Neonatal Care Protocols
Comprehensive Guide to Levels of Care and Infection Control
Introduction to Neonatal Care
Neonatal care protocols are systematic approaches to providing quality healthcare to newborn infants, especially those requiring intensive medical attention due to premature birth, low birth weight, or other medical complications. These protocols encompass a range of practices, from basic newborn care to highly specialized interventions in neonatal intensive care units.
This comprehensive guide addresses the essential components of neonatal care protocols, including structured levels of care and rigorous infection control measures. Understanding these protocols is crucial for nursing professionals working in neonatal units to provide optimal care and improve outcomes for vulnerable newborns.
Key Focus Areas
- Levels of neonatal care classification
- Evidence-based infection control practices
- Standardized protocols for consistent care
Table of Contents
Overview of Neonatal Care
Neonatal care protocols form the backbone of effective care delivery in newborn and infant healthcare settings. These protocols are developed based on evidence-based practices and are designed to standardize care, minimize errors, and improve outcomes for newborns requiring medical intervention.
The neonatal period, defined as the first 28 days of life, is a critical time when infants are most vulnerable and require specialized care tailored to their unique physiological needs. Neonatal care protocols address this vulnerability by providing structured approaches to assessment, intervention, and ongoing management.
Key Components of Neonatal Care
- Physical assessment and vital signs monitoring
- Respiratory support and management
- Thermoregulation
- Nutrition and feeding support
- Infection prevention and control
- Medication administration
- Family-centered care approaches
- Development assessment and support
The implementation of standardized neonatal care protocols has been shown to significantly reduce mortality and morbidity rates among newborns. These protocols are particularly important when managing premature infants, who face numerous physiological challenges including immature organ systems, temperature regulation difficulties, feeding problems, and increased susceptibility to infections.

Illustration of a neonatal care unit showing different levels of care and equipment.
Levels of Neonatal Care
Neonatal care protocols are organized according to four distinct levels of care, as defined by the American Academy of Pediatrics. These levels reflect the complexity of care required and the resources available at different healthcare facilities. Understanding these levels is crucial for nursing professionals to ensure appropriate care delivery and timely referrals when necessary.
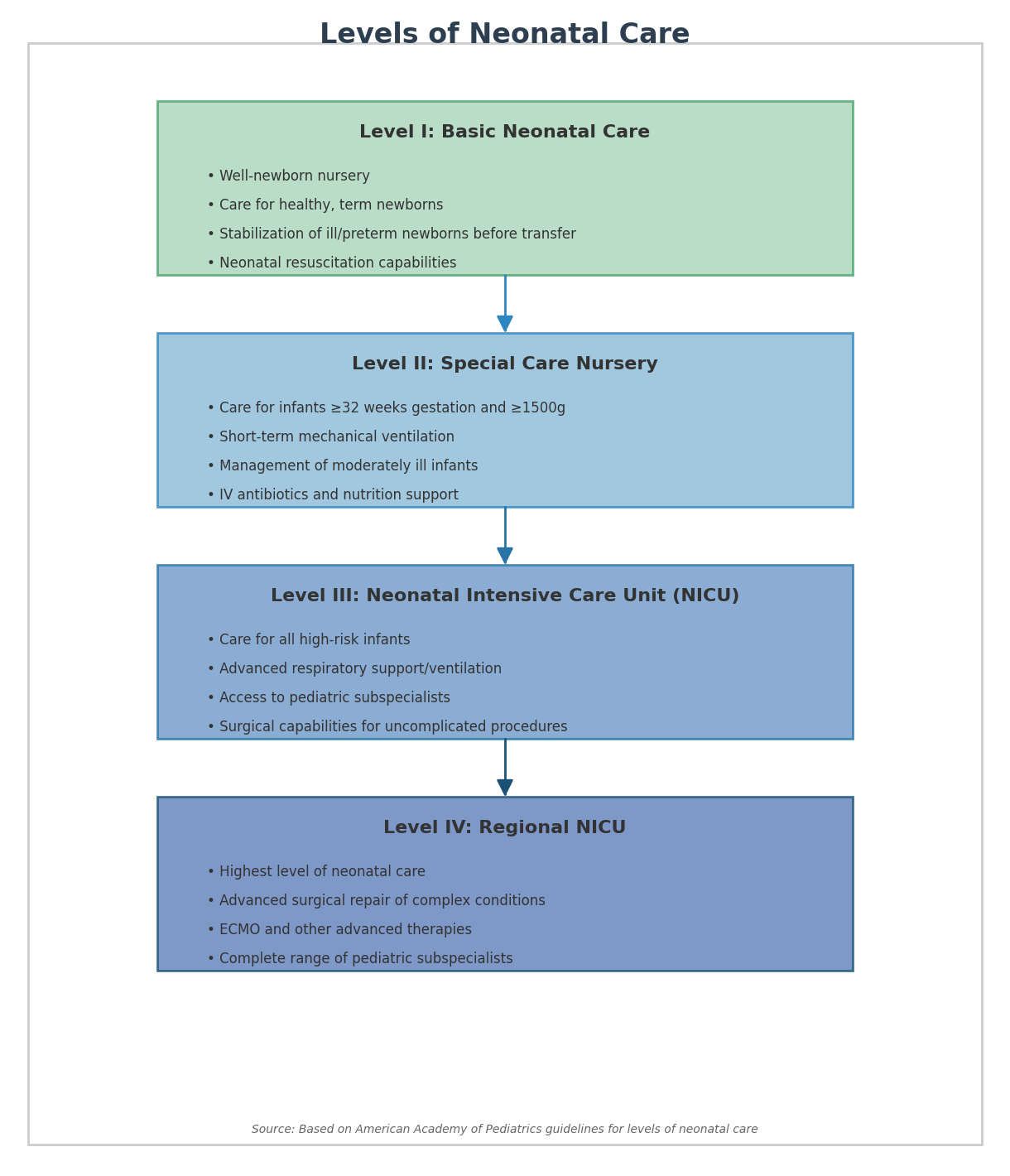
Flow chart of the four levels of neonatal care and their key characteristics.
Level I: Basic Neonatal Care
Level I nurseries, also known as well-newborn nurseries, provide basic care to healthy newborns. These facilities are equipped to:
- Provide care for healthy, term infants (≥37 weeks gestation)
- Perform neonatal resuscitation at every delivery
- Evaluate and provide postnatal care to stable term newborns
- Stabilize ill newborn infants or those born preterm until transfer to a higher level of care
- Facilitate transport to higher-level facilities when needed
Level I facilities implement neonatal care protocols focused on routine care, including temperature maintenance, feeding support, newborn screening, and early detection of complications requiring referral.
Nursing Responsibilities in Level I Care
- Regular assessment of vital signs and physical condition
- Support for breastfeeding initiation
- Parent education on newborn care
- Recognition of warning signs requiring escalation of care
Level II: Special Care Nursery
Level II units, or special care nurseries, provide care for moderately ill infants who are expected to recover quickly and those who are convalescing after intensive care. These facilities:
- Care for infants born at ≥32 weeks gestation and weighing ≥1500g
- Provide care for infants with physiologic immaturity (feeding difficulties, temperature instability)
- Can provide continuous positive airway pressure (CPAP)
- May provide mechanical ventilation for brief durations (up to 24-48 hours)
- Administer intravenous nutrition and medications
Neonatal care protocols in Level II units focus on managing common prematurity issues, feeding difficulties, and mild respiratory distress while maintaining close communication with higher-level facilities for potential transfers.
Special Care Nursery Equipment
Monitoring
- Cardiorespiratory monitors
- Pulse oximeters
- Blood pressure equipment
Respiratory
- CPAP devices
- Oxygen blenders
- Limited ventilator support
Nutrition
- Feeding pumps
- IV infusion equipment
- Specialized feeding tools
Level III: Neonatal Intensive Care Unit (NICU)
Level III NICUs provide comprehensive care for critically ill newborns requiring continuous life support and monitoring. These units:
- Care for infants born at <32 weeks gestation and weighing <1500g
- Provide sustained life support with advanced respiratory support modalities
- Offer advanced imaging capabilities (CT, MRI)
- Have access to pediatric medical subspecialists
- Can perform minor surgical procedures
- Provide comprehensive management of critical medical and surgical conditions
Level III neonatal care protocols are highly specialized and address complex medical conditions including respiratory distress syndrome, severe infections, and neurological conditions. These protocols integrate multidisciplinary approaches involving neonatologists, specialized nurses, respiratory therapists, and other specialists.
Critical Aspects of Level III Care
Respiratory Management
Level III units employ sophisticated ventilation strategies including high-frequency ventilation, nitric oxide therapy, and surfactant administration for neonates with severe respiratory compromise.
Nutritional Support
Comprehensive parenteral nutrition formulations, specialized enteral feeding protocols, and close monitoring of growth parameters are standard practice.
Neurological Monitoring
Continuous EEG monitoring, brain cooling for hypoxic-ischemic encephalopathy, and neurodevelopmental follow-up programs are available.
Infection Control
Rigorous infection prevention protocols, antibiotic stewardship programs, and dedicated isolation capabilities for infectious disease management.
Level IV: Regional NICU
Level IV NICUs represent the highest level of neonatal care, located in major tertiary care or academic centers. These facilities:
- Provide all Level III capabilities plus additional advanced care
- Perform complex surgical repairs of congenital or acquired conditions
- Maintain advanced respiratory support including extracorporeal membrane oxygenation (ECMO)
- Offer specialized transport services and outreach education
- Have access to all pediatric subspecialists 24/7
- Conduct clinical research and implement new therapies
Level IV neonatal care protocols represent the most advanced approaches in neonatal medicine and often serve as the basis for developing new protocols that may eventually be implemented at other levels of care.
Level IV Specialized Capabilities
Surgical Interventions
- Complex cardiac surgery
- Repair of congenital anomalies
- Neurosurgical procedures
Advanced Therapies
- ECMO services
- Therapeutic hypothermia
- Experimental treatments
Core Neonatal Care Protocols
Neonatal care protocols provide standardized approaches to common clinical scenarios and are essential for maintaining consistency in care delivery. These protocols are based on evidence-based practices and are regularly updated to reflect advances in neonatal medicine.
Neonatal Assessment
Comprehensive assessment protocols guide the evaluation of newborns from delivery through the neonatal period.
Key Components:
- Initial assessment: APGAR scoring at 1 and 5 minutes
- Physical examination: Systematic head-to-toe assessment
- Vital signs monitoring: Temperature, heart rate, respiratory rate, blood pressure, oxygen saturation
- Neurobehavioral assessment: Reflexes, tone, state regulation
Respiratory Support
Protocols for respiratory management are critical in neonatal care, particularly for premature infants with underdeveloped lungs.
Support Modalities:
- Oxygen therapy: Guidelines for administration and monitoring
- CPAP: Indications, setup, and management
- Mechanical ventilation: Parameter settings, weaning protocols
- Surfactant administration: Indications, techniques, and monitoring
Nutrition and Feeding
Nutritional support protocols aim to promote growth and development while considering the unique digestive capabilities of neonates.
Feeding Approaches:
- Breastfeeding support: Techniques, assessment, and support measures
- Enteral feeding: Advancement schedules, fortification guidelines
- Parenteral nutrition: Composition, monitoring, and complications
- Growth monitoring: Assessment tools, growth charts, and interventions
Protocol Implementation Best Practices
Protocol Development
- Base protocols on current evidence and guidelines
- Include multidisciplinary input
- Consider facility resources and capabilities
- Create clear, concise documentation
Protocol Maintenance
- Schedule regular reviews (at least annually)
- Track protocol adherence and outcomes
- Update based on new evidence or guidelines
- Provide staff education with each update
Protocol Standardization and Customization
While standardization of neonatal care protocols is essential for consistency, protocols must also allow for individualized care based on each infant’s specific needs and responses to interventions.
Standardization Benefits
- ✓ Reduces practice variation
- ✓ Improves care consistency
- ✓ Facilitates staff training
- ✓ Improves measurable outcomes
- ✓ Enhances communication
Customization Considerations
- ✓ Individual patient factors
- ✓ Family preferences and culture
- ✓ Resource availability
- ✓ Response to interventions
- ✓ Comorbid conditions
Infection Control in Neonatal Care
Infection control is a critical component of neonatal care protocols, as newborns—especially premature infants—have immature immune systems that increase their susceptibility to infections. Healthcare-associated infections (HAIs) can lead to significant morbidity, prolonged hospital stays, and increased mortality in the neonatal population.
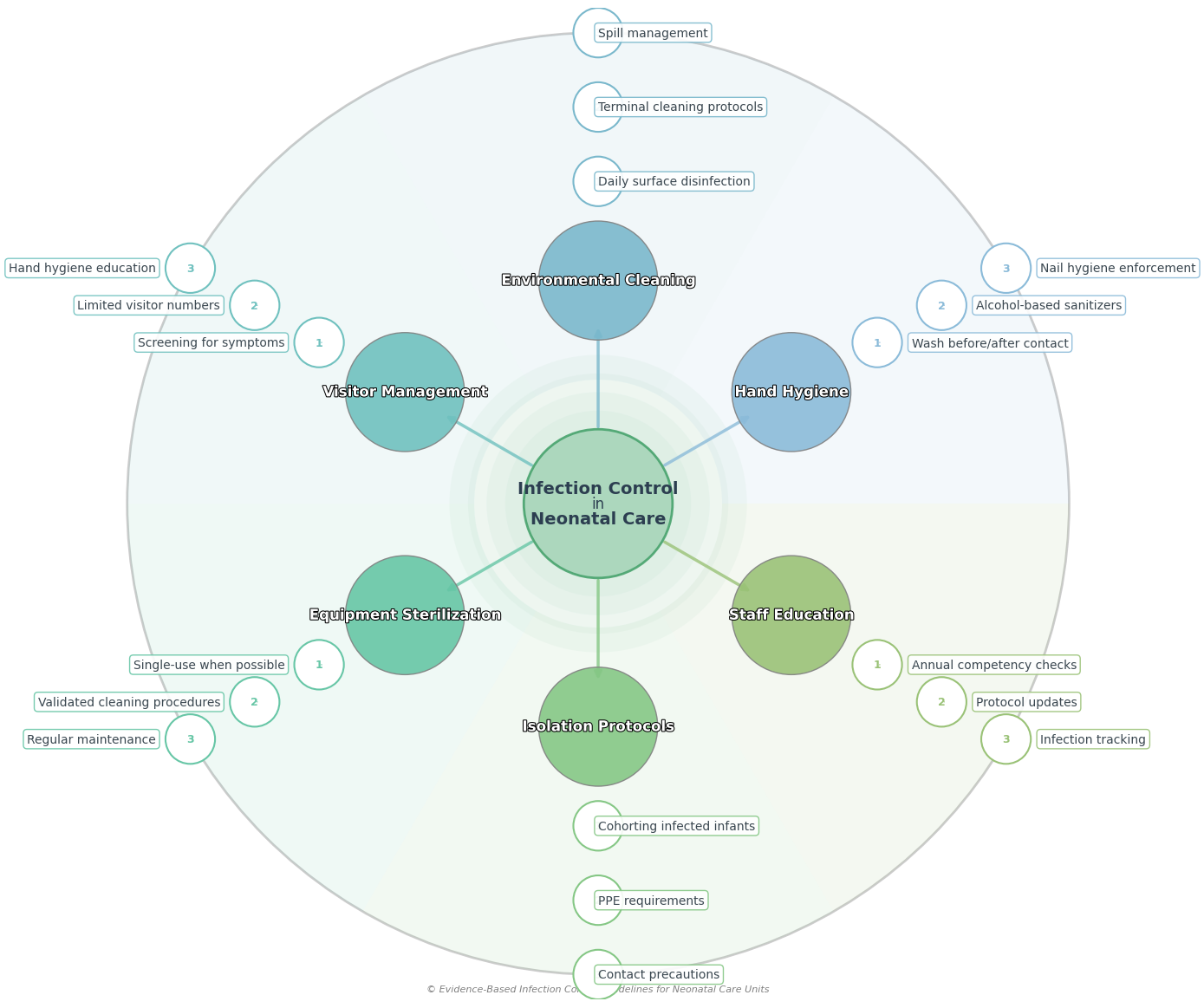
Comprehensive framework of infection control measures in neonatal care units.
Effective infection prevention and control in neonatal units requires a multifaceted approach involving healthcare staff, visitors, and the environment. The following sections detail key components of infection control neonatal care protocols.
Hand Hygiene
Hand hygiene is the single most important measure for preventing healthcare-associated infections in neonatal units. Neonatal care protocols emphasize strict adherence to hand hygiene practices for all staff and visitors.
Key Protocol Components:
- 5 Moments for Hand Hygiene: Before patient contact, before aseptic procedures, after body fluid exposure, after patient contact, and after contact with patient surroundings
- Proper Handwashing Technique: Using soap and water for visibly soiled hands with a minimum duration of 40-60 seconds
- Alcohol-based Hand Rub (ABHR): For routine hand decontamination when hands are not visibly soiled, with a minimum duration of 20-30 seconds
- Nail Hygiene: Keeping nails short, avoiding artificial nails and nail polish
Implementation Strategies:
- • Strategically placed hand hygiene stations throughout the unit
- • Regular hand hygiene audits with performance feedback
- • Visual reminders and educational materials
- • Designation of hand hygiene champions among staff
Environmental Cleaning
Environmental surfaces and equipment in neonatal units can serve as reservoirs for pathogens. Comprehensive neonatal care protocols include detailed cleaning and disinfection procedures to minimize this risk.
Routine Cleaning
- Frequency: Daily cleaning of all horizontal surfaces and frequently touched objects
- Products: Hospital-grade disinfectants approved for use in neonatal areas
- High-touch surfaces: Incubator/warmer controls, monitors, doorknobs, sink handles
Terminal Cleaning
- Timing: After patient discharge or transfer
- Process: Thorough cleaning and disinfection of all surfaces and equipment
- Verification: Cleaning checklist and visual inspection
Specialized Environmental Controls:
- Water Management: Regular testing of water systems and ice machines to prevent waterborne infections
- Ventilation Systems: Maintenance of appropriate air exchanges and filtration
- Waste Management: Proper segregation and disposal of different waste categories
Visitor Management
Family-centered care is important in neonatal units, but visitor policies must balance family involvement with infection control considerations. Neonatal care protocols should include clear visitor guidelines.
Core Visitor Protocol Components:
- Screening: All visitors should be screened for symptoms of communicable diseases (respiratory symptoms, rashes, recent exposures)
- Numbers: Limit visitors to parents/guardians and designated support persons
- Hand Hygiene Education: Instruction on proper hand hygiene techniques for all visitors
- Personal Protective Equipment (PPE): Providing appropriate PPE as indicated
Special Considerations:
Sibling Visits: Many units allow sibling visits with additional screening for childhood illnesses and education appropriate to the child’s age.
Outbreak Situations: Visitor restrictions may be temporarily enhanced during outbreaks of communicable diseases in the facility or community.
Virtual Visitation: When in-person visits are limited, virtual visitation options should be offered to maintain family connections.
Equipment Sterilization
Medical equipment used in neonatal care can transmit pathogens between patients if not properly cleaned, disinfected, or sterilized. Neonatal care protocols must include detailed procedures for equipment management.
Equipment Management Principles:
- Single-Use Items: Preference for single-use items whenever possible for high-risk procedures
- Reprocessing Guidelines: Following manufacturer instructions and evidence-based guidelines for cleaning, disinfection, and sterilization
- Equipment Rotation: Regular schedules for preventive maintenance and cleaning of equipment
| Equipment Category | Examples | Recommended Process |
|---|---|---|
| Non-critical items | Blood pressure cuffs, stethoscopes | Low to intermediate-level disinfection between patients |
| Semi-critical items | Respiratory equipment, laryngoscope blades | High-level disinfection or sterilization |
| Critical items | Surgical instruments, central line insertion kits | Sterilization required |
High-Risk Equipment Considerations:
Special attention should be given to equipment associated with healthcare-associated infections in neonates, including:
- • Ventilator circuits and humidifiers
- • Central line insertion and maintenance supplies
- • Breast milk pumps and collection kits
- • Incubators and radiant warmers
Isolation Protocols
Isolation measures are critical components of neonatal care protocols for preventing the spread of infectious agents among vulnerable neonates.
Types of Isolation Precautions
- Standard Precautions: Applied to all patients regardless of infection status
- Contact Precautions: For patients with known or suspected infections spread by direct or indirect contact
- Droplet Precautions: For patients with infections spread by large respiratory droplets
- Airborne Precautions: For patients with infections spread by small particles that remain suspended in the air
Implementation Strategies
- Cohorting: Grouping patients with the same pathogen together when private rooms are unavailable
- Dedicated Equipment: Assigning specific equipment to isolated patients
- Staff Assignment: Considering dedicated staff assignments for isolated patients
- Communication: Clear signage and communication about isolation status and required precautions
Common Pathogens Requiring Isolation in NICUs:
Bacterial
- • Methicillin-resistant S. aureus (MRSA)
- • Vancomycin-resistant enterococci (VRE)
- • Extended-spectrum beta-lactamase (ESBL) producing organisms
Viral
- • Respiratory syncytial virus (RSV)
- • Influenza
- • Herpes simplex virus
Fungal
- • Candida auris
- • Resistant Candida species
Staff Education
Ongoing education is essential for maintaining high standards of infection control in neonatal units. Staff education is a key component of comprehensive neonatal care protocols.
Staff Education Components:
- Orientation: Comprehensive infection control education for all new staff
- Recurring Training: Annual competency assessments and updates on infection control practices
- Feedback Mechanisms: Regular sharing of infection rate data and compliance with infection control measures
- Protocol Updates: Communication and education when protocols are updated based on new evidence
Infection Prevention Champions:
Designating infection prevention champions among nursing staff can enhance protocol implementation through:
- • Peer-to-peer education and coaching
- • Real-time feedback on infection control practices
- • Identification of barriers to protocol adherence
- • Participation in infection control committees
Integrated Approach to Infection Control
Effective infection control in neonatal units requires an integrated approach that combines multiple strategies. Neonatal care protocols should emphasize the interdependence of different infection control measures, as weakness in one area can compromise the entire system.
Regular surveillance of healthcare-associated infections, antimicrobial stewardship programs, and quality improvement initiatives are additional components that enhance the effectiveness of basic infection control measures in neonatal units.
Helpful Mnemonics for Neonatal Care
Mnemonics are valuable memory aids that can help nursing students remember complex neonatal care protocols and procedures. The following mnemonics address key aspects of neonatal care and infection control.
STABLE
Assessment and stabilization of the sick newborn
- S Sugar and Safe care: Maintain normal glucose levels
- T Temperature: Maintain normal temperature
- A Airway: Ensure airway patency
- B Blood pressure: Maintain normal blood pressure
- L Lab work: Obtain necessary laboratory studies
- E Emotional support: Support the family
ABCDEF
Neonatal assessment priorities
- A Airway: Assess airway patency and positioning
- B Breathing: Evaluate respiratory effort and effectiveness
- C Circulation: Assess heart rate, perfusion, and blood pressure
- D Disability: Check neurological status and tone
- E Exposure: Conduct complete physical examination while maintaining temperature
- F Family: Involve and support family members
HANDS-CLEAN
Infection control principles for neonatal care
- H Hand hygiene: Before and after every patient contact
- A Aseptic technique: For all invasive procedures
- N Never reuse single-use items: Dispose properly after use
- D Disinfect equipment: Between patient use
- S Separate clean and dirty items: Maintain workflow from clean to dirty
- C Clean environment: Regular cleaning of all surfaces
- L Limit visitors: Screen and educate all visitors
- E Educate staff and families: About infection control measures
- A Antibiotics stewardship: Use appropriately
- N Note and report: Signs of infection promptly
PROTOCOL
Key elements of effective neonatal care protocols
- P Practice based on evidence: Use current research findings
- R Regular updates: Review and revise protocols periodically
- O Organized approach: Logical flow and clear instructions
- T Team involvement: Input from all disciplines
- O Outcomes measured: Evaluate effectiveness
- C Clear communication: Accessible and understandable
- O Ongoing education: Train staff on protocol implementation
- L Level-appropriate: Match protocols to unit capabilities
Global Best Practices in Neonatal Care
Neonatal care protocols vary worldwide, with different regions developing innovative approaches based on their specific challenges and resources. Examining global best practices can provide valuable insights for enhancing neonatal care in any setting.
Kangaroo Mother Care
Origin: Colombia
Kangaroo Mother Care (KMC) involves skin-to-skin contact between the infant and parent, combined with exclusive breastfeeding and close follow-up. This approach has shown significant benefits for premature and low birth weight infants.
Key Benefits:
- • Improved thermoregulation
- • Better weight gain
- • Reduced infection rates
- • Enhanced bonding
- • Increased breastfeeding success
Bundle Approach
Origin: United Kingdom and United States
Care bundles are groups of evidence-based interventions that, when implemented together, significantly improve patient outcomes. This approach has been successfully applied to reduce central line-associated bloodstream infections (CLABSI) and ventilator-associated pneumonia (VAP) in NICUs.
Sample CLABSI Bundle:
- • Hand hygiene before line manipulation
- • Maximal barrier precautions during insertion
- • Chlorhexidine skin antisepsis
- • Daily review of line necessity
- • Standardized line care protocols
Family Integrated Care
Origin: Canada
Family Integrated Care (FICare) is a model that actively involves parents as primary caregivers for their hospitalized infant. Parents receive education and support to become competent and confident in providing care, working alongside healthcare professionals.
Program Elements:
- • Structured parent education program
- • Gradual transfer of care responsibilities
- • Parent participation in rounds
- • Peer-to-peer support
- • Modified staff roles to focus on teaching
Technological Innovations in Neonatal Care
Technology has significantly enhanced the implementation of neonatal care protocols worldwide, allowing for more precise monitoring, intervention, and documentation.
Telemedicine in Neonatal Care
Telemedicine connects smaller hospitals with tertiary care centers, allowing for remote consultation on complex cases. This approach has been particularly successful in:
- • Rural Japan’s perinatal telemedicine network
- • Australia’s outback telehealth services
- • United States’ tele-NICU programs
Electronic Protocol Systems
Computerized protocol systems improve adherence to neonatal care protocols through:
- • Decision support tools for medication dosing
- • Automated alerts for protocol deviations
- • Integrated documentation systems
- • Real-time monitoring of protocol compliance
References
- American Academy of Pediatrics Committee on Fetus and Newborn. (2012). Levels of neonatal care. Pediatrics, 130(3), 587-597.
- World Health Organization. (2015). WHO recommendations on interventions to improve preterm birth outcomes. Geneva: World Health Organization.
- Centers for Disease Control and Prevention. (2022). Infection prevention and control in neonatal intensive care units. Atlanta: CDC.
- O’Grady, N. P., Alexander, M., Burns, L. A., et al. (2011). Guidelines for the prevention of intravascular catheter-related infections. Clinical Infectious Diseases, 52(9), e162-e193.
- Polin, R. A., & Denson, S. (2012). Committee on Fetus and Newborn. Strategies for prevention of health care-associated infections in the NICU. Pediatrics, 129(4), e1085-e1093.
- Conde-Agudelo, A., & Díaz-Rossello, J. L. (2016). Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database of Systematic Reviews, (8), CD002771.
- O’Brien, K., Robson, K., Bracht, M., et al. (2018). Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. The Lancet Child & Adolescent Health, 2(4), 245-254.
- Payne, N. R., & Carpenter, J. H. (2018). Strategies to reduce nosocomial infections in the neonatal intensive care unit. Seminars in Perinatology, 42(1), 11-20.
- Dramowski, A., Whitelaw, A., & Cotton, M. F. (2017). Infection prevention and control in neonatal units in developing countries: Challenges and opportunities. Journal of Hospital Infection, 97(3), 285-294.
- Bowen, J. R., Callander, I., Richards, R., & Lindrea, K. B. (2017). Decreasing infection in neonatal intensive care units through quality improvement. Archives of Disease in Childhood-Fetal and Neonatal Edition, 102(1), F51-F57.
Continuous Learning in Neonatal Care
Neonatal care protocols continue to evolve as new evidence emerges. Nursing students and professionals should commit to ongoing education to stay current with best practices in this dynamic field.
- Follow updates from professional organizations
- Pursue specialized neonatal nursing certifications
- Participate in simulation-based training
- Engage in interprofessional learning opportunities
- Contribute to quality improvement initiatives
