Postnatal Vulval Hematoma: Comprehensive Nursing Notes
Table of Contents
- Introduction to Postnatal Vulval Hematoma
- Relevant Anatomy and Physiology
- Pathophysiology of Vulval Hematoma
- Etiology and Risk Factors
- Classification of Puerperal Genital Hematomas
- Clinical Presentation
- Signs and Symptoms
- Clinical Findings
- Diagnosis and Assessment
- Nursing Assessment
- Diagnostic Studies
- Differential Diagnosis
- Management of Vulval Hematoma
- Conservative Management
- Surgical Management
- Nursing Management
- Nursing Diagnoses
- Nursing Interventions
- Complications
- Prognosis
- Prevention Strategies
- Patient Education
- Discharge Planning and Home Care
- Psychological Aspects
- Documentation Guidelines
- Current Research and Evidence-Based Practice
- Case Studies
- Summary
- References
Introduction to Postnatal Vulval Hematoma
A vulval hematoma is a localized collection of blood within the soft tissues of the vulva, occurring due to trauma or spontaneous rupture of blood vessels in the perineal region. When occurring in the postpartum period (postnatal), these hematomas represent a potentially serious complication that requires prompt recognition and management. While postnatal vulval hematomas are relatively uncommon, with incidence ranging from 1 in 300 to 1 in 15,000 deliveries, they can lead to significant maternal morbidity and, in rare cases, mortality if not properly managed.
Understanding the anatomical basis, risk factors, clinical presentation, and management strategies for postnatal vulval hematomas is essential for nursing professionals working in obstetric settings. These nursing notes aim to provide a comprehensive overview of this condition, with a focus on evidence-based nursing assessment and interventions to optimize patient outcomes and minimize complications.
Key Point:
Postnatal vulval hematoma is an accumulation of blood in the vulval tissues following childbirth, representing a potentially serious complication that requires vigilant nursing assessment and prompt intervention.
Relevant Anatomy and Physiology
To understand the development and management of postnatal vulval hematoma, a solid grasp of the relevant anatomy is essential for nursing professionals.
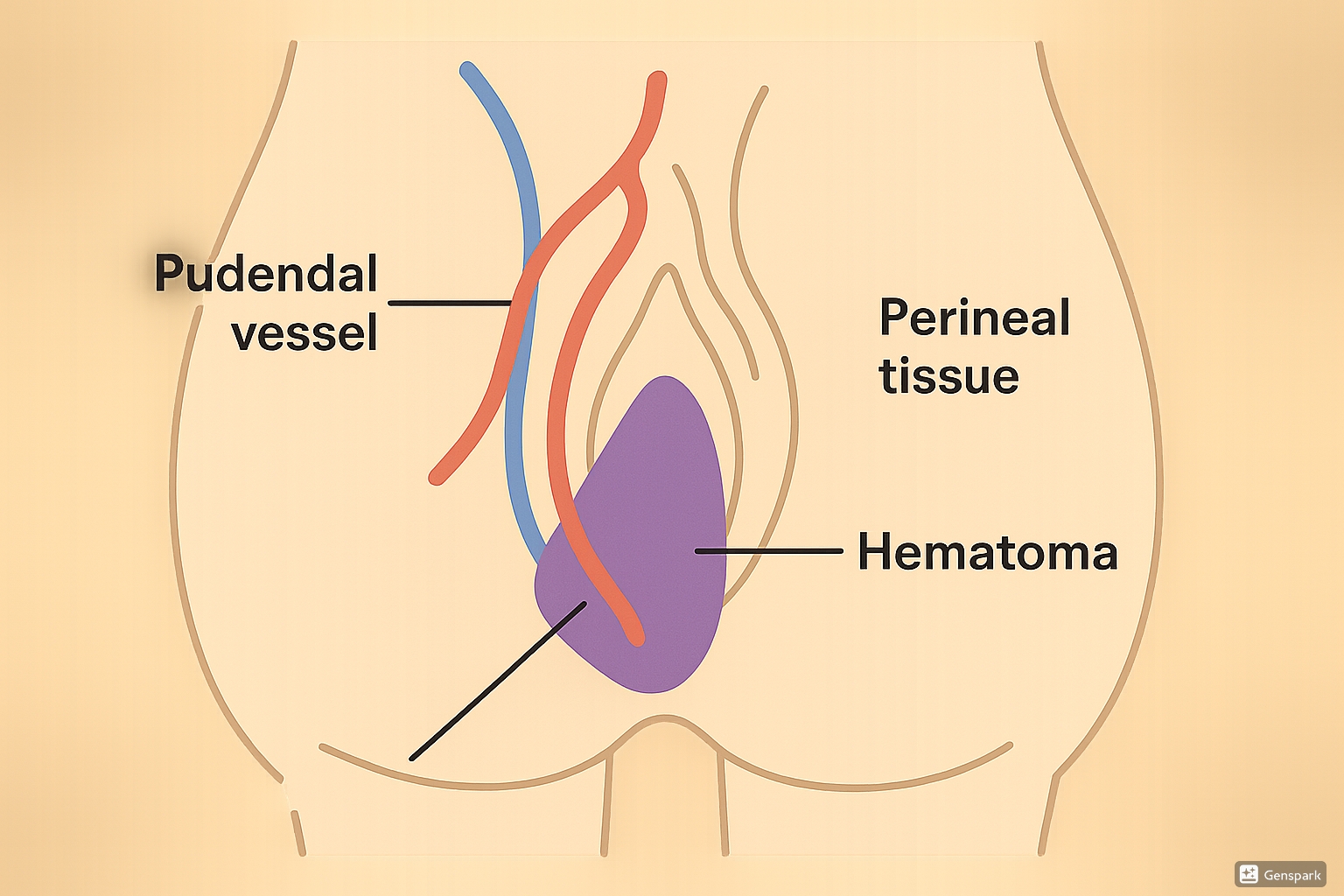
Vulval Anatomy
The vulva comprises several external genital structures including the mons pubis, labia majora, labia minora, clitoris, vestibule, and perineum. These structures consist primarily of soft tissue with abundant vascular supply and loose connective tissue, making them susceptible to significant blood accumulation when blood vessels are damaged.
Blood Supply
The vulva receives its primary blood supply from branches of the pudendal artery, which is a branch of the internal iliac artery. The pudendal vessels run through the Alcock’s canal (pudendal canal) and give rise to:
- Inferior rectal arteries
- Perineal arteries
- Posterior labial arteries
- Deep and dorsal arteries of the clitoris
The extensive vascular network and the loose connective tissue of the vulva create an environment where even minor vascular trauma can lead to significant bleeding and hematoma formation.
Fascial Boundaries
The vulva is bound by fascial planes that can compartmentalize bleeding. Understanding these fascial boundaries helps explain why some vulval hematomas remain localized while others extend into adjacent regions:
- Superficial perineal fascia (Colles’ fascia): Limits superficial vulval hematomas
- Deep perineal fascia: Forms the floor of the superficial perineal space
- Urogenital diaphragm: Separates superficial and deep perineal spaces
These fascial boundaries play a crucial role in determining the extent and spread of hematomas in the perineal region. When a vessel ruptures, the fascial boundaries may initially contain the bleeding, but as the hematoma expands, it may extend along fascial planes to involve adjacent structures.
Pathophysiology of Vulval Hematoma
The pathophysiology of postnatal vulval hematoma involves vascular injury, blood extravasation, and subsequent collection within tissue spaces. Understanding this process is fundamental for effective nursing assessment and intervention.
Etiology and Risk Factors
Postnatal vulval hematomas typically develop due to trauma sustained during childbirth. The primary mechanisms include:
| Mechanism | Description | Associated Risk Factors |
|---|---|---|
| Direct Trauma | Direct injury to blood vessels during vaginal delivery | Operative vaginal deliveries (forceps, vacuum), macrosomia, rapid second stage of labor |
| Surgical Incisions | Inadequate hemostasis after episiotomy or repair of perineal tears | Midline or mediolateral episiotomy, extended episiotomy, 3rd or 4th degree lacerations |
| Pressure Necrosis | Pressure from prolonged fetal head impaction causing vessel wall necrosis | Prolonged second stage of labor, cephalopelvic disproportion |
| Spontaneous Vessel Rupture | Rupture of pre-existing vascular abnormalities during labor | Varicose veins, vascular malformations, coagulopathies |
Specific Risk Factors
Several factors increase the risk of developing postnatal vulval hematoma:
- Obstetric factors:
- Nulliparity (first-time delivery)
- Operative vaginal delivery (forceps or vacuum assistance)
- Prolonged second stage of labor
- Fetal macrosomia (birth weight >4000g)
- Episiotomy, particularly mediolateral
- Higher-degree perineal tears
- Maternal factors:
- Coagulation disorders
- Anticoagulant therapy
- Pre-existing vulvar varicosities
- Hypertensive disorders
- Previous history of vulval hematoma
Warning:
Patients with pre-existing coagulation disorders or those on anticoagulant therapy require increased vigilance for vulval hematoma formation after delivery.
Classification of Puerperal Genital Hematomas
Puerperal genital hematomas can be classified based on their anatomical location, which influences their clinical presentation, management, and prognosis:
| Classification | Location | Clinical Features |
|---|---|---|
| Vulvovaginal (Vulvar) Hematomas | Below the pelvic diaphragm, involving vulvar tissues | Visible external swelling, severe perineal pain, unilateral vulvar swelling |
| Paravaginal Hematomas | Above the pelvic diaphragm, along vaginal walls | May not be externally visible, abdominal pain, urinary retention, rectal pressure |
| Subperitoneal (Retroperitoneal) Hematomas | Extends into retroperitoneal space | Severe abdominal pain, hemodynamic instability, abdominal distension, may not have external signs |
Additionally, vulval hematomas can be classified based on their size:
- Small: <5 cm in diameter
- Medium: 5-10 cm in diameter
- Large: >10 cm in diameter
The size classification is clinically relevant as it often dictates the management approach, with larger hematomas more likely to require surgical intervention.
Clinical Presentation
Signs and Symptoms
The clinical presentation of postnatal vulval hematoma varies depending on the size, location, and rate of hematoma formation. Nurses should be vigilant for the following signs and symptoms:
Mnemonic: “HEMATOMA”
Common presenting symptoms include:
- Pain: Usually the earliest and most prominent symptom. The pain is often described as severe, constant, and throbbing.
- Swelling: Progressive enlargement of vulvar tissues, typically unilateral.
- Pressure symptoms: Sensation of perineal pressure or fullness.
- Urinary symptoms: Difficulty urinating or urinary retention due to urethral compression.
- Rectal pressure: Sensation of rectal fullness or difficulty with defecation.
- Systemic symptoms: In severe cases, signs of hypovolemia including tachycardia, hypotension, dizziness, and pallor.
Nursing Alert:
The degree of pain may not always correlate with the size of the vulval hematoma. Even small hematomas can cause severe pain due to the rich innervation of vulvar tissues. Never dismiss patient complaints of severe perineal pain, even if external signs are minimal.
Clinical Findings
Physical examination findings in postnatal vulval hematoma may include:
Local Findings:
- Visible vulvar swelling, often unilateral
- Discoloration of the overlying skin (bluish, purple, or ecchymotic)
- Tense, firm, and tender mass on palpation
- Distortion of normal vulvar anatomy
- Possible extension into vagina (detected on vaginal examination)
Systemic Findings (in severe cases):
- Tachycardia
- Hypotension
- Pallor
- Diaphoresis
- Altered level of consciousness
The time course of symptom onset is clinically significant:
- Early onset: Symptoms developing within 1-2 hours of delivery typically indicate arterial bleeding
- Delayed onset: Symptoms developing 6-24 hours postpartum often suggest venous bleeding
| Time of Onset | Likely Source | Clinical Implications |
|---|---|---|
| Within 1-2 hours postpartum | Arterial bleeding | More likely to expand rapidly and cause hemodynamic instability |
| 6-24 hours postpartum | Venous bleeding | Usually slower to expand but may reach significant size |
| 24+ hours postpartum | Delayed bleeding or hematoma expansion | May indicate coagulation issues or missed initial diagnosis |
Diagnosis and Assessment
Nursing Assessment
Thorough nursing assessment is crucial for early identification of postnatal vulval hematoma. The assessment should include:
History Taking:
- Details of labor and delivery (duration, mode of delivery, use of instruments)
- Presence and extent of perineal trauma (episiotomy, lacerations)
- Repair techniques used
- Timing of symptom onset
- Character and severity of pain
- Associated symptoms (urinary retention, rectal pressure)
- Medical history, especially bleeding disorders or anticoagulant use
Physical Examination:
- Vital signs assessment with attention to signs of hypovolemia
- Inspection of the vulvar area (swelling, asymmetry, discoloration)
- Gentle palpation to assess size, consistency, and tenderness
- Assessment of urinary output and ability to void
- Evaluation of lochia (amount, character) to differentiate from other causes of postpartum bleeding
Nursing Tip:
Regular perineal assessments in the immediate postpartum period are essential for early detection of vulval hematoma. Pay particular attention to patients who report perineal pain out of proportion to visible trauma or who have had instrumental deliveries.
Diagnostic Studies
While diagnosis of vulval hematoma is primarily clinical, additional studies may be ordered to assess the extent of the hematoma or to monitor the patient’s condition:
| Diagnostic Study | Purpose | Nursing Considerations |
|---|---|---|
| Complete Blood Count (CBC) | Assess for anemia, monitor hemoglobin and hematocrit levels | Trend values to detect ongoing blood loss; baseline and serial measurements are important |
| Coagulation Studies | Evaluate for underlying coagulation disorders | Important in cases with excessive bleeding or history of bleeding disorders |
| Ultrasonography | Determine size, extent, and location of hematoma | Helpful in assessing deeper hematomas or those extending into paravaginal spaces |
| CT Scan | Evaluate extent of larger hematomas, especially those extending retroperitoneally | Usually reserved for cases with suspected extensive involvement or when ultrasound findings are inconclusive |
| MRI | Detailed assessment of tissue planes and extent of hematoma | Rarely needed but may be useful in complex cases |
Differential Diagnosis
Several conditions may present with symptoms similar to vulval hematoma and should be considered in the differential diagnosis:
- Vulvar edema: Diffuse swelling without discoloration or mass effect
- Perineal abscess: Usually presents later (days to weeks postpartum) with signs of infection
- Bartholin’s gland cyst or abscess: Localized to the vestibule
- Vulvar varicosities: Compressible, non-tender unless thrombosed
- Retained vaginal packing: History of prior packing placement
- Vulvar neoplasm: Usually chronic, without acute onset
Management of Vulval Hematoma
The management of postnatal vulval hematoma depends on several factors, including the size of the hematoma, hemodynamic stability of the patient, rate of expansion, severity of symptoms, and available resources. Management strategies can be broadly categorized as conservative or surgical.
Conservative Management
Conservative management is appropriate for small to medium-sized hematomas (<10 cm) in hemodynamically stable patients. It includes:
Pain Management:
- Analgesics (NSAIDs, acetaminophen)
- Opioids for moderate to severe pain
- Local anesthetic agents (topical lidocaine)
Local Measures:
- Ice packs: Applied to the vulvar area for the first 24 hours to reduce swelling and provide analgesia
- Compression: Gentle pressure with sanitary pads to prevent further expansion
- Sitz baths: After 24 hours to promote circulation and healing
Supportive Care:
- Bed rest with elevation of the pelvic region
- Avoidance of prolonged sitting or standing
- Monitoring of vital signs and hematoma size
- Urinary catheterization if urinary retention is present
Systemic Therapy:
- Prophylactic antibiotics (controversial, but often prescribed to prevent secondary infection)
- Iron supplementation for anemic patients
- Blood transfusion if significant blood loss has occurred
Nursing Tip:
When applying ice packs to a vulval hematoma, ensure they are wrapped in a cloth and applied for 15-20 minutes at a time, with breaks in between to prevent tissue injury. Document the timing of ice application and assess the skin regularly for signs of cold injury.
Surgical Management
Surgical intervention is indicated for vulval hematomas that are:
- Large (>10 cm in diameter)
- Rapidly expanding
- Associated with hemodynamic instability
- Causing severe pain unresponsive to conservative management
- Causing significant pressure symptoms (urinary retention, rectal compression)
- Not resolving with conservative management
Surgical procedures may include:
1. Evacuation and Drainage:
- Incision over the most prominent part of the hematoma
- Evacuation of clots
- Identification and ligation of bleeding vessels when possible
- Placement of drainage tube or packing
- Primary or delayed closure of the incision
2. Arterial Embolization:
- Performed by interventional radiology
- Particularly useful for hematomas with identified arterial bleeding source
- Less invasive alternative to surgical exploration
- Requires specialized facilities and expertise
| Management Approach | Indications | Procedures | Nursing Considerations |
|---|---|---|---|
| Conservative |
|
|
|
| Surgical |
|
|
|
Nursing Management
Nursing management of the patient with a postnatal vulval hematoma is multifaceted and focuses on assessment, pain management, monitoring for complications, and provision of holistic care.
Nursing Diagnoses
Common nursing diagnoses for patients with postnatal vulval hematoma include:
- Acute Pain related to tissue trauma and expansion of hematoma as evidenced by verbal reports of pain, guarding behavior, and facial grimacing
- Impaired Physical Mobility related to pain and discomfort as evidenced by difficulty ambulating and need for assistance with activities
- Impaired Urinary Elimination related to urethral compression as evidenced by inability to void or incomplete bladder emptying
- Risk for Infection related to tissue trauma and proximity to perineal area
- Deficient Knowledge regarding self-care and recovery process as evidenced by questions about management and recovery
- Situational Low Self-Esteem related to altered body image and function as evidenced by expressions of embarrassment or distress
- Ineffective Sexuality Pattern related to perineal pain and discomfort as evidenced by concerns about resuming sexual activity
- Risk for Ineffective Breastfeeding related to discomfort in sitting position
- Anxiety related to unfamiliar situation and concern about recovery as evidenced by restlessness and verbalization of concerns
- Risk for Deficient Fluid Volume related to potential blood loss as evidenced by changes in vital signs or laboratory values
Nursing Interventions
1. Assessment and Monitoring:
- Perform comprehensive assessment at regular intervals:
- Vital signs (with focus on signs of hypovolemia)
- Size, appearance, and progression of hematoma
- Pain level using standardized pain scale
- Urinary output and ability to void
- Lochia (amount, color, odor)
- Monitor laboratory values (hemoglobin, hematocrit, coagulation studies)
- Assess for signs of infection (fever, increased pain, purulent discharge)
Mnemonic: “VULVAL” Assessment
2. Pain Management:
- Administer prescribed analgesics as scheduled and PRN
- Apply ice packs to the perineal area for the first 24 hours
- Position patient for comfort (side-lying position often preferred)
- Use supportive cushions or rings for sitting
- Provide distraction techniques and relaxation strategies
- Document pain levels before and after interventions
3. Wound Care and Perineal Hygiene:
- Provide meticulous perineal care after each void or bowel movement
- Use peri-bottle with warm water for cleansing
- Pat dry gently (avoid rubbing)
- Change perineal pads frequently
- Assist with sitz baths after the first 24 hours
- For surgical cases, perform wound care per protocol:
- Drain management if present
- Dressing changes using aseptic technique
- Monitor for signs of infection
4. Promotion of Elimination:
- Monitor urinary output
- Perform intermittent catheterization or insert indwelling catheter if necessary
- Encourage adequate fluid intake
- Provide privacy for elimination
- Administer stool softeners as ordered to prevent constipation
- Educate about avoiding straining during defecation
5. Mobility and Self-Care Assistance:
- Assist with position changes and ambulation
- Teach techniques for movement with minimal discomfort
- Provide assistive devices as needed
- Assist with personal hygiene as required
- Gradually increase activity as tolerated
6. Psychological Support:
- Provide emotional support and reassurance
- Address concerns about body image and sexuality
- Include partner in discussions when appropriate
- Facilitate communication with healthcare providers
- Assess for signs of postpartum depression or anxiety
- Refer to mental health services if needed
7. Breastfeeding Support:
- Assist with positioning for comfortable breastfeeding
- Provide side-lying breastfeeding option
- Use supportive pillows
- Ensure pain management is optimal during feeding times
- Refer to lactation consultant if needed
Nursing Alert:
Monitor for signs of expanding vulval hematoma (increasing pain, enlarging mass, deteriorating vital signs) and report immediately to the healthcare provider. An expanding hematoma may require urgent surgical intervention.
Complications
Postnatal vulval hematoma, if not promptly recognized and appropriately managed, can lead to several complications:
| Complication | Description | Prevention/Management |
|---|---|---|
| Hypovolemic Shock | Significant blood loss leading to hemodynamic instability; more common with large hematomas | Early recognition, fluid resuscitation, blood transfusion if needed, surgical intervention for ongoing bleeding |
| Infection | Secondary infection of the hematoma or surrounding tissues | Meticulous perineal hygiene, prophylactic antibiotics in some cases, prompt treatment if infection develops |
| Abscess Formation | Collection of purulent material following infection of the hematoma | Surgical drainage, appropriate antimicrobial therapy |
| Pressure Necrosis | Tissue necrosis due to pressure from large hematomas compromising blood supply | Early evacuation of large hematomas, position changes, monitoring for signs of tissue compromise |
| Prolonged Pain | Persistent pain beyond the expected healing period | Appropriate pain management, addressing contributing factors, physical therapy if needed |
| Sexual Dysfunction | Dyspareunia, fear of resuming sexual activity, altered body image | Counseling, education about healing process, referral to sexual health specialists if needed |
| Urinary Complications | Retention, urinary tract infection secondary to catheterization | Prompt catheterization when needed, aseptic technique, removal of catheter as soon as feasible |
| Persistent Hematoma | Non-resolving or recurrent hematoma | Surgical evacuation, investigation for underlying vascular abnormalities or coagulation disorders |
| Psychological Impact | Anxiety, depression, trauma related to the experience | Emotional support, counseling, screening for postpartum depression/anxiety |
Warning:
Signs of infection in a vulval hematoma include increasing pain, erythema of surrounding tissues, purulent discharge, foul odor, and fever. Report these signs promptly as they may indicate abscess formation requiring drainage.
Prognosis
The prognosis for patients with postnatal vulval hematoma is generally good with appropriate and timely management.
- Small to medium hematomas: Usually resolve within 2-3 weeks with conservative management
- Surgically evacuated hematomas: Typically heal within 2-4 weeks depending on the extent of dissection required
- Resolution timeline:
- Pain and swelling: Begin to improve within 3-5 days
- Discoloration: May persist for 2-3 weeks
- Complete resolution: Usually within 4-6 weeks
- Long-term outcomes: Most patients recover fully without permanent sequelae
Factors that may influence prognosis include:
- Size and location of the hematoma
- Timeliness of diagnosis and intervention
- Presence of complications (infection, necrosis)
- Underlying maternal conditions (coagulopathies, vascular disorders)
- Quality of follow-up care
Prevention Strategies
While not all cases of postnatal vulval hematoma are preventable, several strategies may reduce the risk or severity:
Antepartum Measures:
- Identification of high-risk patients (coagulation disorders, previous vulval hematoma)
- Management of vulvar varicosities during pregnancy
- Correction of anemia prior to delivery
- Optimization of coagulation status in patients with known disorders
Intrapartum Measures:
- Careful use of instrumental delivery (forceps, vacuum)
- Judicious use of episiotomy
- Controlled delivery of the fetal head to minimize perineal trauma
- Meticulous repair of perineal tears with proper hemostasis
- Thorough inspection of the perineum following repair
Postpartum Measures:
- Regular perineal assessments in the immediate postpartum period
- Early application of ice to the perineum
- Prompt investigation of disproportionate perineal pain
- Monitoring for signs of concealed bleeding
- Avoidance of constipation (stool softeners, adequate hydration)
Nursing Tip:
Teach patients to report persistent or increasing perineal pain, as this may be the earliest sign of vulval hematoma formation. Early recognition leads to more prompt intervention and improved outcomes.
Patient Education
Comprehensive patient education is essential for optimal recovery and prevention of complications in cases of postnatal vulval hematoma.
Education Topics:
1. Understanding the Condition:
- Simple explanation of what a vulval hematoma is and how it forms
- Expected timeline for healing and resolution
- Reassurance about long-term outcomes
- Explanation of treatment plan and rationale
2. Self-Care Measures:
- Perineal care:
- Cleansing techniques (peri-bottle use, front-to-back wiping)
- Pad changing frequency
- Perineal hygiene after elimination
- Pain management:
- Proper use of prescribed medications
- Ice application technique (first 24 hours)
- Sitz bath instructions (after 24 hours)
- Positioning for comfort
- Activity guidelines:
- Appropriate rest periods
- Gradual increase in activities
- Avoidance of prolonged sitting
- Safe lifting techniques
Mnemonic: “PERINEAL” Self-Care
Discharge Planning and Home Care
Effective discharge planning ensures continued recovery after the patient leaves the healthcare facility:
Instructions for Home Care:
- Written instructions for perineal care and pain management
- Medication schedules and side effect information
- Supplies needed at home (peri-bottle, ice packs, perineal pads)
- Activity restrictions and progressive return to normal activities
- Instructions for sitz baths
- Dietary recommendations to promote healing and prevent constipation
Warning Signs to Report:
- Increasing pain or swelling
- Signs of infection (fever, increased redness, purulent discharge)
- Heavy vaginal bleeding
- Inability to urinate
- Foul-smelling vaginal discharge
- Reopening of surgical incision (if applicable)
Follow-Up Care:
- Scheduled follow-up appointments
- Contact information for questions or concerns
- Instructions for when to seek immediate medical attention
- Referrals to specialists if needed (pelvic floor physical therapy, wound care)
Psychological Aspects
The psychological impact of a postnatal vulval hematoma should not be overlooked:
- Body image concerns: Reassurance about the temporary nature of changes
- Anxiety about recovery: Clear information about healing timeline
- Impact on parenting: Strategies for infant care despite discomfort
- Sexual health concerns: Discussion about when to resume activity and what to expect
- Emotional support: Resources for additional support if needed
- Partner education: Including partners in discussions when appropriate
Warning:
Monitor patients with vulval hematoma for signs of postpartum depression or anxiety, which may be exacerbated by the additional stress and discomfort of this complication. Use validated screening tools and refer for mental health support when indicated.
Documentation Guidelines
Proper documentation is essential for continuity of care and legal purposes. Documentation for patients with postnatal vulval hematoma should include:
Essential Elements of Documentation:
- Assessment findings:
- Size, location, and appearance of the hematoma
- Vital signs
- Pain level (using standardized scale)
- Associated symptoms (urinary retention, mobility limitations)
- Interventions performed:
- Medications administered (analgesics, antibiotics)
- Local measures applied (ice, sitz baths)
- Perineal care provided
- Assistance with elimination
- Patient response:
- Changes in pain level after interventions
- Tolerance of activities
- Ability to perform self-care
- Emotional status
- Education provided:
- Topics covered
- Patient’s understanding
- Educational materials given
- Questions addressed
- Communication with healthcare team:
- Consultations requested
- Provider notifications
- Orders received
- Interdisciplinary collaboration
Documentation Tip:
When documenting vulval hematoma assessment, include specific measurements when possible (e.g., “right-sided labial hematoma measuring approximately 6 cm x 4 cm”) rather than subjective descriptions. This provides more accurate tracking of changes over time.
Current Research and Evidence-Based Practice
Research on postnatal vulval hematoma continues to evolve, with several areas of investigation:
Recent Advances:
- Minimally invasive approaches: Arterial embolization as an alternative to surgical evacuation
- Risk prediction models: Identifying patients at highest risk for developing vulval hematoma
- Conservative management protocols: Standardized approaches to non-surgical management
- Novel hemostatic agents: For use during perineal repair to prevent hematoma formation
- Imaging techniques: Enhanced methods for evaluating extent and progression of hematomas
Evidence-Based Recommendations:
- Regular perineal assessment in the immediate postpartum period, particularly for high-risk deliveries
- Early application of ice to the perineum after delivery to reduce swelling and risk of hematoma formation
- Surgical evacuation for hematomas >10 cm or those causing hemodynamic instability
- Conservative management with close monitoring for smaller, stable hematomas
- Antibiotic prophylaxis remains controversial but is often employed in clinical practice
- Multimodal pain management strategies for optimal pain control
“Prompt recognition and appropriate management of vulvar hematomas are essential for reducing maternal morbidity. The decision between conservative and surgical management should be individualized based on hematoma size, hemodynamic stability, and symptom severity.” – American College of Obstetricians and Gynecologists
Case Studies
Case Study 1: Small Vulval Hematoma with Conservative Management
Patient Profile: 28-year-old G1P1, vaginal delivery with second-degree perineal laceration
Presentation: Four hours after delivery, the patient reported increasing perineal pain disproportionate to visible trauma. Assessment revealed a 4 cm x 3 cm firm, tender swelling of the right labia majora with bluish discoloration.
Management:
- Ice application to the perineum
- Analgesics (ibuprofen and acetaminophen alternating)
- Bed rest with pelvic elevation
- Regular assessment of hematoma size and vital signs
- After 24 hours, sitz baths three times daily
Outcome: The hematoma did not expand beyond its initial size. Pain began to decrease after 48 hours. The patient was discharged on day 3 postpartum with instructions for continued perineal care. Complete resolution occurred within three weeks.
Nursing Considerations: Frequent assessment, effective pain management, and detailed discharge education were key factors in successful management.
Case Study 2: Large Vulval Hematoma Requiring Surgical Intervention
Patient Profile: 32-year-old G2P2, forceps-assisted delivery with mediolateral episiotomy
Presentation: Two hours after delivery, the patient experienced severe perineal pain and pressure. Assessment revealed a rapidly expanding left vulval hematoma measuring approximately 8 cm x 6 cm. The patient developed tachycardia (HR 112) and hypotension (BP 90/60 mmHg).
Management:
- IV fluid resuscitation
- Urgent surgical consultation
- Evacuation of hematoma under general anesthesia
- Identification and ligation of bleeding vessels
- Placement of drain
- Blood transfusion (2 units packed red blood cells)
- Broad-spectrum antibiotics
Outcome: Hemodynamic stability was restored following surgery. The drain was removed after 48 hours. The patient required continued pain management but improved progressively. She was discharged on day 5 postpartum with complete healing at the 4-week follow-up visit.
Nursing Considerations: Early recognition of hemodynamic instability, prompt notification of the surgical team, meticulous postoperative care including drain management, and comprehensive discharge planning were critical to the positive outcome.
Summary
Postnatal vulval hematoma represents a potentially serious complication of childbirth that requires vigilant nursing assessment and prompt intervention. Key points from these comprehensive notes include:
- Understanding the anatomy and vascular supply of the vulva is essential for recognizing and managing vulval hematomas
- Risk factors include instrumental deliveries, episiotomy, perineal tears, and coagulation disorders
- Clinical presentation typically involves severe perineal pain and swelling, often unilateral
- Management depends on hematoma size, hemodynamic stability, and symptom severity:
- Small to medium hematomas (<10 cm): Conservative management
- Large or expanding hematomas (>10 cm): Surgical evacuation
- Nursing management focuses on assessment, pain control, prevention of complications, and patient education
- Potential complications include infection, necrosis, abscess formation, and psychological impact
- Prognosis is generally favorable with appropriate and timely intervention
Nursing professionals play a crucial role in the early detection, management, and education of patients with postnatal vulval hematoma. Through comprehensive assessment, evidence-based interventions, and holistic care, nurses can significantly contribute to improved patient outcomes and reduced morbidity associated with this complication.
References
- StatPearls. (2023). Vulvar Hematoma. https://www.ncbi.nlm.nih.gov/books/NBK560753/
- Cekmez, Y., & Şanlıkan, F. (2022). Postpartum spontaneous vulvar hematoma as a cause of maternal morbidity: A case report. Journal of Medical Case Reports, 16(1). https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-022-03281-2
- Kiyama, A., & Terashima, H. (2023). Large Vaginal Hematoma in a Puerperium Patient: Treating a Delayed Diagnosis & Management Caused by an Incomplete Clinical Examination. Cureus. https://www.cureus.com/articles/129128-large-vaginal-hematoma-in-a-puerperium-patient
- Cleveland Clinic. (2023). Vaginal Hematoma: Causes, Symptoms & Treatment. https://my.clevelandclinic.org/health/diseases/vaginal-hematoma
- Merck Manual Professional Version. (2023). Postpartum Care. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-care
- Nurseslabs. (2023). Postpartum Hemorrhage Nursing Care Plans. https://nurseslabs.com/postpartum-hemorrhage-nursing-care-plans/
- Zhang, L., et al. (2024). Risk factors and management of perineal genital hematoma: A systematic review. International Journal of Gynecology & Obstetrics. https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/ijgo.15463
- ACOG Committee Opinion. (2018). Prevention and Management of Obstetric Lacerations at Vaginal Delivery. American College of Obstetricians and Gynecologists.
- Brookside Press. (2023). Hematomas – Obstetric and Newborn Care II. https://brooksidepress.org/ob_newborn_care_2/?page_id=320
- The Journal of Obstetrics and Gynaecology. (2022). Post-Partum Vulva Hematoma Management in a Low Resource Setting. https://www.tjog.org/index.php/tjog/article/view/508/451
- Saxena, M. (2021). Vulvovaginal hematoma. Slideshare. https://www.slideshare.net/slideshow/vulvovaginal-hematoma-dr-mitra-saxena/250141900
- Nurse Together. (2022). Postpartum Hemorrhage: Nursing Diagnoses, Care Plans. https://www.nursetogether.com/postpartum-hemorrhage-nursing-diagnosis-care-plan/
