Neonatal Infections: Comprehensive Guide for Nursing Students
A complete resource for understanding, identifying, preventing, and managing infections in newborns
Table of Contents
- 1. Introduction to Neonatal Infections
- 2. Classification of Neonatal Infections
- 3. Early-Onset vs Late-Onset Neonatal Infections
- 4. Bacterial Infections in Neonates
- 5. Viral Infections in Neonates
- 6. Fungal Infections in Neonates
- 7. Diagnosis of Neonatal Infections
- 8. Treatment Approaches
- 9. Nursing Care and Management
- 10. Prevention Strategies
- 11. Mnemonics and Learning Aids
- 12. Global Best Practices
- 13. References
1. Introduction to Neonatal Infections
Neonatal infections remain a significant cause of morbidity and mortality worldwide, particularly in developing countries. These infections affect approximately 1-5 per 1000 live births in developed countries and 3-20 per 1000 live births in developing countries.
Definition
Neonatal infections are defined as infections occurring during the neonatal period, which extends from birth to 28 days of life. These infections can be acquired before birth (congenital), during delivery (intrapartum), or after birth (postpartum).
The unique vulnerability of neonates to infections stems from several factors:
- Immature immune system: Neonates have underdeveloped innate and adaptive immune responses, making them susceptible to various pathogens.
- Fragile anatomical barriers: Thin skin, delicate mucous membranes, and immature gastrointestinal tract provide reduced protection against pathogen invasion.
- Exposure during birth: Passage through the birth canal exposes the neonate to maternal flora and potential pathogens.
- Limited microbiome development: The protective microbiome is underdeveloped, allowing easier colonization by pathogenic organisms.
- Invasive procedures: Hospitalized neonates often require invasive procedures that breach natural defensive barriers.
Understanding neonatal infections is crucial for nursing students as timely recognition, appropriate management, and preventive strategies can significantly reduce associated morbidity and mortality. This comprehensive guide aims to provide nursing students with essential knowledge about various types of neonatal infections, their diagnosis, treatment approaches, and prevention strategies.
2. Classification of Neonatal Infections
Neonatal infections can be classified based on several criteria, including timing of onset, causative pathogens, and site of infection. Understanding these classifications helps in determining potential causes, guiding diagnostic evaluations, and initiating appropriate treatment.
2.1 Classification Based on Timing
Timing-Based Classification:
- Congenital infections: Acquired before birth through transplacental transmission (e.g., TORCH infections)
- Early-onset infections: Present within the first 72 hours (or up to 7 days) of life
- Late-onset infections: Manifest after 72 hours (or 7 days) of life up to 28 days
- Very late-onset infections: Occur beyond 28 days of life, particularly in premature infants requiring extended hospitalization
2.2 Classification Based on Pathogens
Pathogen-Based Classification:
- Bacterial infections: Group B Streptococcus (GBS), Escherichia coli, Listeria monocytogenes, Staphylococcus aureus, coagulase-negative staphylococci, etc.
- Viral infections: Herpes simplex virus, cytomegalovirus, rubella virus, enterovirus, parechovirus, etc.
- Fungal infections: Candida species, Aspergillus, Zygomycetes, etc.
- Protozoal infections: Toxoplasma gondii, Plasmodium species, etc.
2.3 Classification Based on Site of Infection
Site-Based Classification:
- Bloodstream infections: Neonatal sepsis
- Central nervous system infections: Meningitis, encephalitis
- Respiratory infections: Pneumonia, bronchiolitis
- Gastrointestinal infections: Necrotizing enterocolitis, gastroenteritis
- Skin and soft tissue infections: Cellulitis, impetigo, omphalitis
- Urinary tract infections: Cystitis, pyelonephritis
- Eye infections: Conjunctivitis, ophthalmia neonatorum
Each classification system provides valuable insights into the potential etiology, pathogenesis, and management approach for neonatal infections. In clinical practice, these classifications are often used in combination to guide comprehensive patient care.
3. Early-Onset vs Late-Onset Neonatal Infections
The distinction between early-onset and late-onset neonatal infections is crucial as it influences the likely pathogens, clinical presentation, treatment approach, and outcomes. This classification is primarily based on the timing of symptom onset after birth.
| Feature | Early-Onset Infections | Late-Onset Infections |
|---|---|---|
| Timing | Within first 72 hours (some definitions extend to 7 days) of life | After 72 hours (or 7 days) up to 28 days of life |
| Mode of Transmission | Vertical transmission from mother (transplacental, ascending from birth canal, or during delivery) | Horizontal transmission from environment, healthcare workers, or community |
| Common Pathogens | Group B Streptococcus, E. coli, Listeria monocytogenes, Klebsiella | Coagulase-negative staphylococci, S. aureus, E. coli, Klebsiella, Pseudomonas, Candida |
| Risk Factors | Premature rupture of membranes, maternal fever, chorioamnionitis, inadequate GBS prophylaxis | Prematurity, low birth weight, invasive procedures, central lines, prolonged hospitalization |
| Clinical Presentation | Often fulminant with respiratory distress, shock; commonly presents as pneumonia | More insidious onset; often presents as septicemia or meningitis |
| Prevention Strategies | Maternal screening, intrapartum antibiotic prophylaxis, proper antenatal care | Infection control measures, hand hygiene, proper central line care, minimal invasive procedures |
3.1 Early-Onset Infections
Early-onset neonatal infections typically manifest within the first 72 hours of life and are usually acquired from the maternal genital tract before or during delivery. These infections often present as respiratory distress or pneumonia due to in utero aspiration of infected amniotic fluid.
Risk Factors for Early-Onset Infections:
- Maternal factors:
- Maternal colonization with GBS
- Premature rupture of membranes (PROM) > 18 hours
- Chorioamnionitis
- Maternal fever during labor
- Multiple vaginal examinations during labor
- Urinary tract infection near delivery
- Neonatal factors:
- Prematurity (<37 weeks gestation)
- Low birth weight (<2500g)
- Male gender
- Apgar score <6 at 5 minutes
- Congenital anomalies
The clinical presentation of early-onset infections is often characterized by respiratory distress, lethargy, feeding difficulties, temperature instability, and cardiovascular instability. These infections can progress rapidly and may lead to septic shock if not promptly recognized and treated.
3.2 Late-Onset Infections
Late-onset neonatal infections occur after 72 hours of life and are predominantly acquired from the environment (hospital or community). These infections may present more subtly and are often associated with invasive procedures and prolonged hospital stays.
Risk Factors for Late-Onset Infections:
- Prematurity – particularly very low birth weight infants (<1500g)
- Invasive procedures – central venous catheters, endotracheal intubation, surgeries
- Prolonged hospitalization and ICU stay
- Parenteral nutrition, especially lipid emulsions
- Previous antibiotic exposure disrupting normal flora
- Inadequate infection control practices in healthcare settings
- Immunocompromised state due to underlying conditions
Late-onset infections may present with more subtle clinical features, including feeding intolerance, lethargy, temperature instability, apnea, or bradycardia. These infections may manifest as focal infections such as meningitis, osteomyelitis, or urinary tract infections, in addition to generalized sepsis.
Clinical Pearl:
Never disregard subtle changes in a neonate’s behavior or feeding patterns. In late-onset neonatal infections, early signs might be limited to poor feeding, increased sleeping, or mild temperature instability, which can rapidly progress to severe sepsis if missed.
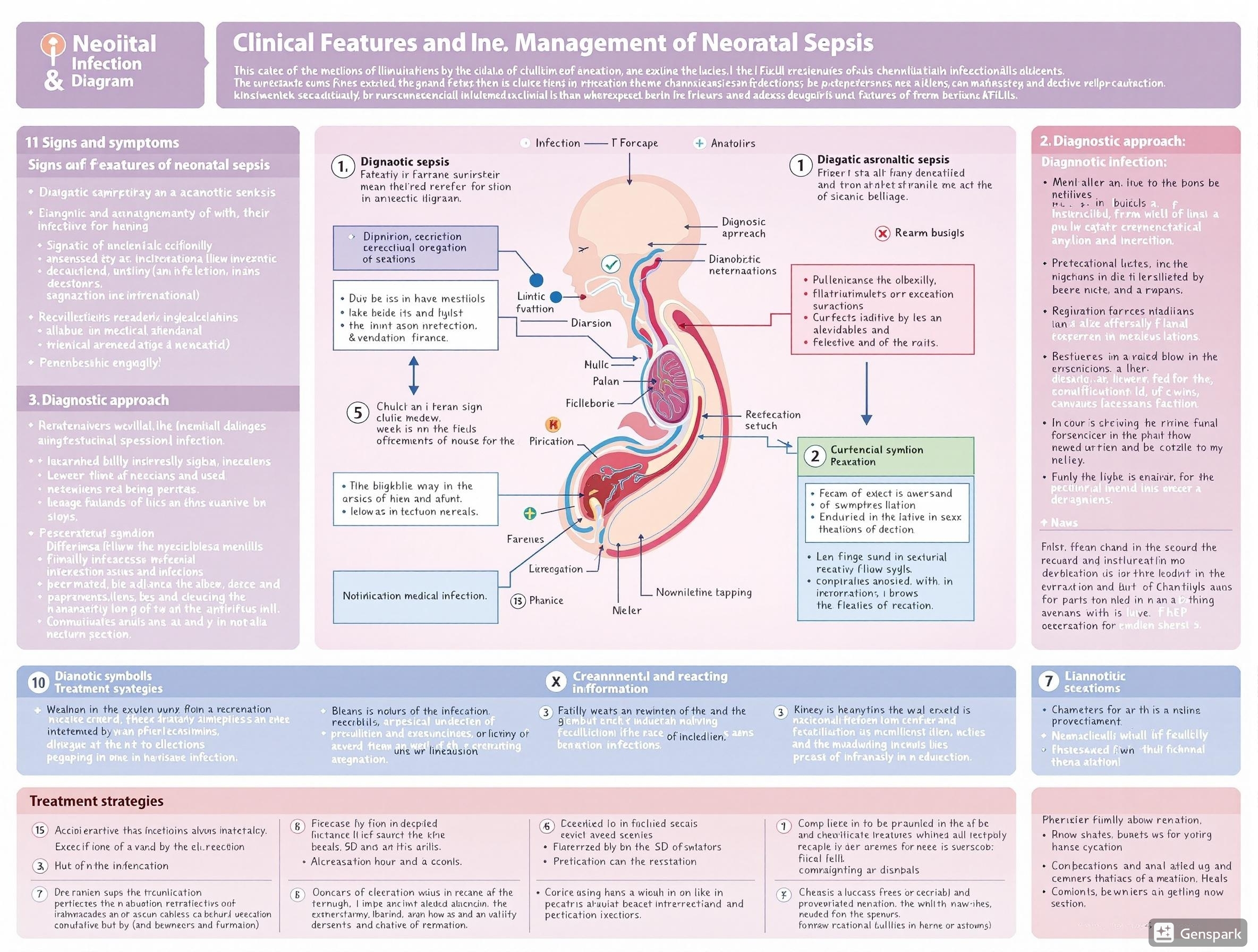
Figure 1: Diagnostic approach and management of neonatal infections showing clinical features, diagnostic methods, and treatment strategies.
4. Bacterial Infections in Neonates
Bacterial infections are the most common cause of neonatal infections, accounting for the majority of cases of neonatal sepsis, pneumonia, and meningitis. Understanding the pathophysiology, clinical presentation, and management of these infections is crucial for nursing care.
4.1 Neonatal Sepsis
Definition
Neonatal sepsis is a systemic inflammatory response syndrome occurring in a neonate less than 28 days of life due to suspected or proven infection. It is one of the leading causes of neonatal mortality worldwide.
Pathophysiology of Neonatal Sepsis
Neonatal sepsis develops when pathogenic bacteria enter the bloodstream and trigger a systemic inflammatory response. The immature immune system of neonates contributes to their vulnerability, with limitations in:
- Neutrophil function: Reduced chemotaxis, phagocytosis, and bactericidal activity
- Complement system: Lower levels of complement proteins, particularly C3 and C5
- Antibody production: Limited immunoglobulin production and maternal IgG transfer in premature infants
- Cytokine response: Dysregulated pro-inflammatory cytokine production leading to excessive inflammation
- Physical barriers: Thin, permeable skin and mucous membranes
Clinical Manifestations
The clinical presentation of neonatal sepsis is often nonspecific and can include:
| System | Signs and Symptoms |
|---|---|
| General | Temperature instability (hypothermia or hyperthermia), poor feeding, lethargy, irritability |
| Respiratory | Tachypnea, grunting, retractions, apnea, cyanosis, increased oxygen requirements |
| Cardiovascular | Tachycardia, bradycardia, hypotension, poor perfusion, prolonged capillary refill time |
| Gastrointestinal | Feeding intolerance, abdominal distension, vomiting, diarrhea, hepatomegaly |
| Neurological | Lethargy, irritability, hypotonia, seizures, bulging fontanelle |
| Hematological | Pallor, petechiae, purpura, bleeding tendency |
| Skin | Mottling, cyanosis, jaundice, pustules, sclerema |
Management of Neonatal Sepsis
The principles of management include:
- Prompt recognition of signs and symptoms
- Immediate initiation of empirical antimicrobial therapy
- Supportive care (fluid management, respiratory support, temperature regulation)
- Source control (removal of infected catheters, drainage of abscesses)
- Continuous monitoring for complications and response to treatment
Mnemonic: “SEPTIC”
To remember common signs of neonatal sepsis:
S – Skin changes (mottling, poor perfusion)
E – Eating problems (feeding intolerance)
P – Pneumonia symptoms (respiratory distress)
T – Temperature instability
I – Irritability or lethargy
C – Cardiovascular changes (tachycardia, hypotension)
4.2 Bacterial Meningitis
Definition
Neonatal meningitis is inflammation of the meninges due to bacterial infection in the first 28 days of life. It can occur as a complication of sepsis or as a primary infection.
Epidemiology and Etiology
Neonatal meningitis affects approximately 0.25-1.0 per 1000 live births. The most common causative organisms include:
- Group B Streptococcus (Streptococcus agalactiae)
- Escherichia coli (particularly K1 strains)
- Listeria monocytogenes
- Streptococcus pneumoniae
- Enterococci
- Gram-negative bacilli (Klebsiella, Enterobacter, Pseudomonas)
Clinical Features
Neonatal meningitis may present with nonspecific symptoms similar to sepsis, as well as some more specific neurological signs:
- Irritability or lethargy
- Poor feeding
- Temperature instability
- Bulging fontanelle
- Seizures (occur in 30-40% of cases)
- Nuchal rigidity (less common in neonates)
- Hypotonia or hypertonia
- Apnea or bradycardia
- High-pitched cry
Diagnosis
Diagnosis is confirmed by cerebrospinal fluid (CSF) analysis obtained through lumbar puncture. Typical CSF findings in bacterial meningitis include:
| Parameter | Normal Neonatal CSF | Bacterial Meningitis |
|---|---|---|
| WBC count | 0-30 cells/mm³ | >100 cells/mm³, neutrophil predominance |
| Protein | 20-170 mg/dL | >170 mg/dL |
| Glucose | 30-80 mg/dL or >60% of blood glucose | <30 mg/dL or <50% of blood glucose |
| Gram stain | No organisms | Organisms may be visible |
| Culture | No growth | Positive for bacteria |
Management
Treatment of neonatal meningitis includes:
- Empirical antibiotics: Combination therapy with ampicillin and gentamicin or ampicillin and cefotaxime until culture results are available
- Duration of therapy: 14-21 days for GBS and Listeria; 21-28 days for gram-negative organisms
- Supportive care: Manage seizures, maintain adequate cerebral perfusion, monitor for complications
- Follow-up: Repeat lumbar puncture to document CSF sterilization, neuroimaging, hearing assessment
Clinical Pearl:
Neonatal meningitis can be present without the classic signs seen in older children. A high index of suspicion should be maintained for any neonate with sepsis, as 10-30% of neonates with sepsis may have concurrent meningitis.
4.3 Neonatal Pneumonia
Definition
Neonatal pneumonia is inflammation of the lung parenchyma due to infectious agents in the first 28 days of life. It can be congenital (acquired in utero), early-onset (within first 7 days), or late-onset (after 7 days).
Etiology
The causative organisms vary depending on the timing of infection:
- Congenital/Early-onset: Group B Streptococcus, E. coli, Klebsiella, Listeria monocytogenes, Ureaplasma urealyticum
- Late-onset: Staphylococcus aureus, Pseudomonas, Klebsiella, viral pathogens
Clinical Features
- Tachypnea (respiratory rate >60 breaths/min)
- Retractions (subcostal, intercostal, sternal)
- Grunting
- Nasal flaring
- Decreased air entry
- Crackles or rales
- Cyanosis
- Increased oxygen requirement
- Apnea episodes
Diagnosis
- Chest radiography: May show infiltrates, consolidation, air bronchograms, pleural effusion
- Blood cultures: To identify causative organism
- Tracheal aspirate culture (in intubated neonates)
- Complete blood count: May show leukocytosis or leukopenia
- Arterial blood gas: May indicate respiratory insufficiency
Management
Treatment approaches include:
- Antimicrobial therapy: Empirical antibiotics based on likely pathogens (ampicillin plus gentamicin for early-onset; vancomycin plus cefotaxime for late-onset)
- Respiratory support: Oxygen supplementation, CPAP, mechanical ventilation as needed
- Supportive care: Fluid management, temperature regulation, nutritional support
- Monitoring: Continuous pulse oximetry, cardiorespiratory monitoring
Nursing Tip:
When caring for neonates with pneumonia, ensure proper positioning (head of bed elevated 30-45 degrees), frequent suctioning of secretions, and careful monitoring of respiratory status. Document oxygen requirements, work of breathing, and any changes in respiratory parameters.
4.4 Omphalitis
Definition
Omphalitis is infection of the umbilical cord stump and surrounding tissues. It represents a serious neonatal infection that can rapidly progress to systemic infection if not promptly treated.
Etiology
Omphalitis is typically polymicrobial, with the most common organisms including:
- Staphylococcus aureus
- Group A Streptococcus
- Escherichia coli
- Klebsiella pneumoniae
- Proteus species
- Anaerobic bacteria (Bacteroides, Clostridium)
Clinical Features
- Erythema around the umbilical stump
- Edema and induration of periumbilical tissues
- Purulent or malodorous discharge from the umbilicus
- Tenderness on palpation
- In severe cases: Abdominal wall discoloration, crepitus, or systemic signs of sepsis
Risk Factors
- Low birth weight or prematurity
- Improper cord care practices
- Unhygienic delivery conditions
- Prolonged rupture of membranes
- Umbilical catheterization
- Maternal infection during delivery
Management
- Antimicrobial therapy: Broad-spectrum antibiotics (typically a combination of ampicillin, gentamicin, and clindamycin or metronidazole) to cover gram-positive, gram-negative, and anaerobic organisms
- Local care: Gentle cleansing of the umbilical area with antiseptic solutions
- Surgical intervention: May be required for necrotizing fasciitis, myonecrosis, or abdominal wall abscess
- Supportive care: IV fluids, temperature regulation, cardiorespiratory monitoring
Clinical Pearl:
Omphalitis is a medical emergency that can rapidly progress to necrotizing fasciitis, myonecrosis, portal vein thrombosis, or systemic sepsis. Prompt recognition and aggressive treatment are essential to prevent these potentially fatal complications.
4.5 Other Bacterial Infections
4.5.1 Neonatal Conjunctivitis (Ophthalmia Neonatorum)
Infection of the conjunctiva in the first 28 days of life, commonly caused by:
- Neisseria gonorrhoeae: Presents with copious purulent discharge 2-5 days after birth
- Chlamydia trachomatis: More common, presents with watery to mucoid discharge 5-14 days after birth
- Other bacteria: Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae
Management: Depends on the causative organism; includes topical and/or systemic antibiotics and careful eye hygiene.
4.5.2 Neonatal Skin Infections
Impetigo
Superficial skin infection characterized by vesicles that rupture and form honey-colored crusts. Commonly caused by Staphylococcus aureus or Group A Streptococcus.
Management: Topical mupirocin for limited disease; oral antibiotics (e.g., cephalexin) for extensive disease.
Cellulitis
Infection of the dermis and subcutaneous tissues, presenting with erythema, warmth, and tenderness of the affected area. Common sites include the face, neck, and periumbilical area.
Management: Systemic antibiotics covering Staphylococcus aureus and Streptococcus; hospitalization may be required.
4.5.3 Urinary Tract Infections
Relatively uncommon in the neonatal period, but more frequent in males and infants with urinary tract anomalies. Common pathogens include E. coli, Klebsiella, and Enterococcus.
Clinical features may be nonspecific, including poor feeding, vomiting, jaundice, or fever.
Management: Appropriate antibiotics based on culture and sensitivity; investigation for underlying structural abnormalities.
4.5.4 Necrotizing Enterocolitis (NEC)
A serious gastrointestinal emergency primarily affecting premature infants, characterized by intestinal inflammation, invasion of enteric bacteria, and potential necrosis.
Clinical features: Feeding intolerance, abdominal distension, bilious vomiting, bloody stools, lethargy.
Management: Bowel rest, gastric decompression, antibiotics, supportive care; surgical intervention for perforation or necrosis.
6. Fungal Infections in Neonates
Fungal infections represent an important cause of neonatal infections, particularly in premature and low birth weight infants requiring prolonged hospitalization and invasive procedures. Candida species are the most common fungal pathogens in neonates, but other fungi such as Aspergillus and Malassezia can also cause infection.
6.1 Neonatal Candidiasis
Definition
Neonatal candidiasis refers to infections caused by Candida species in the neonatal period. It can manifest as mucocutaneous disease (thrush, diaper dermatitis) or invasive disease (candidemia, disseminated candidiasis).
Epidemiology and Risk Factors
- Incidence: 1-4% of very low birth weight (VLBW) infants develop invasive candidiasis
- Risk factors:
- Prematurity (especially <28 weeks gestation)
- Very low birth weight (<1500g)
- Central venous catheters
- Parenteral nutrition, especially lipid emulsions
- Broad-spectrum antibiotic therapy
- H2-receptor antagonists or proton pump inhibitors
- Abdominal surgery
- Endotracheal intubation
- Maternal vaginal candidiasis
Clinical Manifestations
Mucocutaneous Candidiasis
- Oral thrush: White, adherent plaques on the oral mucosa that cannot be easily wiped away
- Diaper dermatitis: Erythematous rash with satellite lesions in the diaper area
- Congenital cutaneous candidiasis: Generalized erythematous maculopapular or pustular rash present at birth or within 12 hours
Invasive Candidiasis
- Candidemia: Often presents with nonspecific signs similar to bacterial sepsis
- Disseminated candidiasis: Multiple organ involvement including:
- Central nervous system (meningitis)
- Eyes (endophthalmitis)
- Heart (endocarditis)
- Lungs (pneumonia)
- Kidneys (renal abscesses)
- Liver and spleen (hepatosplenic abscesses)
- Bones and joints (osteomyelitis, arthritis)
Diagnosis
- Blood cultures: Gold standard for candidemia, but may take 2-3 days and have limited sensitivity
- Other cultures: Urine, CSF, endotracheal aspirates, peritoneal fluid as clinically indicated
- Direct microscopy: KOH preparation of skin scrapings or oral lesions
- Biomarkers: Beta-D-glucan, mannan, anti-mannan antibodies (not routinely used in neonates)
- PCR: Emerging technique with improved sensitivity and rapid results
- Imaging: Echocardiography, abdominal ultrasound, cranial ultrasound or MRI to detect metastatic foci
- Ophthalmologic examination: To rule out endophthalmitis
Management
Mucocutaneous Candidiasis
- Oral thrush: Nystatin suspension (100,000 units/mL) 0.5-1 mL to each side of the mouth four times daily
- Diaper dermatitis: Topical antifungal creams (nystatin, miconazole, clotrimazole)
- Congenital cutaneous candidiasis: Topical therapy for limited disease; systemic therapy if extensive or in VLBW infants
Invasive Candidiasis
- First-line therapy:
- Amphotericin B deoxycholate (1 mg/kg/day) or
- Liposomal amphotericin B (3-5 mg/kg/day) or
- Micafungin (10 mg/kg/day for neonates <1000g; 7-10 mg/kg/day for neonates >1000g)
- Alternative therapy: Fluconazole (12 mg/kg loading dose, then 6-12 mg/kg/day) if Candida is susceptible
- Duration:
- Candidemia without metastatic complications: minimum 14 days after first negative blood culture
- Disseminated candidiasis: 4-6 weeks or longer depending on clinical response
- Additional measures:
- Removal of central venous catheters when possible
- Evaluation for metastatic foci (ophthalmologic exam, echocardiogram, ultrasound)
- Monitoring of liver and renal function during antifungal therapy
Prevention
- Fluconazole prophylaxis: 3-6 mg/kg twice weekly for neonates <1000g in NICUs with high incidence of invasive candidiasis
- Nystatin prophylaxis: Oral nystatin (100,000 units three times daily) is an alternative where fluconazole is unavailable
- Infection control measures: Hand hygiene, minimal handling, sterile technique for procedures
- Antimicrobial stewardship: Judicious use of broad-spectrum antibiotics
Nursing Tip:
When administering oral nystatin for thrush, apply it directly to the affected areas rather than mixing with feeds. Ensure the medication contacts all oral surfaces by swabbing gently around the mouth. Continue treatment for 48-72 hours after lesions have resolved to prevent recurrence.
6.2 Invasive Fungal Infections
6.2.1 Aspergillosis
Although rare in neonates, invasive aspergillosis can occur, particularly in extremely premature infants with prolonged hospitalization and multiple risk factors.
Clinical manifestations: Primarily pulmonary (pneumonia), but can disseminate to other organs including the brain, heart, and skin.
Diagnosis: Difficult; may require bronchoscopy with bronchoalveolar lavage, tissue biopsy, and fungal cultures. Galactomannan assay may be helpful but has not been well-validated in neonates.
Treatment: Voriconazole is the first-line agent; liposomal amphotericin B is an alternative. Prolonged therapy is required (minimum 6-12 weeks).
6.2.2 Malassezia Infections
Malassezia species, particularly M. furfur, can cause fungemia in premature infants receiving lipid emulsions through central venous catheters.
Clinical features: Fever, feeding intolerance, respiratory deterioration; may be indistinguishable from other causes of sepsis.
Diagnosis: Blood cultures with lipid supplementation; skin cultures if cutaneous lesions are present.
Management: Discontinuation of lipid infusions, removal of central venous catheters, and treatment with fluconazole or amphotericin B.
6.2.3 Zygomycosis (Mucormycosis)
Extremely rare but often fatal in neonates. Typically involves cutaneous infection at sites of skin trauma (adhesive tape, electrode placement).
Clinical features: Rapidly progressive necrotic skin lesions that may invade underlying tissues.
Management: Aggressive surgical debridement combined with high-dose liposomal amphotericin B.
Critical Warning:
Invasive fungal infections in neonates often have subtle initial presentations but can rapidly progress to life-threatening disease. Maintain a high index of suspicion in high-risk infants, particularly extremely premature neonates with multiple risk factors who have persistent clinical deterioration despite antibiotic therapy.
7. Diagnosis of Neonatal Infections
Early and accurate diagnosis of neonatal infections is crucial for timely intervention and improved outcomes. The diagnostic approach combines clinical assessment, laboratory investigations, and sometimes imaging studies. The challenge lies in the nonspecific presentation of infections in neonates and the limitations of some diagnostic tests in this population.
7.1 Clinical Assessment
The clinical assessment of a neonate with suspected infection includes a thorough history, physical examination, and recognition of risk factors.
Maternal History
- Premature rupture of membranes > 18 hours
- Maternal fever during labor (>38°C or 100.4°F)
- Chorioamnionitis
- Group B Streptococcus colonization
- Inadequate intrapartum antibiotic prophylaxis
- History of genital herpes or active lesions
- Sexually transmitted infections during pregnancy
- Vaginal or rectal colonization with pathogenic organisms
Neonatal Risk Factors
- Prematurity (<37 weeks gestation)
- Low birth weight (<2500g)
- Resuscitation at birth
- Invasive procedures (central lines, endotracheal intubation)
- Prolonged hospitalization
- Previous antibiotic exposure
Physical Examination
Signs and symptoms of neonatal infection can be nonspecific and may include:
| System | Signs and Symptoms |
|---|---|
| General | Temperature instability (hypo- or hyperthermia), lethargy, irritability, poor feeding |
| Respiratory | Tachypnea, grunting, nasal flaring, retractions, apnea, cyanosis |
| Cardiovascular | Tachycardia, bradycardia, hypotension, poor perfusion, delayed capillary refill |
| Gastrointestinal | Abdominal distension, vomiting, feeding intolerance, diarrhea, hepatomegaly |
| Neurological | Hypotonia, lethargy, irritability, seizures, bulging fontanelle, high-pitched cry |
| Hematological | Pallor, petechiae, purpura, easy bruising |
| Skin | Mottling, poor perfusion, jaundice, pustules, vesicles, omphalitis |
Clinical Pearl:
The absence of fever does not rule out infection in neonates. In fact, hypothermia may be a more common manifestation of neonatal infection than fever, particularly in preterm infants. Any unexpected change in a neonate’s clinical status should raise suspicion for infection.
7.2 Laboratory Investigations
7.2.1 Blood Tests
- Complete blood count (CBC) with differential:
- White blood cell count (WBC): Leukocytosis (>30,000/mm³) or leukopenia (<5,000/mm³)
- Absolute neutrophil count (ANC): Neutropenia (<1,500/mm³) is concerning
- Immature-to-total neutrophil ratio (I:T ratio): >0.2 suggests infection
- Platelet count: Thrombocytopenia (<100,000/mm³) may indicate severe infection
- Blood culture: Gold standard for diagnosing bacteremia; collect before starting antibiotics when possible; 1-2 mL of blood improves yield
- C-reactive protein (CRP): Elevation (>10 mg/L) occurs 6-8 hours after onset of infection; serial measurements more useful than a single value
- Procalcitonin: Rises earlier than CRP (within 2-4 hours); levels >2 ng/mL suggest bacterial infection
- Serum glucose: Hyper- or hypoglycemia may occur with sepsis
- Blood gas analysis: May show metabolic acidosis in severe infection
7.2.2 Cerebrospinal Fluid (CSF) Analysis
Lumbar puncture should be performed in neonates with suspected sepsis, particularly those with late-onset sepsis or neurological symptoms.
| Parameter | Term Neonate | Preterm Neonate | Bacterial Meningitis | Viral Meningitis |
|---|---|---|---|---|
| WBC (cells/mm³) | 0-20 | 0-25 | >100 (neutrophil predominance) | 5-1000 (lymphocyte predominance) |
| Protein (mg/dL) | 20-170 | 65-150 | >170 | Mildly elevated |
| Glucose (mg/dL) | 30-80 | 20-80 | <30 or <50% of blood glucose | Normal or slightly decreased |
7.2.3 Urine Tests
- Urinalysis: Pyuria (>5 WBC/hpf), positive leukocyte esterase or nitrite
- Urine culture: Obtained by suprapubic aspiration or catheterization; bag specimens are not reliable
7.2.4 Microbiological Tests
- Cultures: Blood, CSF, urine, endotracheal aspirate, wounds, skin lesions as clinically indicated
- Gram stain: Direct visualization of bacteria in clinical specimens
- Viral studies: PCR for HSV, enterovirus, parechovirus in CSF, blood, and surface swabs
- TORCH serologies: When congenital infection is suspected
7.2.5 Molecular Diagnostic Techniques
- Polymerase chain reaction (PCR): Rapid detection of bacterial and viral pathogens
- Multiplex PCR panels: Simultaneous detection of multiple pathogens
- 16S rRNA sequencing: Identification of bacteria that are difficult to culture
- MALDI-TOF mass spectrometry: Rapid identification of bacterial species
7.3 Imaging Studies
7.3.1 Chest Radiography
Indicated for neonates with respiratory symptoms or suspected pneumonia. Findings may include:
- Infiltrates or consolidation
- Pleural effusion
- Air bronchograms
- Atelectasis
7.3.2 Abdominal Radiography
Useful in evaluating for necrotizing enterocolitis (NEC) or other intra-abdominal pathology. Findings may include:
- Pneumatosis intestinalis (air in the bowel wall)
- Portal venous gas
- Pneumoperitoneum (free air)
- Ileus or bowel dilation
7.3.3 Cranial Ultrasonography
Useful for detecting:
- Ventriculomegaly
- Brain abscess
- Periventricular leukomalacia
- Intracranial hemorrhage
7.3.4 Magnetic Resonance Imaging (MRI)
Provides detailed imaging of the brain and is particularly useful in:
- HSV encephalitis
- Congenital CMV infection
- Congenital toxoplasmosis
- Evaluation of brain abscesses
7.3.5 Echocardiography
Indicated for neonates with suspected endocarditis or in cases of persistent candidemia. May detect:
- Vegetations on heart valves or endocardium
- Myocardial abscesses
- Pericardial effusion
Diagnostic Algorithm
For suspected neonatal infection, obtain:
- Complete blood count with differential
- Blood culture (1-2 mL)
- CRP and/or procalcitonin
- Consider lumbar puncture for CSF analysis (especially for late-onset sepsis)
- Urine culture if age >72 hours
- Chest X-ray if respiratory symptoms are present
- Additional cultures and viral studies based on clinical presentation
8. Treatment Approaches
The treatment of neonatal infections requires a multidisciplinary approach and often involves empiric antimicrobial therapy initiated before definitive diagnosis, followed by targeted therapy once the causative pathogen is identified. Supportive care is equally important in managing these vulnerable patients.
8.1 Antibiotic Therapy
8.1.1 Empirical Antibiotic Therapy
Initial empiric antibiotic selection is based on the likely pathogens, which vary depending on the timing of infection (early vs. late onset) and local epidemiology.
| Clinical Scenario | Recommended Empirical Regimen | Rationale |
|---|---|---|
| Early-onset sepsis | Ampicillin + Gentamicin | Covers GBS, E. coli, Listeria, and other common early-onset pathogens |
| Late-onset sepsis (community-acquired) | Ampicillin + Gentamicin or Ampicillin + Cefotaxime | Covers common community-acquired pathogens |
| Late-onset sepsis (hospital-acquired) | Vancomycin + Gentamicin or Cefotaxime | Covers coagulase-negative staphylococci, S. aureus, and gram-negative bacilli |
| Meningitis (suspected) | Ampicillin + Cefotaxime | Better CSF penetration of cefotaxime compared to gentamicin |
| Necrotizing enterocolitis | Ampicillin + Gentamicin + Metronidazole or Piperacillin-tazobactam | Coverage for enteric and anaerobic organisms |
8.1.2 Antibiotic Dosing
| Antibiotic | Dose (Term Neonates) | Dose (Preterm Neonates) | Interval |
|---|---|---|---|
| Ampicillin | 50-100 mg/kg/dose (meningitis: 100 mg/kg/dose) | 50 mg/kg/dose | q8h-q12h depending on age |
| Gentamicin | 4-5 mg/kg/dose | 3.5-4 mg/kg/dose | q24h-q48h depending on gestational and postnatal age |
| Cefotaxime | 50 mg/kg/dose | 50 mg/kg/dose | q8h-q12h depending on age |
| Vancomycin | 10-15 mg/kg/dose | 10-15 mg/kg/dose | q8h-q24h depending on gestational and postnatal age |
| Metronidazole | 7.5 mg/kg/dose | 7.5 mg/kg/dose | q12h-q24h depending on age |
8.1.3 Duration of Therapy
| Condition | Recommended Duration | Comments |
|---|---|---|
| Culture-negative sepsis | 48-72 hours | If clinical improvement and negative cultures |
| Bacteremia | 10-14 days | From first negative blood culture |
| Meningitis (GBS) | 14-21 days | Minimum 14 days from sterilization of CSF |
| Meningitis (gram-negative) | 21-28 days | Longer duration for complicated cases |
| Bone/joint infections | 3-4 weeks | May require surgical drainage |
| Endocarditis | 4-6 weeks | From first negative blood culture |
Nursing Tip:
When administering gentamicin, ensure that serum levels are monitored (peak and trough) to prevent ototoxicity and nephrotoxicity. Administer the drug over 30 minutes and flush the IV line thoroughly afterward. Document the exact time of administration to ensure accurate timing of level measurements.
8.3 Antifungal Therapy
8.3.1 Candida Infections
| Antifungal Agent | Indication | Dosage | Duration |
|---|---|---|---|
| Amphotericin B deoxycholate | Invasive candidiasis, first-line agent in neonates | 1 mg/kg/day IV once daily | 14-21 days after negative cultures |
| Liposomal amphotericin B | Alternative to conventional amphotericin B | 3-5 mg/kg/day IV once daily | 14-21 days after negative cultures |
| Fluconazole | Susceptible Candida species | 12 mg/kg loading dose, then 6-12 mg/kg/day | 14-21 days after negative cultures |
| Micafungin | Alternative for invasive candidiasis | 10 mg/kg/day for neonates <1000g; 7-10 mg/kg/day for neonates >1000g | 14-21 days after negative cultures |
| Nystatin | Oral thrush, prophylaxis | 100,000 units (1 mL) per side of mouth 4 times daily | 7-14 days for treatment; continued during risk period for prophylaxis |
8.3.2 Prophylaxis
- Fluconazole prophylaxis: Consider in extremely low birth weight infants (<1000g) in NICUs with high incidence of invasive candidiasis
- Dosage: 3-6 mg/kg twice weekly
- Duration: Until central lines are removed or until 6 weeks of age
8.3.3 Special Considerations
- Central venous catheter removal: Recommended in candidemia
- Ophthalmologic examination: To rule out endophthalmitis
- Echocardiography: To rule out endocarditis
- Monitoring: Follow blood cultures until negative, monitor renal and hepatic function
8.4 Supportive Care
Supportive care is a crucial component in the management of neonatal infections and may include:
8.4.1 Respiratory Support
- Oxygen supplementation
- Continuous positive airway pressure (CPAP)
- Mechanical ventilation
- Surfactant administration (if indicated)
- Proper positioning and suctioning
8.4.2 Hemodynamic Support
- Fluid resuscitation (10-20 mL/kg boluses of normal saline or lactated Ringer’s solution)
- Inotropic support (dopamine, dobutamine, epinephrine)
- Vasopressor support for persistent hypotension
- Blood product transfusions as needed (packed RBCs, platelets, fresh frozen plasma)
8.4.3 Nutritional Support
- Intravenous fluids with appropriate glucose, electrolytes, and minerals
- Parenteral nutrition for prolonged illness
- Enteral nutrition when tolerated
- Breast milk (preferred) or formula when oral feeding is possible
8.4.4 Metabolic Management
- Glucose monitoring and management of hypo/hyperglycemia
- Electrolyte monitoring and correction of imbalances
- Acid-base balance management
- Temperature regulation (avoid hyperthermia and hypothermia)
8.4.5 Neurological Support
- Seizure recognition and management
- Intracranial pressure monitoring in severe cases
- Phenobarbital or levetiracetam for seizure control
- Neuroprotective strategies when appropriate
8.4.6 Pain Management and Comfort Measures
- Assessment of pain using validated neonatal pain scales
- Non-pharmacological comfort measures (swaddling, sucrose, non-nutritive sucking)
- Pharmacological pain management when indicated
- Minimal handling and clustering of care activities
Response to Treatment
Monitor for signs of improvement, which typically include:
- Resolution of temperature instability
- Improved feeding tolerance
- Decreased respiratory effort
- Improved perfusion and hemodynamic stability
- Normalization of laboratory values
- Resolution of specific symptoms related to the site of infection
9. Nursing Care and Management
Nursing care is fundamental in the management of neonates with infections. Nurses are at the frontline of recognizing early signs of infection, implementing prescribed treatments, providing supportive care, and educating families.
9.1 Nursing Assessment
Comprehensive nursing assessment is critical for early identification of neonatal infections. Key components include:
9.1.1 General Assessment
- Vital signs: Temperature, heart rate, respiratory rate, blood pressure, oxygen saturation
- Activity level: Lethargy, irritability, responsiveness
- Skin assessment: Color, perfusion, rashes, lesions, mottling
- Feeding pattern: Intake, tolerance, sucking strength
- Elimination: Urine output, stool pattern and characteristics
- Weight: Daily weight to monitor fluid status and nutritional status
9.1.2 System-Specific Assessment
- Respiratory: Work of breathing, use of accessory muscles, retractions, nasal flaring, grunting, breath sounds
- Cardiovascular: Peripheral perfusion, capillary refill time, pulses, heart sounds
- Gastrointestinal: Abdominal distension, tenderness, bowel sounds, vomiting, gastric residuals
- Neurological: Level of consciousness, fontanelle assessment, reflexes, tone, seizure activity
- Umbilical cord: Signs of omphalitis (erythema, discharge, tenderness)
Nursing Tip:
Use a systematic approach when assessing neonates for signs of infection. Compare current findings with the neonate’s baseline status, as subtle changes can be the earliest indicators of deterioration. Document and report changes promptly to facilitate early intervention.
9.2 Nursing Diagnoses
Common nursing diagnoses for neonates with infections include:
| Nursing Diagnosis | Related Factors | Defining Characteristics |
|---|---|---|
| Risk for Ineffective Thermoregulation | Infection process, immature thermoregulatory mechanisms | Temperature instability, hypothermia or hyperthermia |
| Ineffective Breathing Pattern | Respiratory infection, sepsis-induced respiratory distress | Tachypnea, nasal flaring, retractions, grunting, apnea |
| Risk for Impaired Skin Integrity | Invasive procedures, poor perfusion, skin lesions | Rashes, lesions, poor tissue perfusion, edema |
| Imbalanced Nutrition: Less Than Body Requirements | Feeding intolerance, increased metabolic demands | Poor feeding, weight loss, vomiting, abdominal distension |
| Risk for Impaired Gas Exchange | Pneumonia, respiratory distress | Hypoxemia, increased work of breathing, cyanosis |
| Risk for Deficient Fluid Volume | Fever, poor intake, vomiting, diarrhea | Decreased urine output, dry mucous membranes, sunken fontanelle |
| Acute Pain | Inflammatory process, invasive procedures | Irritability, crying, physiological indicators (tachycardia, hypertension) |
| Risk for Infection Transmission | Contagious pathogens, invasive devices | Presence of transmissible pathogens |
| Anxiety (Parents/Family) | Uncertainty about prognosis, invasive procedures, separation | Expressed concerns, questions, emotional distress |
| Risk for Impaired Parent-Infant Attachment | Separation due to isolation or intensive care needs | Limited physical contact, expressed feelings of helplessness |
9.3 Nursing Interventions
9.3.1 Infection Control Measures
- Hand hygiene: Strict adherence to hand washing before and after patient contact
- Personal protective equipment (PPE): Gloves, gowns, masks as appropriate based on isolation precautions
- Isolation practices: Implementation of appropriate isolation based on suspected/confirmed pathogen
- Equipment management: Dedicated equipment, proper cleaning and disinfection
- Environmental cleaning: Regular cleaning and disinfection of patient care areas
9.3.2 Medication Administration
- Antimicrobial therapy: Accurate preparation and administration of antibiotics, antivirals, or antifungals
- Timing: Administration at precise intervals to maintain therapeutic levels
- Monitoring: Assessment for therapeutic effects and adverse reactions
- Central line management: Aseptic technique for all line access, dressing changes per protocol
9.3.3 Thermoregulation
- Temperature monitoring: Frequent assessment of axillary or core temperature
- Environmental control: Appropriate incubator or radiant warmer settings
- Neutral thermal environment: Adjusting environmental temperature based on neonate’s needs
- Intervention for hyperthermia: Gradual cooling measures, not rapid cooling
9.3.4 Respiratory Support
- Positioning: Proper positioning to optimize oxygenation (elevated head of bed)
- Oxygen administration: Appropriate delivery method and monitoring of oxygen saturation
- Suctioning: Gentle suctioning as needed to maintain airway patency
- Ventilator management: Monitoring ventilator settings, preventing complications
- Respiratory assessment: Regular evaluation of respiratory status and work of breathing
9.3.5 Nutritional Support
- Feeding plan: Implementation of appropriate feeding method (oral, gavage, parenteral)
- Monitoring tolerance: Assessment for feeding intolerance, gastric residuals
- Caloric and fluid intake: Ensuring adequate nutrition and hydration
- Parenteral nutrition: Safe administration and monitoring for complications
9.3.6 Pain Management
- Pain assessment: Using appropriate neonatal pain scales
- Non-pharmacological measures: Swaddling, facilitated tucking, non-nutritive sucking, sucrose
- Pharmacological measures: Administration of prescribed analgesics when indicated
- Environmental modifications: Reducing noise, light, and handling to minimize stress
9.3.7 Family Support
- Education: Providing information about the infection, treatment plan, and expected course
- Involvement in care: Encouraging parents to participate in appropriate aspects of care
- Emotional support: Acknowledging concerns, providing reassurance, and facilitating coping
- Bonding promotion: Facilitating skin-to-skin contact when possible, supporting breastfeeding if appropriate
Mnemonic: “INFANTS”
To remember key nursing interventions for neonatal infections:
I – Infection control practices
N – Nutritional support
F – Fluid and electrolyte management
A – Antimicrobial administration
N – Neurological assessment
T – Thermoregulation
S – Supportive care and family support
9.4 Evaluation
Continuous evaluation of the neonate’s response to interventions is essential to determine effectiveness of treatment and adjust the care plan as needed.
9.4.1 Expected Outcomes
- Resolution of signs and symptoms of infection
- Maintenance of stable vital signs within age-appropriate parameters
- Adequate oxygenation and ventilation
- Appropriate weight gain and growth
- Tolerance of feeds
- Absence of complications
- Parent demonstration of knowledge regarding infection prevention and home care
9.4.2 Documentation
Thorough documentation should include:
- Detailed assessments and findings
- Interventions performed and neonate’s response
- Medication administration and effects
- Fluid intake and output
- Laboratory and diagnostic test results
- Communication with healthcare team members
- Family education provided and their understanding
Clinical Pearl:
When evaluating a neonate’s response to treatment for infection, remember that improvement may be gradual. Look for trends rather than focusing on isolated measurements. Persistent tachycardia despite apparent improvement in other parameters may indicate ongoing infection or complications requiring further evaluation.
10. Prevention Strategies
Prevention of neonatal infections requires a multifaceted approach addressing various risk factors across the continuum of care from pregnancy through the neonatal period. Effective preventive strategies can significantly reduce the incidence of these potentially devastating infections.
10.1 Antenatal Prevention
10.1.1 Maternal Immunization
- Tetanus toxoid: Prevents neonatal tetanus
- Influenza vaccine: Protects mother and provides passive immunity to newborn
- Pertussis vaccine (Tdap): Recommended during each pregnancy (ideally between 27-36 weeks)
- Hepatitis B vaccine: For non-immune mothers at risk
10.1.2 Screening and Treatment of Maternal Infections
- Group B Streptococcus (GBS): Universal screening at 35-37 weeks and intrapartum antibiotic prophylaxis for positive mothers
- Human immunodeficiency virus (HIV): Universal screening, antiretroviral therapy during pregnancy, and appropriate mode of delivery
- Hepatitis B: Screening and appropriate management to prevent vertical transmission
- Syphilis: Universal screening and treatment of infected mothers
- Genital herpes: Antiviral suppressive therapy for women with active lesions; consider cesarean delivery for primary infection near term
- Urinary tract infections: Screening and treatment during pregnancy
