Postpartum Thrombophlebitis
Comprehensive Nursing Notes for Students
Table of Contents
Definition
Postpartum thrombophlebitis refers to inflammation with the formation of blood clots (thrombi) that occurs during the postpartum period, typically within 6-8 weeks after childbirth. It involves inflammation of a vein (phlebitis) accompanied by the formation of a blood clot (thrombus) that adheres to the wall of the blood vessel, potentially obstructing blood flow.
The condition occurs in approximately 1 in 1500 pregnancies, making it a relatively rare but serious postpartum complication. The postpartum period presents a particularly high-risk time for thrombotic events due to the physiological changes that occur during pregnancy and delivery.
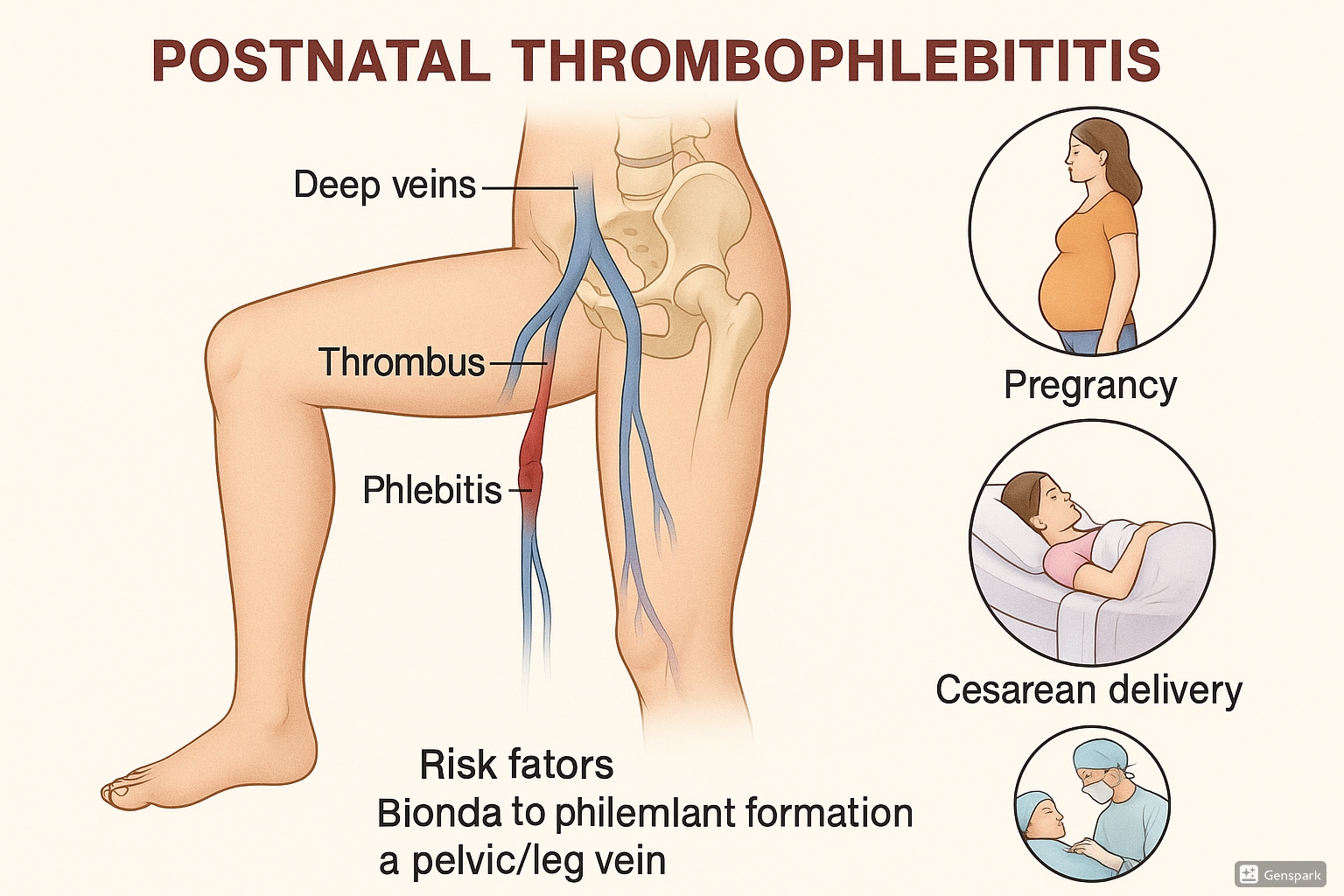
Fig. 1: Postpartum Thrombophlebitis showing blood clot formation and inflammation in the pelvic and leg veins with associated risk factors
Types of Postpartum Thrombophlebitis
There are three main types of thrombophlebitis that can occur during the postpartum period:
Superficial Venous Thrombosis (SVT)
Involves inflammation and clotting in veins close to the skin’s surface, most commonly the saphenous vein of the lower leg. It presents with localized symptoms and is generally less serious than deep vein thrombosis.
Characteristics: More prevalent postpartum than during pregnancy, especially in women with varicose veins. The affected vein appears painful, hard, reddened, and warm and is easily visible.
Deep Vein Thrombosis (DVT)
Involves inflammation and clotting in the deep veins, typically in the legs, pelvis, or thighs. More serious than SVT due to potential complications.
Characteristics: May involve veins from the feet to the femoral area. Approximately 50% of clients with DVT are asymptomatic, making it potentially more dangerous. Characterized by pain, calf tenderness, leg edema, and color changes.
Septic Pelvic Thrombophlebitis (SPT)
A rare postpartum complication characterized by an infected thrombus in the pelvic veins, often associated with endometritis or chorioamnionitis.
Characteristics: Frequently follows cesarean delivery. May present with prolonged fever despite antibiotic therapy, with or without abdominal pain. Often responds to systemic anticoagulation.
Understanding these distinct types is crucial for appropriate assessment and management, as each presents differently and carries various levels of risk. While superficial thrombophlebitis may be managed conservatively, deep vein thrombosis and septic pelvic thrombophlebitis require more aggressive intervention to prevent serious complications.
Pathophysiology
Postpartum thrombophlebitis develops through a complex interplay of physiological factors unique to the postpartum state. The pathophysiology is best understood through Virchow’s triad, which identifies three primary factors contributing to thrombosis formation:
Virchow’s Triad in Postpartum Thrombophlebitis
- Venous Stasis: The enlarged uterus during pregnancy can compress pelvic veins, particularly the inferior vena cava and left iliac vein, reducing blood flow in the lower extremities. This stasis persists into the early postpartum period. Additionally, decreased mobility following delivery, especially after cesarean sections, further promotes venous stasis.
- Hypercoagulability: Pregnancy naturally induces a hypercoagulable state that continues into the postpartum period. During pregnancy, levels of fibrinogen and other clotting factors (factors VII, VIII, IX, and X) increase, while levels of clot-dissolving factors naturally decrease. This hypercoagulable state serves as a protective mechanism against excessive bleeding during delivery but increases thrombosis risk postpartum.
- Vascular Injury: Trauma to blood vessels can occur during vaginal delivery or cesarean section. Endothelial damage to vessel walls initiates the clotting cascade, promoting thrombus formation. In cases of infection (like endometritis), inflammation can damage vascular endothelium, contributing to septic pelvic thrombophlebitis.
Specific Postpartum Factors
Several unique elements in the postpartum period contribute to thrombophlebitis development:
- Hormonal Changes: The rapid decline in estrogen and progesterone levels after delivery affects vascular tone and coagulation profiles.
- Increased Blood Volume: During pregnancy, blood volume increases by approximately 50%. After delivery, this increased volume undergoes redistribution, potentially promoting stasis in certain areas.
- Endothelial Activation: The placental separation process releases tissue factors that activate the coagulation cascade.
- Inflammatory Response: The inflammatory processes associated with childbirth and tissue healing further promote a prothrombotic state.
- Delayed Mobilization: Limited mobility after delivery, especially following cesarean section, contributes significantly to venous stasis.
Thrombus Formation Process
The thrombus formation in postpartum thrombophlebitis follows this progression:
- Initial platelet adhesion and aggregation at the site of vascular injury or stasis
- Activation of the coagulation cascade
- Fibrin deposition forming the structural framework of the clot
- The size of the clot increases as circulating blood passes over it, depositing more platelets, fibrin, and cells
- Inflammatory response to the thrombus, with neutrophils and monocytes migrating to the site
- Vein wall inflammation (phlebitis) occurring in response to the thrombus or preceding it
This cascade of events can lead to partial or complete obstruction of venous blood flow, resulting in the characteristic symptoms and potential complications of postpartum thrombophlebitis.
Risk Factors
Multiple risk factors increase a woman’s susceptibility to developing postpartum thrombophlebitis. These can be categorized as pregnancy-specific factors, delivery-related factors, and pre-existing conditions.
| Category | Risk Factors |
|---|---|
| Pregnancy-Related |
|
| Delivery-Related |
|
| Pre-existing |
|
Clinical Insight
The risk of postpartum thrombophlebitis is highest during the first 3-6 weeks after delivery, with the peak incidence occurring in the second week postpartum. Risk assessment should be performed during pregnancy, upon admission for delivery, and before discharge to identify women who may benefit from prophylactic measures.
Risk stratification is essential for determining appropriate preventive measures. Women with multiple risk factors should receive targeted interventions, including early mobilization, mechanical prophylaxis, and, in some cases, pharmacological prophylaxis with anticoagulants during the postpartum period.
Clinical Manifestations
The symptoms and signs of postpartum thrombophlebitis vary depending on the type (superficial venous thrombosis, deep vein thrombosis, or septic pelvic thrombophlebitis) and the specific veins affected. Recognizing these manifestations is crucial for early diagnosis and intervention.
Superficial Venous Thrombosis (SVT)
- Pain and tenderness along the course of the affected vein
- Visible, palpable cord-like structure representing the thrombosed vein
- Localized redness (erythema) over the affected area
- Warmth when touching the area
- Mild edema around the affected vein
- Increased pain when ambulating or bearing weight
- Usually affects the saphenous vein of the lower leg
- Generally without systemic symptoms like fever or chills
Deep Vein Thrombosis (DVT)
- Unilateral leg swelling (edema)
- Pain and tenderness, particularly in the calf or thigh
- Skin discoloration – may appear pale or cyanotic
- Warmth over the affected area
- Dilated superficial veins (collateral circulation)
- Positive Homan’s sign (pain in the calf upon dorsiflexion of the foot) in some cases, though this sign is no longer considered reliable for diagnosis
- Leg heaviness or fatigue
- About 50% of cases are asymptomatic, making detection challenging
- Severity of symptoms correlates with the extent and location of thrombosis:
- Calf vein involvement: minimal or no edema
- Femoral vein involvement: mild to moderate edema
- Iliofemoral vein thrombosis: severe edema
Septic Pelvic Thrombophlebitis (SPT)
- Persistent fever (often spiking) despite antibiotic therapy
- Lower abdominal pain, often unilateral
- Pelvic pain or tenderness
- Tachycardia out of proportion to fever
- Occasionally a palpable mass in the lower abdomen
- Malodorous lochia (vaginal discharge)
- May have minimal or no physical findings despite significant symptoms
- Often follows endometritis or chorioamnionitis
Warning Signs of Pulmonary Embolism
Since pulmonary embolism is a potential life-threatening complication of DVT, nurses must recognize these warning signs that require immediate intervention:
- Sudden onset of shortness of breath
- Sharp chest pain that worsens with deep breathing
- Rapid or irregular heartbeat
- Hemoptysis (coughing up blood)
- Anxiety or sense of impending doom
- Lightheadedness or syncope
- Cyanosis (bluish discoloration of lips or extremities)
Differentiating SVT from DVT
Clinical differentiation between superficial and deep venous involvement is important for determining treatment approaches:
- SVT typically presents with visible, palpable veins and localized symptoms
- DVT often has more diffuse swelling and may not have visible external signs
- SVT tends to have more pronounced redness and inflammation over the affected area
- DVT may present with pallor or cyanosis rather than erythema
- Pain in SVT is typically more localized and superficial
It’s important to note that clinical assessment alone is not sufficient for definitive diagnosis, and diagnostic imaging is required to confirm suspicion of postpartum thrombophlebitis.
Diagnostic Procedures
Accurate diagnosis of postpartum thrombophlebitis requires a combination of clinical evaluation and objective diagnostic testing. Early and precise diagnosis is essential for appropriate management and prevention of complications.
Initial Clinical Assessment
- Comprehensive history: Assessing risk factors, symptom onset, and progression
- Physical examination: Evaluating for signs of inflammation, swelling, tenderness, and Homan’s sign (although not reliable as a single diagnostic indicator)
- Clinical prediction rules: Using tools like the Wells score to stratify risk and guide further testing
Laboratory Studies
- D-dimer test: Elevated in the presence of blood clots, though often naturally elevated during pregnancy and postpartum
- High sensitivity but low specificity in the postpartum period
- Normal result can help rule out DVT in low-risk patients
- Complete blood count (CBC)
- May show leukocytosis in septic thrombophlebitis
- Evaluate for anemia, which can exacerbate symptoms
- Coagulation profile
- Prothrombin time (PT)
- Activated partial thromboplastin time (aPTT)
- International normalized ratio (INR)
- Blood cultures: Important in suspected septic pelvic thrombophlebitis
- Thrombophilia testing: May be considered if there is a personal or family history suggestive of a hypercoagulable state
- Factor V Leiden mutation
- Prothrombin gene mutation
- Protein C, Protein S deficiency
- Antithrombin deficiency
- Antiphospholipid antibodies
Imaging Studies
Compression Ultrasound with Doppler
First-line imaging test for suspected DVT
- Non-invasive and safe during postpartum period
- High sensitivity (95%) and specificity (96%) for proximal DVT
- Less accurate for isolated calf vein thrombosis and pelvic veins
- Evaluates vein compressibility and blood flow
CT Venography
For suspected pelvic vein thrombosis
- More effective for visualizing iliac veins and IVC
- Useful when ultrasound results are inconclusive
- Requires contrast administration
- Provides detailed anatomical information
MR Venography
Alternative when other methods are contraindicated
- No radiation exposure
- Excellent for pelvic and iliac vein visualization
- Higher cost and limited availability
- Safe during lactation with gadolinium contrast
Additional Diagnostic Studies
- Contrast Venography: Historically the gold standard but now rarely used due to its invasive nature and availability of other techniques
- CT Pulmonary Angiography: For suspected pulmonary embolism, a potential complication of DVT
- Ventilation-Perfusion (V/Q) Scan: Alternative for pulmonary embolism diagnosis when CT angiography is contraindicated
Diagnostic Algorithm for Postpartum Thrombophlebitis
- Clinical assessment and risk stratification
- D-dimer testing (with appropriate threshold adjustments for postpartum state)
- Compression ultrasound for suspected lower extremity DVT
- CT or MR venography for suspected pelvic vein thrombosis
- Additional imaging for suspected complications
Diagnostic Challenges
Diagnosis of postpartum thrombophlebitis presents unique challenges:
- D-dimer levels are physiologically elevated during pregnancy and the postpartum period
- Symptoms may overlap with normal postpartum changes
- Septic pelvic thrombophlebitis may have minimal physical findings
- Balancing the need for accurate diagnosis with concerns about radiation exposure during lactation
Accurate and timely diagnosis is essential for implementing appropriate treatment and preventing potentially life-threatening complications like pulmonary embolism.
Management
The management of postpartum thrombophlebitis involves both pharmacological and non-pharmacological approaches, tailored to the type and severity of thrombophlebitis. Treatment aims to prevent clot progression, reduce inflammation, alleviate symptoms, and prevent complications.
Pharmacological Management
| Medication Class | Examples | Indications | Nursing Considerations |
|---|---|---|---|
| Anticoagulants |
|
|
|
| Nonsteroidal Anti-inflammatory Drugs (NSAIDs) |
|
|
|
| Antibiotics |
|
|
|
| Analgesics |
|
|
|
Treatment Duration
- Superficial Thrombophlebitis: 1-2 weeks of NSAIDs; anticoagulation may be prescribed for 4-6 weeks if extensive
- Deep Vein Thrombosis: Minimum 3 months of anticoagulation; typically 6-12 weeks postpartum
- Septic Pelvic Thrombophlebitis: 7-10 days of antibiotics plus anticoagulation for 7-14 days or until clinical improvement
Non-Pharmacological Management
Rest and Positioning
- Leg elevation above heart level when sitting or lying down
- Bed rest during acute phase, particularly for DVT
- Gradual resumption of activities as symptoms improve
- Avoidance of prolonged sitting or standing
Compression Therapy
- Graduated compression stockings (20-30 mmHg)
- Proper fitting is essential to avoid tourniquet effect
- Apply before rising in the morning
- Sequential compression devices during hospitalization
Warm Compresses
- Application of moist heat to affected area
- Helps reduce inflammation and discomfort
- Apply for 15-20 minutes several times daily
- Ensure appropriate temperature to prevent burns
Additional Interventions
- Early Mobilization: Encourage gentle movement and progressive ambulation as tolerated
- Adequate Hydration: Maintain fluid intake of at least 2500ml daily unless contraindicated
- Breathing Exercises: Deep breathing exercises to improve venous return
- IVC Filter Placement: Considered in cases of recurrent thromboembolism despite anticoagulation or when anticoagulation is contraindicated
- Surgical Interventions: Rarely indicated except in cases of massive iliofemoral DVT or phlegmasia cerulea dolens
Clinical Insight: Treatment of Septic Pelvic Thrombophlebitis
Septic pelvic thrombophlebitis typically requires a two-pronged approach:
- Broad-spectrum antibiotics to address the infectious component
- Anticoagulation to manage the thrombotic component
Persistent fever despite antibiotic therapy is a hallmark sign suggesting the need for anticoagulation. Clinical improvement typically occurs within 48-72 hours after initiating anticoagulation.
Breastfeeding Considerations
Most medications used to treat postpartum thrombophlebitis are compatible with breastfeeding:
- Heparins (both unfractionated and low molecular weight) do not pass into breast milk due to their high molecular weight
- Warfarin is considered safe during breastfeeding as minimal amounts enter breast milk
- Most NSAIDs are compatible with breastfeeding
- DOACs are generally not recommended during breastfeeding due to limited safety data
Management should be individualized based on the type and severity of thrombophlebitis, patient risk factors, and breastfeeding status. A multidisciplinary approach involving obstetricians, hematologists, and nursing staff optimizes outcomes in postpartum thrombophlebitis.
Nursing Care Plans
Comprehensive nursing care for postpartum thrombophlebitis involves systematic assessment, planning, implementation, and evaluation. The following nursing care plans address the primary concerns for patients with this condition.
Priority Nursing Diagnoses
- Impaired Tissue Perfusion related to venous stasis and thrombus formation
- Acute Pain related to inflammation and vascular congestion
- Risk for Injury related to potential complications (pulmonary embolism, septicemia)
- Anxiety related to uncertain prognosis and impact on postpartum experience
- Deficient Knowledge regarding condition, treatment, and self-care measures
- Risk for Ineffective Breastfeeding related to maternal illness and medication concerns
- Impaired Physical Mobility related to pain and prescribed activity restrictions
Nursing Care Plan 1: Impaired Tissue Perfusion
Goal: The patient will demonstrate improved tissue perfusion as evidenced by decreased edema, normal skin color, and palpable pulses.
Nursing Interventions:
- Assessment
- Assess affected extremity for color changes, temperature, edema, and pulses q4h
- Measure and record circumference of affected limb daily
- Monitor capillary refill time
- Interventions
- Elevate affected extremity above heart level when sitting or lying down
- Apply prescribed graduated compression stockings correctly
- Facilitate and document early, progressive ambulation as prescribed
- Administer anticoagulants as ordered and monitor for therapeutic effect
- Ensure adequate hydration (2500 ml/day unless contraindicated)
- Instruct on active ankle and foot exercises when on bed rest
- Avoid placing pillows under knees or sharp knee flexion
- Evaluation
- Patient demonstrates reduced edema in affected extremity
- Skin color and temperature return to normal
- Patient reports decreased discomfort in affected area
Nursing Care Plan 2: Acute Pain
Goal: The patient will report pain at a tolerable level (less than 3/10) and demonstrate effective pain management strategies.
Nursing Interventions:
- Assessment
- Assess pain characteristics using a standardized scale (0-10)
- Note location, quality, radiation, aggravating/alleviating factors
- Evaluate effectiveness of pain management strategies
- Interventions
- Administer prescribed analgesics and NSAIDs according to schedule
- Apply warm, moist compresses to affected area for 15-20 minutes q4h
- Position for comfort with affected limb elevated
- Provide gentle support for affected area using pillows or folded blankets
- Use a bed cradle to keep linens off sensitive areas
- Teach distraction techniques and relaxation exercises
- Document pain levels before and after interventions
- Evaluation
- Patient reports pain level at or below 3/10
- Patient demonstrates use of non-pharmacological pain management techniques
- Patient maintains adequate rest and comfort
Nursing Care Plan 3: Risk for Injury
Goal: The patient will not experience complications such as pulmonary embolism, extension of thrombosis, or septicemia.
Nursing Interventions:
- Assessment
- Monitor vital signs, especially respiratory rate and heart rate, q4h
- Assess for signs of pulmonary embolism: sudden dyspnea, chest pain, tachypnea
- Monitor for signs of sepsis: fever, chills, hypotension
- Observe for extension of thrombosis: increasing pain, edema, or discoloration
- Interventions
- Administer anticoagulant therapy as prescribed and monitor for effectiveness
- Instruct patient to avoid massaging affected area
- Monitor laboratory values (coagulation studies, CBC) as ordered
- Assess for bleeding (common sites: gums, nose, urine, stool) during anticoagulant therapy
- Maintain oxygen therapy if prescribed
- Instruct in deep breathing exercises q2h while awake
- Facilitate gradual, progressive ambulation as tolerated
- Implement fall precautions during anticoagulant therapy
- Evaluation
- Patient maintains stable respiratory status and vital signs
- Patient demonstrates no signs of complications
- Laboratory values remain within therapeutic range
Nursing Care Plan 4: Deficient Knowledge
Goal: The patient will verbalize understanding of condition, treatment plan, medication regimen, and signs/symptoms requiring medical attention.
Nursing Interventions:
- Assessment
- Assess baseline knowledge of thrombophlebitis and its treatment
- Identify learning needs and preferred learning style
- Evaluate literacy level and potential barriers to understanding
- Interventions
- Provide education about:
- Nature of thrombophlebitis and its causes
- Medication purpose, dosage, administration, and side effects
- Importance of compliance with treatment plan
- Proper application of compression stockings
- Activity restrictions and progressive resumption
- Warning signs requiring immediate attention
- Safety considerations with anticoagulant therapy
- Follow-up care requirements
- Provide written materials to reinforce verbal instruction
- Demonstrate self-injection technique if LMWH prescribed
- Use teach-back method to verify understanding
- Provide education about:
- Evaluation
- Patient verbalizes understanding of condition and treatment
- Patient correctly demonstrates self-care techniques
- Patient identifies warning signs requiring medical attention
- Patient verbalizes plan for follow-up care
Special Considerations for Postpartum Patients
- Maternal-Infant Bonding: Facilitate bonding despite activity restrictions by positioning infant safely near mother
- Breastfeeding Support: Assist with breastfeeding positioning that doesn’t compromise affected extremity
- Postpartum Recovery: Continue to monitor typical postpartum recovery needs alongside thrombophlebitis management
- Emotional Support: Address potential feelings of disappointment, frustration, or anxiety related to complicated postpartum experience
- Family Education: Include support persons in education to assist patient at home
Documentation Focus
Thorough documentation should include:
- Assessment findings including limb measurements and pain scores
- Interventions implemented and patient’s response
- Medication administration and effectiveness
- Patient education provided and understood
- Progress toward goals and any changes to care plan
- Coordination with interdisciplinary team
Prevention Strategies
Preventing postpartum thrombophlebitis involves identifying at-risk women and implementing appropriate prophylactic measures. A systematic approach to prevention can significantly reduce the incidence of this potentially serious complication.
Risk Assessment
- Antenatal Screening: Assess risk factors throughout pregnancy
- Peripartum Assessment: Reassess risk upon admission for delivery
- Postpartum Evaluation: Perform final risk assessment before discharge
- Scoring Systems: Use validated VTE risk assessment tools to stratify risk
Preventive Measures Based on Risk Stratification
| Risk Level | Preventive Interventions |
|---|---|
| Low Risk (No risk factors) |
|
| Moderate Risk (1-2 risk factors) |
|
| High Risk (≥3 risk factors, previous VTE, thrombophilia) |
|
Mechanical Prophylaxis
- Early Ambulation: Encourage getting out of bed and walking as soon as possible after delivery
- Graduated Compression Stockings: Properly fitted stockings providing 20-30 mmHg pressure
- Sequential Compression Devices: Particularly beneficial during cesarean delivery and immediate postpartum period
- Proper Positioning: Avoid prolonged periods with legs in dependent position
- Leg Exercises: Ankle pumps, calf stretches, and other exercises when mobility is limited
Pharmacological Prophylaxis
- Low Molecular Weight Heparin (LMWH): Preferred agent for postpartum prophylaxis
- Dosage typically based on patient weight
- Administered subcutaneously once daily
- Duration depends on risk assessment (7 days to 6 weeks)
- Unfractionated Heparin (UFH): Alternative when LMWH is unavailable or contraindicated
- Timing of Initiation: Usually 6-12 hours after vaginal delivery, 12-24 hours after cesarean delivery
Nursing Tip
When teaching patients about self-administration of LMWH injections, emphasize:
- Proper injection technique into abdominal subcutaneous tissue
- Rotating injection sites
- Proper disposal of needles
- Signs of complications to report
Patient Education for Prevention
- Warning Signs: Teach recognition of early symptoms (leg pain, swelling, warmth)
- Lifestyle Modifications:
- Avoid prolonged sitting or standing
- Elevate legs when resting
- Stay adequately hydrated
- Avoid crossing legs
- Stop smoking
- Activity Guidelines: Encourage regular, appropriate physical activity
- Compression Stocking Use: Proper application, duration of use, and care
Nursing Role in Prevention
- Risk Assessment: Conduct thorough evaluations to identify at-risk patients
- Implementation: Ensure prescribed preventive measures are correctly applied
- Monitoring: Observe for early signs of thrombophlebitis
- Education: Provide comprehensive patient and family teaching
- Documentation: Record risk assessments, preventive measures, and patient response
- Advocacy: Ensure appropriate prophylaxis based on risk stratification
Important Considerations
Special attention to prevention should be given in the following scenarios:
- After cesarean delivery
- Following postpartum hemorrhage
- During prolonged bed rest
- Women with pre-existing thrombophilia
- History of previous VTE
- Multiple risk factors
Effective prevention relies on systematic risk assessment, timely implementation of appropriate preventive measures, ongoing monitoring, and comprehensive patient education. By identifying at-risk individuals and providing targeted prophylaxis, the incidence of postpartum thrombophlebitis can be significantly reduced.
Complications
Despite appropriate management, postpartum thrombophlebitis can lead to several serious complications. Early recognition and intervention are essential to prevent these potentially life-threatening sequelae.
Major Complications
Pulmonary Embolism (PE)
The most serious and potentially fatal complication of DVT, occurring when a blood clot breaks free and travels to the lungs.
Warning Signs:
- Sudden shortness of breath
- Sharp chest pain, especially during breathing
- Rapid heart rate
- Hemoptysis (coughing up blood)
- Anxiety or sense of impending doom
- Hypoxemia and decreased oxygen saturation
If untreated, pulmonary embolism can cause sudden death. The incidence of pulmonary embolism is approximately 24% in untreated postpartum DVT cases, with a fatality rate of 15%.
Septicemia
A potential complication of septic pelvic thrombophlebitis, characterized by bacteria entering the bloodstream.
Warning Signs:
- High fever with chills
- Rapid breathing and heart rate
- Hypotension
- Altered mental status
- Decreased urine output
- Severe malaise
Can progress to septic shock, multiorgan failure, and death if not promptly treated.
Post-Thrombotic Syndrome (PTS)
A long-term complication occurring in 20-50% of patients with DVT, characterized by chronic venous insufficiency.
Manifestations:
- Chronic leg pain
- Persistent edema
- Skin changes (hyperpigmentation, eczema)
- Venous ulcers
- Varicose veins
- Leg heaviness and fatigue
Development may begin within months of DVT and persist for years or indefinitely.
Other Complications
- Recurrent Thrombosis: Increased risk for future thrombotic events
- Women with postpartum thrombophlebitis have a higher lifetime risk of recurrent VTE
- Risk particularly elevated during subsequent pregnancies
- May require prophylactic anticoagulation in future high-risk situations
- Chronic Venous Insufficiency: Long-term venous damage
- Valvular incompetence leading to venous reflux
- Persistent edema and discomfort
- May require long-term use of compression therapy
- Phlegmasia Cerulea Dolens: Rare but severe complication
- Massive iliofemoral DVT causing severe venous obstruction
- Presents with painful, swollen, cyanotic limb
- Can lead to venous gangrene if untreated
- Requires urgent intervention, possibly including thrombolysis
- Bleeding Complications: Related to anticoagulant therapy
- Increased risk of postpartum hemorrhage with early anticoagulation
- Potential for intracranial hemorrhage
- Gastrointestinal bleeding
- Wound hematomas after cesarean delivery
- Psychological Impact: Mental health consequences
- Anxiety about future health and recurrence
- Depression related to chronic symptoms
- Disruption to maternal-infant bonding
- Postpartum period complications affecting transition to motherhood
Long-Term Management After Complications
- Extended Anticoagulation: May be necessary for recurrent events or thrombophilia
- Chronic Disease Management: For post-thrombotic syndrome
- Lifelong compression therapy
- Regular follow-up with vascular specialists
- Skin care to prevent ulceration
- Psychological Support: Counseling for women experiencing anxiety or depression
- Preconceptional Counseling: For future pregnancy planning
- Risk assessment
- Prophylaxis planning
- Close monitoring during subsequent pregnancies
Warning Signs Requiring Immediate Medical Attention
Nurses should educate patients to seek immediate medical care if they experience:
- Sudden shortness of breath or chest pain
- Coughing up blood
- Severe, increasing, or spreading pain in affected limb
- Significant increase in swelling
- Limb becoming pale, blue, or cold
- High fever with chills
- Unusual bleeding or bruising while on anticoagulants
Vigilant monitoring for complications and prompt intervention can significantly reduce morbidity and mortality associated with postpartum thrombophlebitis. Patient education about warning signs and the importance of adherence to treatment regimens is crucial to preventing these serious complications.
