Comprehensive Nursing Notes: Understanding Convulsions
A detailed guide for nursing students on assessment, management, and care
Table of Contents
Introduction to Convulsions
A convulsion is a medical condition where body muscles contract and relax rapidly and repeatedly, resulting in an uncontrolled shaking of the body. Convulsions are physical manifestations of abnormal electrical activity in the brain and are characterized by sudden, brief attacks of altered consciousness, motor activity, and sensory phenomena.
The terms “convulsion” and “seizure” are often used interchangeably, though technically a convulsion refers specifically to the motor components of a seizure that involve muscle contractions. Not all seizures involve convulsions, but all convulsions are considered a type of seizure.
Epilepsy is diagnosed when a person has two or more unprovoked seizures. While epilepsy always involves seizures, not all seizures indicate epilepsy. Convulsions can be isolated events triggered by various factors including high fever, head injury, or metabolic disturbances.
For nursing students, understanding the mechanisms, types, and management of convulsions is crucial for providing effective care to affected patients and potentially preventing complications or further seizure activity.
Key Terminology
- Convulsion: Uncontrolled muscle contractions causing shaking movements
- Seizure: A sudden surge of abnormal electrical activity in the brain
- Epilepsy: A chronic disorder characterized by recurrent, unprovoked seizures
- Ictal state: The period during a seizure
- Postictal state: The recovery period following a seizure
- Aura: A sensory warning that may precede a seizure
- Status epilepticus: A seizure lasting more than 5 minutes or recurrent seizures without recovery between them
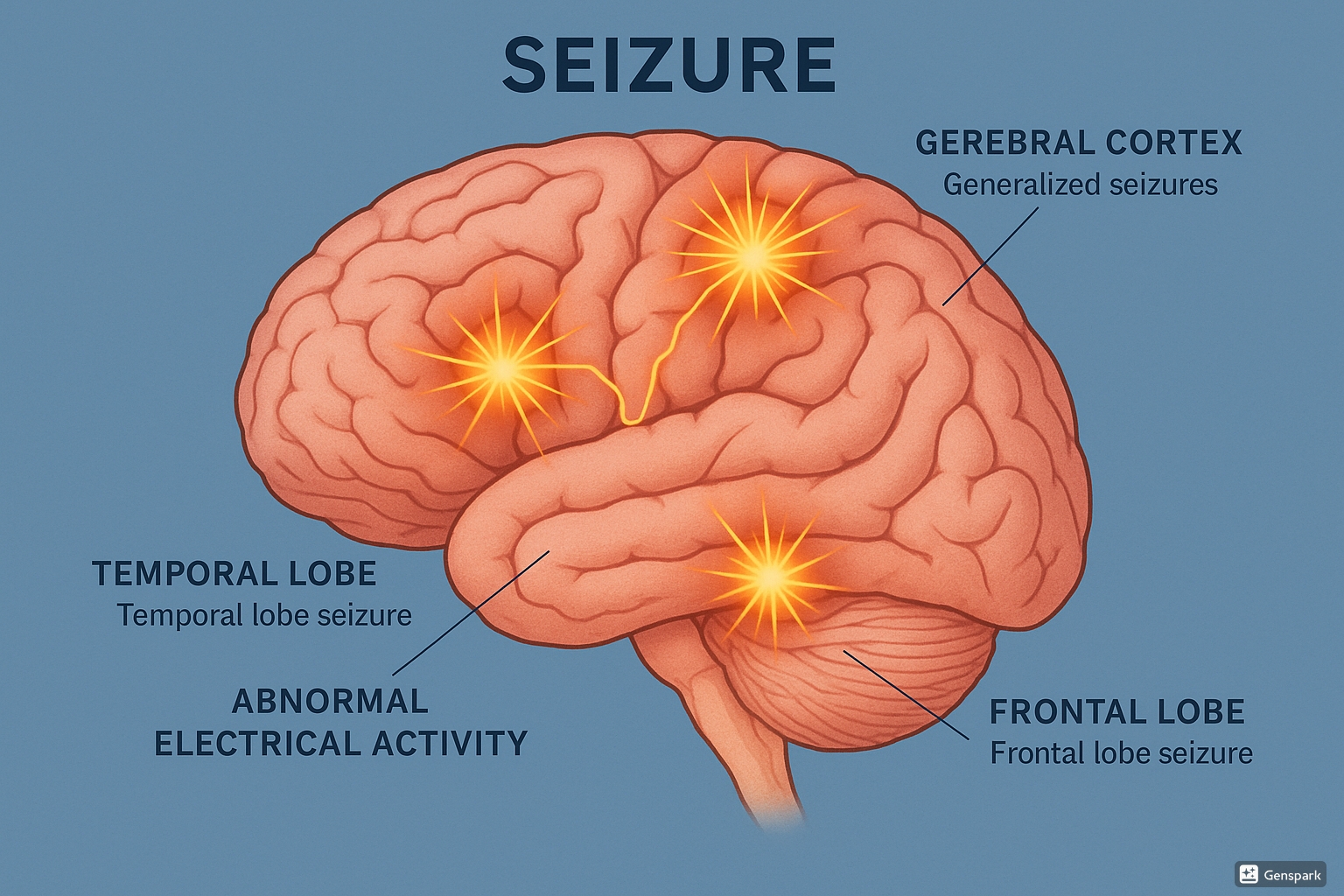
Anatomical illustration of the brain showing abnormal electrical activity during a seizure with affected brain regions labeled
Types of Convulsions/Seizures
According to the International League Against Epilepsy (ILAE) 2017 classification, seizures are categorized based on their onset, awareness level, and motor symptoms. Understanding these types helps nurses provide appropriate care and documentation.
Based on Origin
| Type | Characteristics | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|
| Focal Seizures (Partial) | Start in one area of the brain | May involve sensory symptoms, motor activity, autonomic features, or altered awareness depending on brain region affected | Observe and document specific movements or behaviors to help localize the seizure focus |
| Generalized Seizures | Involve both hemispheres of the brain from the start | Usually involve loss of consciousness, widespread motor activity | Focus on airway management, preventing injury, timing the episode |
| Unknown Onset | Origin cannot be determined | May begin with unclear signs before evolving into more recognizable patterns | Detailed observation of sequence of events is crucial for later diagnosis |
Focal Seizures Subtypes
Focal Aware Seizures
Formerly called simple partial seizures
- Consciousness is preserved
- Patient remains alert and can recall events
- May experience motor symptoms (rhythmic movements), sensory symptoms (unusual smells, tastes), or autonomic symptoms (racing heart, stomach discomfort)
- Usually brief (seconds to minutes)
Focal Impaired Awareness Seizures
Formerly called complex partial seizures
- Consciousness is impaired
- Patient appears confused or dazed
- May perform repetitive movements (automatisms) like lip-smacking, chewing, or fidgeting
- Typically last 1-2 minutes
- Followed by confusion and memory gap for the event
Generalized Seizures Subtypes
| Type | Characteristics | Duration | Nursing Considerations |
|---|---|---|---|
| Tonic-Clonic (Grand Mal) | Initial stiffening (tonic phase) followed by rhythmic jerking (clonic phase); loss of consciousness; may have urinary/bowel incontinence | 1-3 minutes | Protect from injury, time the seizure, maintain airway, position on side after seizure, expect postictal confusion |
| Absence (Petit Mal) | Brief staring episodes; minimal or no motor movement; abrupt onset and cessation | 5-30 seconds | May be mistaken for daydreaming; important to document frequency; minimal postictal confusion |
| Myoclonic | Brief, shock-like muscle jerks of the face, trunk, or extremities | Seconds | Differentiate from normal startle responses; may occur in clusters |
| Tonic | Sustained muscle stiffening without clonic phase | <1 minute | High risk for falls; protect head; may cause vocalization from air forced through vocal cords |
| Atonic (Drop Attacks) | Sudden loss of muscle tone causing falls | <15 seconds | High risk for head injury; protective helmets may be needed; rapid recovery |
| Clonic | Rhythmic jerking movements without initial tonic component | Variable | Less common than tonic-clonic; protect from injury during movements |
Special Consideration: Status Epilepticus
Status epilepticus is a medical emergency defined as:
- A seizure lasting longer than 5 minutes, OR
- Multiple seizures without full recovery of consciousness between them
This condition requires immediate medical intervention to prevent neurological damage and other life-threatening complications.
Causes of Convulsions
Provoked Seizures
Provoked (acute symptomatic) seizures occur due to a specific trigger and may not recur when the trigger is removed.
- Metabolic disturbances: Hypoglycemia, hyponatremia, hypocalcemia, uremia
- Toxic: Alcohol withdrawal, drug overdose or withdrawal, carbon monoxide poisoning
- High fever: Particularly in children (febrile seizures)
- Acute infection: Meningitis, encephalitis, brain abscess
- Acute head trauma: Concussion, contusion, intracranial hemorrhage
- Sleep deprivation: Can lower seizure threshold
- Medication reactions: Some antibiotics, antipsychotics, stimulants
Unprovoked Seizures
Unprovoked seizures occur without an immediate identifiable cause and may indicate epilepsy if recurrent.
- Genetic factors: Family history of epilepsy, genetic syndromes
- Congenital abnormalities: Brain malformations, cortical dysplasia
- Acquired brain injuries: Previous stroke, traumatic brain injury
- Tumors: Primary brain tumors, metastatic lesions
- Neurodegenerative disorders: Alzheimer’s disease, multiple sclerosis
- Perinatal injuries: Birth trauma, hypoxic-ischemic encephalopathy
- Remote infections: Previous CNS infections leaving scarring
- Idiopathic: No identifiable cause (approximately 50% of epilepsy cases)
Risk Factors for Developing Epilepsy
- Family history of epilepsy
- History of febrile seizures in childhood
- Head trauma, especially with loss of consciousness
- CNS infections (meningitis, encephalitis)
- Stroke or cerebrovascular disease
- Brain tumors or abnormal brain structures
- Neurodevelopmental disorders
- Alzheimer’s disease and other dementias
- Autism spectrum disorder
- Advanced age (>65 years)
Mnemonic: “VITAMIN” for Common Seizure Causes
- V – Vascular (stroke, hemorrhage)
- I – Infections (meningitis, encephalitis)
- T – Trauma (head injuries)
- A – AV Malformations (arteriovenous abnormalities)
- M – Metabolic (electrolyte imbalances, hypoglycemia)
- I – Idiopathic (unknown causes)
- N – Neoplasms (tumors)
Pathophysiology of Convulsions
Understanding the pathophysiology of convulsions is essential for comprehending seizure manifestations and their management. Convulsions result from abnormal, excessive, and hypersynchronous electrical discharges from neurons in the brain.
Normal Neuronal Activity
In normal brain function, there is a delicate balance between excitatory and inhibitory neurotransmission:
- Excitatory neurotransmitters: Primarily glutamate, which stimulates neurons to fire action potentials
- Inhibitory neurotransmitters: Primarily GABA (gamma-aminobutyric acid), which inhibits neuronal activity
This balance allows for controlled information processing and normal brain function.
Seizure Development
During a seizure, this balance is disrupted, leading to:
- Excessive excitation (increased glutamate activity)
- Decreased inhibition (reduced GABA effectiveness)
- Alterations in ion channels (especially sodium, potassium, and calcium)
- Hypersynchronization of neuronal networks
- Formation of an epileptogenic focus (area where seizures originate)
The Seizure Process
- Initiation: Triggered by factors that lower seizure threshold or by spontaneous activity in an epileptogenic focus
- Paroxysmal Depolarization Shifts (PDS): Neurons begin to fire abnormally, creating bursts of high-frequency discharges
- Propagation: The abnormal electrical activity spreads to neighboring neurons through synaptic and non-synaptic mechanisms
-
Clinical manifestation: As different brain regions become involved, specific symptoms appear based on the affected areas:
- Motor cortex involvement → convulsive movements
- Sensory cortex involvement → sensory symptoms
- Widespread involvement → loss of consciousness
-
Termination: Eventually inhibitory mechanisms overcome excitation, ending the seizure through:
- Neurotransmitter depletion
- Energy substrate depletion
- Activation of inhibitory mechanisms
- Changes in ion channel properties
Metabolic Changes During Prolonged Seizures
Status epilepticus causes significant physiological changes:
Cerebral Effects
- Increased cerebral metabolic demand
- Increased cerebral blood flow initially
- Decreased cerebral blood flow later
- Cerebral edema
- Neuronal damage and death
Systemic Effects
- Lactic acidosis
- Hyperthermia
- Respiratory compromise
- Increased catecholamine levels
- Rhabdomyolysis
- Hypoglycemia
Postictal State
- Neuronal exhaustion
- GABA-mediated inhibition
- Altered consciousness
- Muscle soreness
- Confusion and disorientation
- Todd’s paralysis (temporary weakness)
Understanding this pathophysiology helps nurses recognize why certain symptoms occur during and after convulsions, as well as the rationale behind various treatment approaches, particularly the mechanisms of action for antiseizure medications.
Assessment of Patients with Convulsions
A comprehensive assessment is crucial for patients experiencing convulsions. Nurses play a vital role in collecting accurate information that will guide diagnosis and treatment.
History Taking
Mnemonic: “TDOC” for Seizure Documentation
- T – Type of seizure (observed characteristics)
- D – Duration (how long the seizure lasted)
- O – Onset (how the seizure began, any warning signs)
- C – Complications (any injuries, breathing issues, etc.)
Key Questions to Ask
- For witnessed seizures:
- What happened first? (aura, warning signs)
- Which body parts were involved? (focal vs. generalized onset)
- Was consciousness affected? (aware vs. impaired awareness)
- How long did it last?
- What happened after the seizure? (postictal state)
- Patient history:
- Previous seizures or diagnosis of epilepsy?
- Family history of seizures?
- Recent head trauma?
- Current medications and compliance?
- Recent illness or fever?
- Alcohol or drug use?
- Sleep patterns?
- Stress levels?
Physical Examination
During a Seizure
- Vital signs: Monitor for changes in BP, HR, RR, temperature
- Level of consciousness: Document any changes
- Motor activity: Type, location, progression of movements
- Eyes: Position, movement, pupil size and reactivity
- Color: Note cyanosis or pallor
- Incontinence: Document if present
- Autonomic signs: Salivation, sweating, flushing
- Duration: Time the seizure accurately
Post-Seizure Assessment
- Neurological status: Use Glasgow Coma Scale
- Orientation: Person, place, time, situation
- Motor function: Strength, symmetry, Todd’s paralysis
- Vital signs: Continue monitoring
- Injuries: Check for trauma, especially to head and tongue
- Mental status: Confusion, memory, speech
- Respiratory status: Breathing pattern, oxygen saturation
- Pain: Headache, muscle pain
Diagnostic Tests
| Diagnostic Test | Purpose | Nursing Considerations |
|---|---|---|
| Electroencephalogram (EEG) | Records brain’s electrical activity; can identify seizure type and focus |
|
| Brain Imaging (CT, MRI) |
Identifies structural abnormalities like tumors, malformations, stroke, trauma |
|
| Blood Tests | CBC, electrolytes, glucose, calcium, magnesium, drug levels, toxicology screen |
|
| Lumbar Puncture | To rule out CNS infection in cases with fever or suspected meningitis/encephalitis |
|
Warning Signs Requiring Immediate Medical Attention
- Seizure lasting more than 5 minutes
- Multiple seizures without regaining consciousness
- Breathing difficulties during or after seizure
- Seizure occurring in water
- First-time seizure without identified cause
- Seizure in pregnant women
- Significant injury during seizure
- Prolonged post-ictal confusion (>30 minutes)
Nursing Care and Management
Nursing care for patients experiencing convulsions focuses on patient safety, preventing complications, and providing support during and after seizure episodes.
During a Seizure
DO
- Time the seizure from beginning to end
- Stay with the patient throughout the seizure
- Protect the patient from injury by removing harmful objects
- Gently guide the patient to the floor if standing or sitting
- Place something soft under the head
- Turn the patient to their side (recovery position) to prevent aspiration
- Loosen tight clothing, especially around the neck
- Stay calm and reassure others nearby
- Document seizure characteristics
- Call for medical assistance if seizure lasts >5 minutes
DON’T
- Do not restrain the patient’s movements
- Do not put anything in the patient’s mouth
- Do not try to hold the tongue
- Do not offer food or water until fully alert
- Do not attempt to move the patient unless in danger
- Do not leave the patient alone during or immediately after a seizure
After a Seizure (Postictal Care)
Immediate Care
- Maintain the recovery position until consciousness returns
- Perform thorough neurological assessment
- Check vital signs
- Assess for injuries sustained during seizure
- Suction airway if necessary
- Administer oxygen if indicated
- Monitor respiration and cardiac status
- Reorient the patient as consciousness returns
Ongoing Care
- Allow the patient to rest in a quiet environment
- Maintain privacy and dignity
- Provide emotional support
- Assist with hygiene if incontinence occurred
- Document postictal state and recovery time
- Observe for signs of status epilepticus
- Administer medications as prescribed
- Prepare for diagnostic tests
Seizure Precautions
Implementing seizure precautions is essential for patients at risk of convulsions. These include:
- Padded side rails when in bed
- Bed in lowest position
- Call bell within easy reach
- Avoid sharp objects in the patient’s environment
- Oxygen and suction equipment readily available
- IV access maintained for emergency medication administration
- Frequent monitoring
- Supervision during activities such as bathing
- Clear pathways in room to prevent injury
- Identifying and minimizing seizure triggers when possible
Patient Education
Key Educational Topics
For the Patient:
- Importance of medication adherence
- Recognition of seizure triggers
- Safety precautions at home
- Lifestyle modifications (sleep, stress management)
- When to seek medical attention
- Importance of wearing medical ID
- Driving restrictions and legal implications
- Employment considerations
For Family Members/Caregivers:
- Seizure first aid
- When to call emergency services
- How to maintain a seizure diary
- Administration of rescue medications
- Creating a safe home environment
- Supporting medication compliance
- Managing social stigma
- Resources for support groups
Special Considerations for Specific Populations
Children
- Age-appropriate explanation of seizures
- School coordination and education
- Addressing developmental concerns
- Involving parents in care
- Medication administration strategies
Pregnant Women
- Medication adjustments
- Fetal monitoring
- Birth planning
- Breastfeeding considerations
- Risk assessments
Older Adults
- Fall prevention strategies
- Medication interactions
- Cognitive assessment
- Home safety modifications
- Caregiver support
Nursing Care Plans
Effective nursing care for patients with convulsions requires structured care plans addressing key nursing diagnoses. Here are comprehensive nursing care plans for the most common diagnoses in patients with seizure disorders.
Nursing Diagnosis: Risk for Injury
Related Factors
- Altered consciousness during seizure activity
- Uncontrolled movements during convulsions
- Postictal confusion
- Environmental hazards
Expected Outcomes
- Patient will remain free from injury during seizure episodes
- Patient will identify and modify environmental risk factors
- Patient will verbalize understanding of safety precautions
Nursing Interventions
| Intervention | Rationale |
|---|---|
| Implement seizure precautions (padded side rails, bed in lowest position, clear pathways) | Reduces risk of trauma during seizure activity |
| Remove potential hazards from environment when seizure activity begins | Prevents injury from hard or sharp objects |
| Place patient in side-lying position during seizure if possible | Reduces risk of aspiration and maintains airway patency |
| Educate patient and family about home safety modifications (e.g., padded furniture corners, carpet instead of hard flooring, shower chairs) | Promotes safety in the home environment |
| Educate about activities requiring supervision (bathing, swimming, cooking) | Prevents injury during activities with higher risk |
Evaluation
- Patient remains free from injury during hospital stay
- Patient and family demonstrate understanding of safety precautions
- Patient verbalizes plan for home safety measures
Nursing Diagnosis: Ineffective Airway Clearance
Related Factors
- Excessive secretions during seizure
- Altered consciousness affecting gag and cough reflexes
- Potential for tongue obstruction
- Risk of aspiration
Expected Outcomes
- Patient will maintain patent airway during and after seizure episodes
- Patient will demonstrate adequate oxygenation as evidenced by normal respiratory rate and oxygen saturation
- Patient will remain free from signs of aspiration
Nursing Interventions
| Intervention | Rationale |
|---|---|
| Position patient in lateral recumbent position during seizure when possible | Facilitates drainage of secretions and prevents tongue from blocking airway |
| Have suction equipment readily available | Enables quick removal of secretions to maintain airway patency |
| Monitor respiratory rate, pattern, and oxygen saturation | Provides early detection of respiratory compromise |
| Administer oxygen as prescribed | Improves oxygenation during periods of increased demand |
| Assess for signs of aspiration (crackles, decreased oxygen saturation, fever) | Early identification allows prompt intervention |
Evaluation
- Patient maintains patent airway throughout seizure episodes
- Oxygen saturation remains above 95%
- No evidence of aspiration pneumonia
Nursing Diagnosis: Deficient Knowledge
Related Factors
- New diagnosis of seizure disorder
- Lack of exposure to information about seizure management
- Misinterpretation of information
- Cognitive limitations
Expected Outcomes
- Patient will verbalize understanding of seizure disorder, triggers, and management
- Patient will demonstrate correct medication administration
- Patient will identify when to seek medical attention
- Family members will demonstrate appropriate first aid for seizures
Nursing Interventions
| Intervention | Rationale |
|---|---|
| Assess patient’s and family’s current knowledge of seizure disorder | Establishes baseline for education and identifies misconceptions |
| Provide information about type of seizures, triggers, and treatment options | Builds understanding of the condition and promotes participation in care |
| Teach proper administration of antiepileptic medications, including dosing schedule, side effects, and importance of adherence | Promotes medication compliance and therapeutic effectiveness |
| Demonstrate seizure first aid to family members and caregivers | Prepares them to respond appropriately during seizure episodes |
| Provide written materials and resources for continued learning | Reinforces verbal teaching and serves as reference |
Evaluation
- Patient correctly explains seizure disorder and management
- Patient demonstrates proper medication administration
- Family members correctly describe and demonstrate seizure first aid
- Patient identifies appropriate circumstances for seeking medical attention
Nursing Diagnosis: Disturbed Body Image
Related Factors
- Social stigma associated with seizures
- Unpredictability of seizure occurrence
- Loss of control during seizures
- Medication side effects (weight gain, hair changes)
Interventions
- Encourage expression of feelings about diagnosis
- Provide accurate information to counter stigma
- Connect patient with support groups
- Discuss strategies for maintaining privacy and dignity
- Address medication side effects and management
Nursing Diagnosis: Anxiety
Related Factors
- Fear of having seizures in public
- Uncertainty about prognosis
- Concerns about independence
- Lifestyle restrictions (driving, work limitations)
Interventions
- Provide emotional support and active listening
- Teach stress reduction techniques
- Help identify coping strategies
- Educate about seizure control methods
- Refer to counseling or support services if needed
Documentation Guidelines
Complete and accurate documentation is essential for continuity of care. Include:
- Detailed description of seizure activity using objective terms
- Time of onset and duration
- Interventions performed and patient’s response
- Vital signs before (if possible), during, and after seizure
- Medications administered
- Postictal state and recovery time
- Any injuries or complications
- Patient and family education provided
- Referrals made
Medication Management
Pharmacological management is a cornerstone of seizure control. Nurses play a vital role in medication administration, monitoring for therapeutic effects and side effects, and patient education.
Classes of Antiepileptic Drugs (AEDs)
| Drug Class | Common Medications | Primary Mechanism | Common Side Effects | Nursing Considerations |
|---|---|---|---|---|
| Sodium Channel Blockers | Phenytoin (Dilantin) Carbamazepine (Tegretol) Lamotrigine (Lamictal) Oxcarbazepine (Trileptal) |
Block sodium channels to limit rapid repetitive firing of action potentials | Dizziness, ataxia, diplopia, nausea, rash, gingival hyperplasia (phenytoin) |
|
| GABA Enhancers | Benzodiazepines (diazepam, lorazepam) Phenobarbital Vigabatrin Tiagabine |
Enhance inhibitory GABA effects by various mechanisms | Sedation, cognitive impairment, respiratory depression, dependence |
|
| Multiple Mechanisms | Valproic acid (Depakote) Levetiracetam (Keppra) Topiramate (Topamax) Zonisamide |
Multiple or complex mechanisms including GABA enhancement, glutamate inhibition, and ion channel modulation | Tremor, weight gain/loss, hair loss, mood changes, kidney stones |
|
| Calcium Channel Modulators | Ethosuximide (Zarontin) Gabapentin (Neurontin) Pregabalin (Lyrica) |
Modulate calcium channels to reduce neuronal excitability | Dizziness, somnolence, peripheral edema |
|
Emergency Medications for Status Epilepticus
Status epilepticus is a medical emergency requiring prompt intervention with the following medication sequence:
-
First Line (0-5 minutes): Benzodiazepines
- Lorazepam 4 mg IV (may repeat once in 5-10 minutes)
- Diazepam 10 mg IV (may repeat once in 5-10 minutes)
- Midazolam 10 mg IM/IV/buccal (if no IV access)
-
Second Line (5-20 minutes): If seizures continue
- Fosphenytoin 20 mg PE/kg IV (max 1500 mg PE)
- Valproic acid 40 mg/kg IV (max 3000 mg)
- Levetiracetam 60 mg/kg IV (max 4500 mg)
-
Third Line (20-40 minutes): Refractory status epilepticus
- General anesthesia with:
- Propofol
- Midazolam continuous infusion
- Pentobarbital/thiopental
- Requires intubation and ICU care with continuous EEG monitoring
- General anesthesia with:
Nursing Priorities During Status Epilepticus
- Accurately time seizure duration
- Ensure patent airway and oxygenation
- Establish IV access promptly
- Administer medications as ordered without delay
- Monitor vital signs continuously
- Prepare for potential intubation and ICU transfer
- Collect blood samples for diagnostic tests
Medication Administration Considerations
Nursing Responsibilities
- Verify correct drug and dosage before administration
- Assess for drug allergies and interactions
- Monitor therapeutic drug levels as ordered
- Be alert for signs of toxicity
- Evaluate medication effectiveness in reducing seizure frequency
- Document response to medications
- Understand that abrupt discontinuation of AEDs can trigger seizures
- Monitor and report side effects promptly
- Evaluate for drug-drug interactions
Patient Education
- Explain purpose and expected benefits of medications
- Stress importance of taking medications as prescribed
- Teach about common and serious side effects
- Explain importance of regular blood tests
- Advise against abrupt discontinuation
- Discuss potential drug interactions with OTC medications
- Address concerns about long-term medication use
- Provide strategies for maintaining medication adherence
- Teach women of childbearing age about pregnancy considerations
Special Considerations
Pediatric Patients
- Weight-based dosing critical
- Consider liquid formulations
- Monitor growth and development
- School administration plans
Pregnant Women
- Avoid valproate if possible
- Folic acid supplementation
- Risk-benefit assessment
- Possible dose adjustments throughout pregnancy
Older Adults
- Start low, go slow with dosing
- Monitor for cognitive effects
- Assess fall risk
- Check for drug interactions
Prevention Strategies
While not all seizures and convulsions can be prevented, certain strategies can reduce their occurrence and impact. According to the World Health Organization, approximately 25% of epilepsy cases are potentially preventable.
Primary Prevention
Strategies to prevent the development of seizure disorders:
- Prevent head injuries
- Wear helmets during sports and recreational activities
- Use seat belts and proper child car seats
- Prevent falls, especially in older adults and children
- Avoid driving under the influence of alcohol or drugs
- Reduce risk of stroke
- Manage hypertension, diabetes, and high cholesterol
- Maintain a healthy diet and exercise regularly
- Avoid tobacco products
- Limit alcohol consumption
- Prevent CNS infections
- Complete recommended vaccination schedules
- Practice good hygiene and food safety
- Prevent parasitic infections like cysticercosis
- Seek prompt treatment for suspected infections
- Adequate prenatal and perinatal care
- Regular prenatal check-ups
- Proper nutrition during pregnancy
- Avoiding alcohol and drugs during pregnancy
- Skilled birth attendance to reduce birth injuries
Secondary Prevention
Strategies to prevent seizures in individuals with epilepsy:
- Medication adherence
- Take antiepileptic drugs as prescribed
- Use reminders and pill organizers
- Don’t abruptly discontinue medications
- Attend follow-up appointments for monitoring
- Seizure trigger avoidance
- Maintain regular sleep patterns
- Manage stress effectively
- Avoid alcohol and recreational drugs
- For photosensitive epilepsy, avoid flashing lights
- Dietary considerations
- Regular meal times to prevent hypoglycemia
- Ketogenic diet (for some refractory cases)
- Limit caffeine intake
- Ensure adequate hydration
- Lifestyle management
- Regular physical activity (with appropriate precautions)
- Stress reduction techniques
- Adequate rest and recovery
- Monitor for illness and fever
Nursing Role in Prevention
Education
- Teach about seizure triggers and avoidance
- Explain medication mechanisms and importance
- Provide resources on seizure first aid
- Address misconceptions about epilepsy
Monitoring
- Assess for medication side effects
- Monitor therapeutic drug levels
- Track seizure frequency and patterns
- Evaluate effectiveness of interventions
Advocacy
- Promote public awareness about epilepsy
- Support helmet use and injury prevention
- Connect patients to support resources
- Advocate for accessible epilepsy care
Emerging Prevention Approaches
- Seizure Prediction Devices: Wearable technology that can detect patterns and warn of impending seizures
- Neurostimulation: Vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation for seizure prevention
- Genetic Counseling: For families with hereditary forms of epilepsy
- Digital Health Tools: Apps for medication adherence, trigger tracking, and seizure diaries
- Telehealth Monitoring: Remote patient monitoring for early intervention
Mnemonic: “STOP SEIZURE” for Seizure Prevention
- Stress management
- Trauma prevention (head injuries)
- Overexertion avoidance
- Proper medication adherence
- Sleep adequately and regularly
- Electrolyte balance maintenance
- Illness management (especially fever)
- Zealous avoidance of triggers (like flashing lights)
- Understand proper medication dosing
- Recreational drugs and alcohol avoidance
- Education about seizure management
Helpful Mnemonics
Mnemonics are valuable tools for nursing students to remember key information about convulsions and seizures. Here are several useful memory aids:
Causes of Seizures: “VITAMIN”
- V – Vascular (stroke, hemorrhage)
- I – Infections (meningitis, encephalitis)
- T – Trauma (head injuries)
- A – AV Malformations
- M – Metabolic (electrolyte imbalances, hypoglycemia)
- I – Idiopathic (unknown causes)
- N – Neoplasms (tumors)
Seizure Documentation: “TDOC”
- T – Type of seizure
- D – Duration of seizure
- O – Onset (how it began)
- C – Complications (injuries, breathing issues)
Essential for accurate documentation and communication with healthcare team.
Types of Generalized Seizures: “MATCH”
- M – Myoclonic (brief jerks)
- A – Atonic (sudden loss of muscle tone)
- T – Tonic (stiffening)
- C – Clonic (rhythmic jerking)
- H – Hybrid (tonic-clonic)
(Absence seizures don’t fit the mnemonic but are also generalized)
Emergency Seizure Management: “ABCDE”
- A – Airway (ensure it’s patent)
- B – Breathing (monitor respiration)
- C – Circulation (check pulse and BP)
- D – Duration (time the seizure)
- E – Environment (make it safe)
Status Epilepticus Care: “TIME”
- T – Time the seizure (>5 minutes is status epilepticus)
- I – IV access (establish immediately)
- M – Medication (administer benzodiazepines)
- E – Ensure airway protection and oxygenation
Postictal Assessment: “AWARE”
- A – Airway patency
- W – Wakefulness level
- A – Assess for injuries
- R – Reorientation needed?
- E – Evaluate neurological status
Patient Education: “TEACH”
- T – Triggers identification and avoidance
- E – Emergency protocols and first aid
- A – Antiepileptic drug administration and compliance
- C – Complication prevention and safety measures
- H – Healthcare follow-up importance
Statistics and Facts
Understanding the epidemiology and statistical data related to convulsions and epilepsy helps nurses contextualize the significance of this condition and provides valuable information for patient education.
Global Prevalence and Incidence
- Approximately 50 million people worldwide have epilepsy, making it one of the most common neurological diseases globally
- Nearly 80% of people with epilepsy live in low- and middle-income countries
- About 5 million people are diagnosed with epilepsy each year
- The incidence rate ranges from 16 to 51 per 100,000 person-years in high-income countries and up to 139 per 100,000 in low- and middle-income countries
- The lifetime risk of developing epilepsy is approximately 1 in 26 people
Demographics and Risk Factors
- Epilepsy affects all age groups, but incidence is highest in young children and adults over 60
- Males are slightly more likely than females to develop epilepsy
- Approximately 50% of epilepsy cases have no identified cause
- In the United States, about 3.4 million people (3 million adults and 470,000 children) have active epilepsy
- 2-5% of children will experience at least one febrile seizure before age 5
- Up to 10% of people worldwide will have at least one seizure during their lifetime
Treatment and Outcomes
- With appropriate treatment, up to 70% of people with epilepsy could become seizure-free
- However, about 75% of people with epilepsy in low-income countries do not receive the treatment they need (treatment gap)
- After 2 years seizure-free, many patients can consider discontinuing medications
- About 30% of patients have drug-resistant epilepsy that does not respond to medication
- Surgical interventions can help 60-70% of carefully selected patients with drug-resistant epilepsy
- The risk of recurrence after a first unprovoked seizure is approximately 40-50%
Impact and Burden
- People with epilepsy have a 2-3 times higher risk of premature death compared to the general population
- Approximately 25% of epilepsy cases are potentially preventable
- Epilepsy accounts for more than 0.5% of the global burden of disease
- Status epilepticus has a mortality rate of 20% if not treated promptly
- People with epilepsy often experience stigma and discrimination, affecting education, employment, relationships, and overall quality of life
- The economic burden of epilepsy in the United States is estimated at $15.5 billion annually in direct and indirect costs
Key Facts About Convulsions
- Not all seizures include convulsions – only about 60% of seizures involve convulsive movements
- Tonic-clonic (grand mal) seizures are the most recognized form of convulsive seizures
- A convulsive seizure typically lasts 1-3 minutes
- More than 5 minutes of continuous convulsions constitutes a medical emergency (status epilepticus)
- Febrile seizures (often convulsive) affect 2-5% of children and are usually benign
- While frightening to witness, most convulsive seizures do not cause brain damage
- The risk of sudden unexpected death in epilepsy (SUDEP) is about 1 in 1,000 per year for people with epilepsy
- Convulsive seizures can also occur in non-epileptic conditions such as psychogenic non-epileptic seizures (PNES)
References
- World Health Organization. (2023). Epilepsy Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/epilepsy
- Centers for Disease Control and Prevention. (2023). Epilepsy: Prevention. https://www.cdc.gov/epilepsy/prevention/index.html
- Fisher, R. S., Cross, J. H., French, J. A., Higurashi, N., Hirsch, E., Jansen, F. E., Lagae, L., Moshé, S. L., Peltola, J., Roulet Perez, E., Scheffer, I. E., & Zuberi, S. M. (2017). Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology. Epilepsia, 58(4), 522–530.
- Nurse Together. (2022). Seizure: Nursing Diagnoses, Care Plans, Assessment & Interventions. https://www.nursetogether.com/seizure-nursing-diagnosis-care-plan/
- Nurseslabs. (2023). 6 Seizure Disorder Nursing Care Plans. https://nurseslabs.com/seizure-disorder-nursing-care-plans/
- Registered Nurse RN. (2022). Seizures (Epilepsy) NCLEX Review. https://www.registerednursern.com/seizures-epilepsy-nclex-review/
- Huff, J. S., Murr, N. (2023). Seizure. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430765/
- Kapur, J., Elm, J., Chamberlain, J. M., Barsan, W., Cloyd, J., Lowenstein, D., … & NETT and PECARN Investigators. (2019). Randomized trial of three anticonvulsant medications for status epilepticus. New England Journal of Medicine, 381(22), 2103-2113.
- American Epilepsy Society. (2023). Guidelines for the evaluation and management of status epilepticus. Epilepsy Currents, 16(1), 48-61.
- Brophy, G. M., Bell, R., Claassen, J., Alldredge, B., Bleck, T. P., Glauser, T., … & Neurocritical Care Society Status Epilepticus Guideline Writing Committee. (2012). Guidelines for the evaluation and management of status epilepticus. Neurocritical Care, 17(1), 3-23.
