessful
Management of Urinary Tract Infections
Prompt recognition and treatment of UTIs is essential to prevent ascending infection and complications:
Diagnostic Evaluation
- Midstream urine sample for culture and sensitivity
- Urinalysis for leukocyte esterase and nitrites
- Assessment of systemic symptoms
Antibiotic Treatment
Treatment selection should consider:
- Local antibiotic resistance patterns
- Breastfeeding status
- Severity of infection
- Common first-line agents include:
- Nitrofurantoin (safe during breastfeeding)
- Cephalexin
- Amoxicillin-clavulanate
- Duration typically 3-7 days for uncomplicated cystitis
Supportive Measures
- Increased fluid intake (2-3 liters daily)
- Cranberry products (modest preventive effect)
- Adequate analgesia for pain relief
- Warm sitz baths for perineal discomfort
Warning Signs Requiring Urgent Attention
Refer for immediate medical assessment if any of these symptoms develop:
- High fever (>38.5°C/101.3°F)
- Severe flank pain
- Persistent vomiting
- Signs of sepsis (tachycardia, hypotension)
- Inability to take oral medications
Management of Catheter Care in Postpartum Period
Proper management of urinary catheters is essential to prevent complications:
Indwelling Catheter Care
- Maintain closed drainage system
- Secure catheter to prevent movement and traction
- Position drainage bag below level of bladder
- Perform routine perineal care twice daily and after bowel movements
- Monitor urine output, color, and clarity
- Maintain adequate hydration
Catheter Removal Protocol
- Remove catheter in morning (allows monitoring throughout day)
- Encourage oral fluids
- Request patient to void within 4-6 hours
- Record time and volume of first void
- Perform bladder scan or catheterization to measure PVR volume
- Further action based on PVR measurement:
- PVR <150ml: continue normal voiding
- PVR 150-300ml: recheck after next void
- PVR >300ml: recatheterize or start intermittent catheterization
Documentation
Maintain comprehensive documentation including:
- Reason for catheterization
- Type and size of catheter
- Date and time of insertion
- Urine output and characteristics
- Patient response and comfort level
- Removal date and time
- Post-removal voiding pattern and volumes
- PVR measurements
Pharmacological Interventions for Postnatal Urinary Complications
Medications play an important but selective role in managing postnatal urinary complications. Consideration must be given to the safety of these medications during breastfeeding.
Medications for Urinary Retention
| Medication Class | Examples | Mechanism of Action | Considerations in Postpartum |
|---|---|---|---|
| Parasympathomimetics | Bethanechol (Urecholine) | Stimulates muscarinic receptors in the detrusor muscle, promoting bladder contraction |
|
| Alpha-adrenergic Blockers | Tamsulosin, Alfuzosin | Relaxes smooth muscle at the bladder neck and proximal urethra, reducing outflow resistance |
|
Medications for Urinary Incontinence
| Medication Class | Examples | Type of Incontinence | Considerations in Postpartum |
|---|---|---|---|
| Anticholinergics | Oxybutynin, Solifenacin, Tolterodine, Darifenacin | Urge incontinence, Overactive bladder |
|
| Beta-3 Adrenergic Agonists | Mirabegron | Urge incontinence, Overactive bladder |
|
| Topical Estrogens | Vaginal estrogen creams, rings, or tablets | Stress or urge incontinence with urogenital atrophy |
|
Medications for Urinary Tract Infections
| Antibiotic Class | Examples | Common Dosage | Safety in Breastfeeding |
|---|---|---|---|
| Nitrofurantoin | Macrobid, Macrodantin | 100mg twice daily for 5 days |
Safe
Compatible with breastfeeding; avoid in G6PD deficiency |
| Cephalosporins | Cephalexin, Cefuroxime | 500mg four times daily for 3-7 days |
Safe
Compatible with breastfeeding |
| Penicillins | Amoxicillin-clavulanate | 875/125mg twice daily for 5-7 days |
Safe
Compatible with breastfeeding |
| Trimethoprim-sulfamethoxazole | Bactrim, Septra | 160/800mg twice daily for 3 days |
Caution
Avoid in first 2 months of breastfeeding or if infant has G6PD deficiency or hyperbilirubinemia |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | Ciprofloxacin 500mg twice daily for 3-7 days |
Caution
Generally considered compatible, but other options preferred if available |
Important Considerations
- Always check the most current resources for medication safety in breastfeeding
- Treat according to local antibiotic resistance patterns
- Adjust dosage for renal function if needed
- Complete the full course of antibiotics even if symptoms resolve
- Follow-up urine culture may be needed for complicated infections
Pain Management Considerations
Pain management is important for comfort but can impact urinary function:
| Medication Class | Examples | Effect on Urinary Function | Recommendations |
|---|---|---|---|
| NSAIDs | Ibuprofen, Diclofenac | Minimal direct effect on urinary function |
|
| Opioids | Codeine, Oxycodone, Morphine | Can cause urinary retention by increasing sphincter tone and reducing detrusor contractility |
|
| Local Anesthetics | Lidocaine spray/gel, EMLA cream | Local numbing can affect urinary sensation and control |
|
Prevention Strategies for Postnatal Urinary Complications
Prevention is the best approach to postnatal urinary complications. Implementing effective strategies during pregnancy, labor, and the postpartum period can significantly reduce the risk of developing urinary problems.
Antepartum Prevention
Pelvic Floor Exercises
- Begin pelvic floor muscle training during pregnancy
- Regular exercises (3 times daily) strengthen muscles before delivery
- Proper technique instruction from healthcare provider
- Continue throughout pregnancy unless contraindicated
Weight Management
- Maintain appropriate weight gain during pregnancy
- Follow nutritional guidelines for pregnancy
- Regular, appropriate exercise as approved by healthcare provider
Dietary Habits
- Adequate fiber intake to prevent constipation
- Proper hydration (2-3 liters daily)
- Avoidance of bladder irritants (caffeine, artificial sweeteners)
Intrapartum Prevention
Labor Management
- Regular bladder emptying during labor (every 2-4 hours)
- Consider intermittent catheterization if unable to void
- Avoid prolonged second stage of labor when possible
- Careful instrumental delivery technique when required
Anesthesia Considerations
- Use lowest effective dose of epidural anesthesia
- Early removal of epidural after delivery when appropriate
- Regular bladder emptying for women with regional anesthesia
Perineal Care
- Selective rather than routine episiotomy
- Careful perineal repair techniques
- Minimize tissue trauma during delivery
Early Postpartum Prevention
Structured Bladder Care Protocol
Implementing a structured protocol for all postpartum women:
- Document time of delivery or catheter removal
- Encourage first void within 4-6 hours
- Measure and document volume of first void
- Assess for signs of incomplete emptying
- Consider PVR assessment for high-risk women
Early Mobilization
- Encourage ambulation as soon as appropriate after delivery
- Assist to bathroom rather than offering bedpan when possible
- Provide privacy and comfortable position for voiding
Hydration Management
- Encourage adequate fluid intake (2-3 liters daily)
- Monitor intake and output
- Avoid excessive fluid loading, particularly IV fluids
Medication Considerations
- Minimize use of medications that affect bladder function
- Balance pain management with risk of urinary retention
- Consider timing of pain medication in relation to voiding attempts
Late Postpartum Prevention
Ongoing Pelvic Floor Care
- Structured pelvic floor rehabilitation program
- Continued exercises for at least 3-6 months
- Consider referral to pelvic floor physiotherapy
- Gradual return to pre-pregnancy activity level
Postpartum Check-ups
- Screen for urinary symptoms at postpartum visits
- Provide opportunity to discuss concerns
- Early intervention for developing problems
Weight Management
- Gradual return to pre-pregnancy weight
- Focus on balanced nutrition and appropriate exercise
- Avoid high-impact exercises that strain pelvic floor until recovered
Pelvic Floor Exercises for Postnatal Recovery
Pelvic floor exercises, also known as Kegel exercises, are the cornerstone of prevention and management for many postnatal urinary complications. Teaching proper technique is essential for effective outcomes.
Understanding the Pelvic Floor
Before teaching exercises, ensure women understand the anatomy and function of the pelvic floor:
- The pelvic floor is a hammock-like layer of muscles spanning from the pubic bone to the tailbone
- These muscles support the pelvic organs (bladder, uterus, rectum)
- They help control bladder and bowel function
- During pregnancy and childbirth, these muscles stretch and can become weakened
Identifying the Correct Muscles
Many women contract the wrong muscles when attempting pelvic floor exercises. Help them identify the correct muscles:
Methods to Identify Pelvic Floor Muscles
- Stop flow technique: During urination, try to stop the flow of urine mid-stream. The muscles used are the pelvic floor muscles.
- Note: This is only for identification, not as a regular exercise
- Imaginary scenarios: Imagine trying to:
- Prevent passing gas
- Pull the vagina upward
- Tighten around a tampon
- Mirror check: Using a hand mirror, the perineum should lift slightly when correctly contracting
Common Mistakes
Advise women to avoid these common errors:
- Holding breath during exercises
- Contracting abdomen, buttocks, or inner thigh muscles instead
- Bearing down instead of pulling up
- Performing exercises inconsistently
Basic Pelvic Floor Exercise Technique
Finding a Comfortable Position
Start in a comfortable position – lying down is easiest for beginners, then progress to sitting and standing:
- Lying on back with knees bent and feet flat
- Sitting on a firm chair with feet flat
- Standing with feet shoulder-width apart
Slow Contractions (Endurance)
- Empty the bladder before beginning
- Breathe normally throughout the exercise
- Tighten and lift the pelvic floor muscles
- Hold the contraction for 3-5 seconds initially (gradually build to 10 seconds)
- Completely relax the muscles for the same duration as the contraction
- Repeat 10 times (one set)
Quick Contractions (Strength)
- Rapidly tighten and lift the pelvic floor muscles
- Hold briefly (1-2 seconds)
- Release quickly
- Repeat 10 times in quick succession
Progression and Integration
- Perform 3 sets of exercises daily (morning, afternoon, evening)
- Gradually increase hold time to 10 seconds
- Progress from lying to sitting to standing positions
- Integrate exercises into daily activities (while feeding baby, waiting in line, etc.)
- Practice “the knack” – contracting pelvic floor muscles before and during activities that increase abdominal pressure (coughing, sneezing, lifting)
Helpful Tip
Set reminders on phone or associate exercises with regular daily activities (like breastfeeding or diaper changes) to help remember to do them consistently.
Advanced Techniques
Once basic techniques are mastered, women can progress to more advanced approaches:
Functional Integration
- Practice contracting before and during lifting (especially when lifting the baby)
- Contract during exercise routines
- Practice quick contractions before coughing or sneezing
Assistive Devices
For women who find it difficult to identify or contract the correct muscles:
- Vaginal Cones: Weighted devices retained in the vagina that provide resistance training
- Biofeedback Devices: Provide visual or auditory feedback about correct muscle contractions
- Smartphone Apps: Several apps can help with reminders and tracking progress
When to Refer
Consider referral to a pelvic floor physiotherapist if:
- Woman has difficulty identifying correct muscles
- No improvement after 4-6 weeks of consistent exercises
- Symptoms worsen despite exercises
- Pain occurs during exercises
- Moderate to severe urinary or fecal incontinence persists
Expected Outcomes
When performed correctly and consistently:
- Mild to moderate stress incontinence typically improves within 4-6 weeks
- Maximum benefit may take 3-6 months of consistent practice
- Long-term maintenance with daily exercises is recommended
- 80% of women with mild postpartum stress incontinence experience significant improvement with dedicated pelvic floor exercises
Red Flags and Emergency Care
While most postnatal urinary complications are not emergencies, certain signs and symptoms warrant urgent medical attention. Nurses should educate women about these warning signs and ensure prompt referral when needed.
Red Flag Signs Requiring Immediate Medical Attention
Urinary Retention Red Flags
- Inability to void for >8 hours despite urge
- Severe suprapubic pain or distention
- Bladder distention visible on inspection
- Overflow incontinence with bladder distention
- Altered mental status with urinary symptoms
Urinary Tract Infection Red Flags
- High fever (>38.5°C/101.3°F)
- Flank pain or costovertebral angle tenderness
- Rigors (shaking chills)
- Hematuria (blood in urine)
- Signs of sepsis (tachycardia, hypotension, confusion)
- Nausea/vomiting preventing oral medication intake
Escalation Protocol
When red flag signs are present, follow this protocol:
Immediate Assessment
- Vital signs (temperature, pulse, respiration, blood pressure)
- Focused assessment of symptoms
- Bladder assessment (palpation/percussion, bladder scan if available)
- Brief review of relevant history (delivery details, previous issues)
Urgent Interventions
- For acute retention:
- Straight catheterization to relieve distention
- Measure residual volume
- Consider indwelling catheter if volume >500ml
- For suspected pyelonephritis/sepsis:
- Obtain urine and blood cultures
- Initiate IV access
- Begin fluids and antipyretics
Medical Notification
- Contact obstetric provider immediately
- Provide SBAR (Situation, Background, Assessment, Recommendation) communication
- Document notification time and instructions received
Ongoing Monitoring
- Maintain close observation of vital signs
- Monitor intake and output
- Reassess symptoms regularly
- Document findings and interventions
Emergency Department Transfer Criteria
Consider emergency department transfer for any of the following:
- Signs of sepsis (altered mental status, hypotension, tachycardia)
- Severe pain unresponsive to initial interventions
- Inability to establish urinary drainage in acute retention
- Significant hematuria
- Acute kidney injury (oliguria, elevated creatinine)
- Unstable vital signs
Transfer Preparation
- Ensure IV access if indicated
- Send copy of relevant records
- Include details of recent delivery
- Document medications given
- Communicate breastfeeding status
- Arrange for infant care if needed
- Inform family members
Patient Education
Effective patient education is crucial for prevention and management of postnatal urinary complications. Education should begin during pregnancy, continue through hospital stay, and extend into postpartum follow-up visits.
Key Educational Topics
Normal Postpartum Urinary Function
- Expected changes in urination patterns after delivery
- Normal diuresis in first 24-48 hours
- Temporary changes in sensation
- Gradual return to pre-pregnancy function
Warning Signs
- Inability to void despite urge
- Frequent small volume voids
- Sensation of incomplete emptying
- Painful urination
- Urinary incontinence
- Fever, chills, or flank pain
- When and how to seek help
Preventive Practices
- Proper hydration (amount and timing)
- Voiding techniques (complete emptying, double voiding)
- Perineal hygiene practices
- Regular toileting habits (not delaying urination)
- Avoiding constipation
Pelvic Floor Exercises
- Detailed instruction on correct technique
- Practice sessions with feedback
- Recommended frequency and progression
- Integration into daily activities
- Long-term maintenance recommendations
Educational Methods and Resources
Written Materials
- Discharge instructions with clear guidance
- Illustrated pelvic floor exercise guides
- Bladder diary templates
- Resource lists for additional support
Demonstration and Practice
- One-on-one instruction on pelvic floor exercises
- Return demonstration to confirm understanding
- Models or visual aids to explain anatomy
Digital Resources
- Recommended mobile apps for exercise reminders
- Online videos for exercise technique
- Reliable websites for additional information
Teach-Back Method
To ensure understanding, use the teach-back method:
- Provide information in clear, simple language
- Ask the woman to explain or demonstrate her understanding
- Clarify any misconceptions
- Repeat process until confident in her understanding
Sample Patient Education Script: Explaining Pelvic Floor Exercises
Nurse: “Now I’d like to talk about exercises to strengthen the muscles that support your bladder and help prevent leaking urine. These are called pelvic floor or Kegel exercises.”
Explanation: “Your pelvic floor muscles are like a hammock that supports your bladder, uterus, and bowel. During pregnancy and childbirth, these muscles stretch and can become weakened. This might cause you to leak urine when you cough, laugh, or exercise.”
Finding the muscles: “To find these muscles, try to stop the flow of urine midstream the next time you use the bathroom. The muscles you use to do this are your pelvic floor muscles. But only do this to identify them – don’t make a habit of stopping your urine flow regularly.”
Exercise technique: “To exercise these muscles, tighten them as if you’re trying to stop urine flow or hold in gas. Lift and squeeze inward. Hold for a count of 3 to 5 seconds, then relax completely for the same amount of time. This is one repetition. Try to do 10 repetitions, three times a day.”
Practice and feedback: “Let’s practice now. Tighten your pelvic floor muscles… hold… and relax. Try to keep breathing normally while you do this. Also, try not to tighten your abdomen, thighs, or buttocks – focus just on the pelvic floor.”
Integration: “You can do these exercises anywhere – while feeding your baby, waiting in line, or watching TV. No one will know you’re doing them. The key is consistency. Over time, try to increase how long you hold each contraction, working up to 10 seconds.”
Teach-back: “Now, could you tell me how you would do these exercises and how often you should do them?”
Case Study: Postnatal Urinary Retention
Patient Scenario
Patient: Sarah, 28-year-old primipara (first-time mother)
Delivery: Vaginal delivery 16 hours ago after 24-hour labor with 3 hours of pushing
Interventions during delivery: Epidural anesthesia, forceps-assisted delivery, second-degree perineal tear repaired with sutures
Current status: Has not voided since delivery despite reporting feeling the urge to urinate. Complains of lower abdominal discomfort.
Assessment Findings
- Vital signs: Temperature 37.0°C, HR 85, BP 120/70, RR 18
- Visible suprapubic distention
- Palpable bladder 3cm above symphysis pubis
- Tenderness on suprapubic palpation
- Continuous small leakage of urine noted on perineal pad
- Perineal area shows moderate edema with intact sutures
- Reports pain with movement rated 6/10
Nursing Diagnosis
- Acute Urinary Retention related to effects of epidural anesthesia, perineal trauma, and postpartum edema as evidenced by inability to void for 16 hours, suprapubic distention, and discomfort
- Acute Pain related to perineal trauma and bladder distention as evidenced by patient’s report of pain 6/10 and guarding behavior
Interventions
- Initial conservative measures:
- Assisted to bathroom with privacy
- Positioned comfortably on toilet
- Ran water in sink to stimulate urination
- Poured warm water over perineum
- Assessment after failed voiding attempt:
- Performed bladder scan showing 650ml residual volume
- Catheterization:
- Obtained order for straight catheterization
- Explained procedure to patient
- Performed sterile catheterization
- Drained 700ml of clear yellow urine
- Documented procedure, amount, and urine characteristics
- Pain management:
- Administered prescribed ibuprofen 600mg
- Applied ice pack to perineum
- Positioned patient comfortably with pillows
- Education:
- Explained cause of urinary retention
- Discussed importance of regular voiding attempts
- Demonstrated double-voiding technique
- Instructed on signs of incomplete emptying
Monitoring Plan
- Scheduled voiding attempts every 3-4 hours
- Intake and output monitoring
- Post-void residual assessment via bladder scan after first spontaneous void
- Perineal assessment with each pad change
- Pain evaluation using numeric scale every 4 hours
Outcome
4 hours after catheterization, Sarah was able to void spontaneously with a volume of 250ml. Post-void bladder scan showed 80ml residual. She was instructed on double voiding, and a repeat bladder scan showed reduction to 30ml residual. Sarah continued to void without difficulty and was discharged with education on pelvic floor exercises and signs of urinary problems to report.
Learning Points from the Case
- Risk factors: primiparity, prolonged labor, epidural anesthesia, instrumental delivery, perineal trauma
- Assessment strategy: clinical evaluation + technological assessment (bladder scan)
- Conservative measures should be attempted before catheterization
- Documentation of volumes is critical for monitoring progress
- Patient education is essential for ongoing self-management
- Gradual improvement with appropriate intervention is the expected course
Mnemonics for Postnatal Urinary Complications
Mnemonics can be valuable tools to help nursing students remember key concepts related to postnatal urinary complications. Here are several useful mnemonics:
BLADDER – Risk Factors for Postnatal Urinary Retention
B – Birth trauma (instrumental delivery, prolonged labor)
L – Labor medications (epidural, opioids)
A – Age (>35 years increases risk)
D – Damage to perineum (tears, episiotomy)
D – Delivery type (first vaginal delivery)
E – Excess edema in perineal area
R – Restricted mobility after delivery
VOID – Assessment for Urinary Retention
V – Volume (measure output, normal is >150ml)
O – Obstruction signs (suprapubic distention, pain)
I – Inability to empty bladder completely
D – Distress (discomfort, frequency, urgency)
PREVENT – Preventive Strategies for Postnatal Urinary Complications
P – Pelvic floor exercises daily
R – Regular voiding (every 2-3 hours)
E – Early mobilization after delivery
V – Volume of fluids (maintain adequate hydration)
E – Emptying bladder completely (double voiding)
N – Normal defecation (prevent constipation)
T – Timely treatment of infections
LEAKS – Types of Urinary Incontinence
L – Laughing/coughing (stress incontinence)
E – Emergency rushing (urge incontinence)
A – Always dribbling (overflow incontinence)
K – Kinds combined (mixed incontinence)
S – Sensory issues (functional incontinence)
CATHETER – Care of Indwelling Catheters
C – Clean perineal area daily
A – Aseptic technique during insertion
T – Tubing positioned below bladder level
H – Hydration adequate to maintain output
E – Empty drainage bag regularly
T – Tug-free, secure attachment
E – Evaluate for signs of infection
R – Remove as soon as clinically appropriate
UTI – Signs of Urinary Tract Infection
U – Uncomfortable urination (dysuria, frequency)
T – Temperature elevated (fever)
I – Intense pain (suprapubic, flank)
PELVIC FLOOR – Teaching Kegel Exercises
P – Position comfortably (lying, sitting, standing)
E – Empty bladder before starting
L – Lift and squeeze muscles inward
V – Verify correct muscles (not abdomen or thighs)
I – Inhale and exhale normally during exercise
C – Count during contraction (3-10 seconds)
F – Fully relax between contractions
L – Long-term commitment (daily practice)
O – Often repeat (10 repetitions, 3 times daily)
O – Observe for improvement over weeks
R – Regularly integrate into daily activities
