Abnormal Uterine Bleeding
Comprehensive Nursing Assessment & Management Guide
Overview & Definition
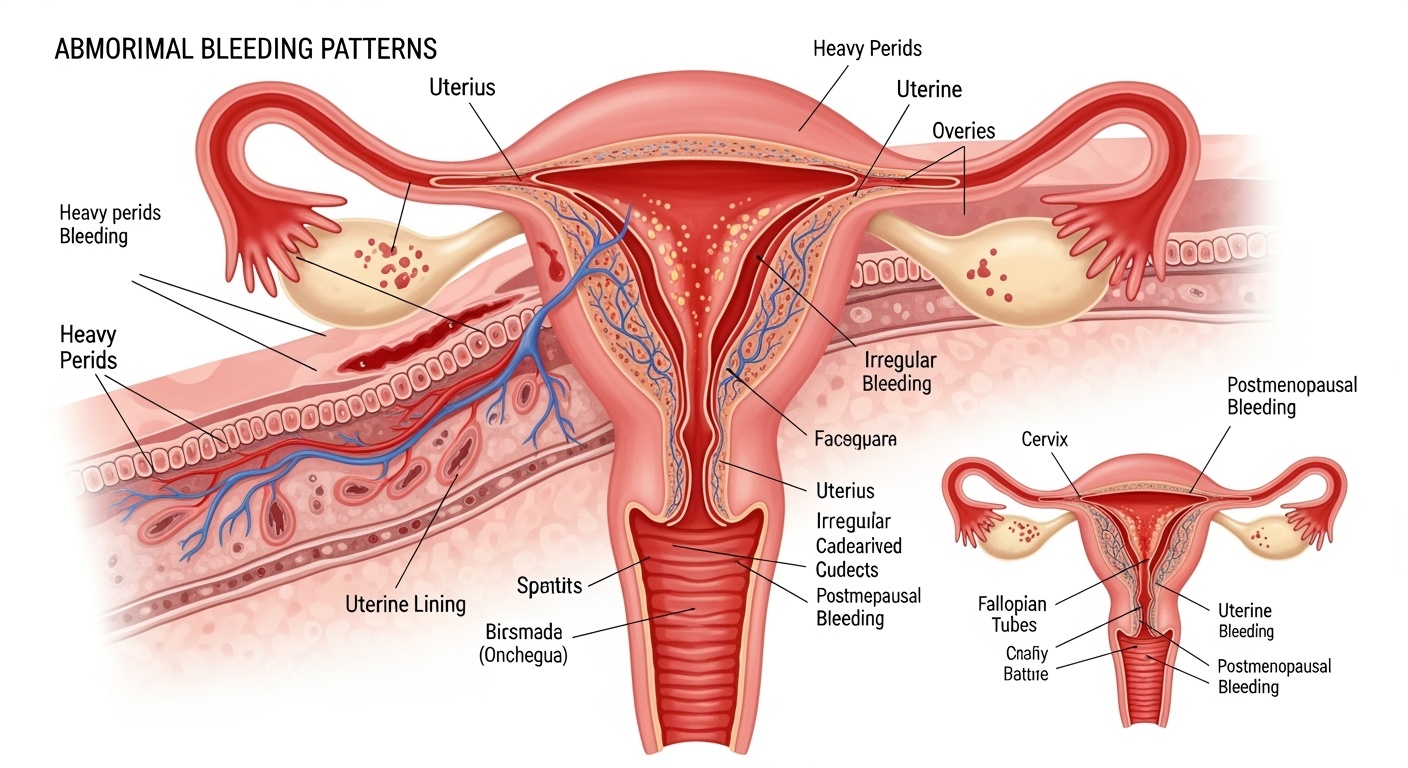
Abnormal uterine bleeding represents one of the most common gynecological concerns encountered in clinical practice, affecting approximately 14-25% of women of reproductive age. This condition encompasses any deviation from normal menstrual patterns, including changes in frequency, duration, volume, or regularity of menstrual cycles.
As nursing professionals, understanding abnormal uterine bleeding is crucial for providing comprehensive women’s health care. The condition significantly impacts quality of life, causing physical discomfort, emotional distress, and potential complications such as anemia or infertility. Early recognition and appropriate nursing interventions can dramatically improve patient outcomes and prevent serious complications.
Clinical Definition
Abnormal uterine bleeding is defined as bleeding from the uterine corpus that differs from normal menstruation in frequency, regularity, duration, or volume. This includes bleeding that occurs outside the normal menstrual cycle or bleeding patterns that deviate significantly from the individual’s established menstrual pattern.
FIGO Classification System
The International Federation of Gynecology and Obstetrics (FIGO) established a comprehensive classification system for abnormal uterine bleeding, providing standardized terminology that enhances communication among healthcare providers and improves patient care consistency.
| Classification Category | Definition | Clinical Examples |
|---|---|---|
| Heavy Menstrual Bleeding | Excessive menstrual blood loss interfering with quality of life | Flow >80ml per cycle, changing protection hourly |
| Intermenstrual Bleeding | Bleeding between regular menstrual periods | Spotting mid-cycle, breakthrough bleeding |
| Postmenopausal Bleeding | Any bleeding 12+ months after menopause | Vaginal bleeding in postmenopausal women |
| Irregular Menstruation | Unpredictable timing of menstrual cycles | Cycles varying >20 days from norm |
Acute Abnormal Uterine Bleeding
Episodes requiring immediate intervention to prevent further blood loss. Often presents with hemodynamic instability and requires urgent medical attention.
Chronic Abnormal Uterine Bleeding
Bleeding patterns that have been abnormal for most of the previous 6 months. Allows for systematic evaluation and planned management approaches.
Causes & Etiology – PALM-COEIN Framework
The PALM-COEIN classification system provides a systematic approach to understanding the various causes of abnormal uterine bleeding. This framework divides causes into structural (PALM) and non-structural (COEIN) categories, facilitating comprehensive assessment and targeted treatment.
PALM – Structural Causes
P – Polyps
Endometrial or cervical polyps causing irregular bleeding patterns
A – Adenomyosis
Endometrial tissue growing into uterine muscle wall
L – Leiomyomas
Uterine fibroids affecting menstrual flow and duration
M – Malignancy/Hyperplasia
Endometrial cancer or atypical hyperplasia
COEIN – Non-Structural Causes
C – Coagulopathy
Inherited or acquired bleeding disorders
O – Ovulatory Dysfunction
Hormonal imbalances affecting ovulation
E – Endometrial
Primary endometrial disorders
I – Iatrogenic
Medication-related bleeding
N – Not Yet Classified
Other rare or undefined causes
Common Risk Factors
Reproductive Factors
- • Early menarche or late menopause
- • Nulliparity or low parity
- • PCOS or metabolic disorders
Medical Conditions
- • Thyroid dysfunction
- • Diabetes mellitus
- • Liver or kidney disease
Lifestyle Factors
- • Obesity or rapid weight changes
- • Excessive exercise
- • Stress and psychological factors
Comprehensive Nursing Assessment
Systematic nursing assessment of abnormal uterine bleeding requires thorough history-taking, physical examination, and careful documentation. The assessment should focus on characterizing bleeding patterns, identifying potential causes, and evaluating the impact on the patient’s physical and emotional well-being.
Menstrual History Assessment
Cycle Characteristics
Frequency, duration, volume, and regularity patterns
Timing Patterns
Onset, interval changes, relationship to activities
Flow Assessment
Quantification using standardized tools and patient reports
Associated Symptoms
Pain Assessment
Dysmenorrhea, pelvic pain, cramping intensity
Systemic Symptoms
Fatigue, weakness, dizziness, syncope
Impact on Quality of Life
Work, social activities, sexual function, emotional health
| Assessment Component | Key Questions | Clinical Significance |
|---|---|---|
| Bleeding Pattern | How often? How long? How heavy? Clots present? | Helps classify type of abnormal uterine bleeding |
| Reproductive History | Pregnancies, births, contraceptive use, sexual activity | Identifies pregnancy-related and contraceptive causes |
| Medical History | Chronic conditions, medications, previous procedures | Reveals underlying systemic causes |
| Family History | Bleeding disorders, cancer, reproductive issues | Identifies genetic predispositions and risk factors |
Diagnostic Workup & Laboratory Studies
Comprehensive diagnostic evaluation of abnormal uterine bleeding involves a systematic approach combining laboratory studies, imaging, and specialized procedures. The extent of workup depends on patient age, bleeding severity, and clinical presentation.
Initial Laboratory Panel
- Complete Blood Count (CBC)
- Iron studies and ferritin
- Pregnancy test (βhCG)
- Thyroid function tests
- Coagulation studies (if indicated)
Imaging Studies
- Transvaginal ultrasound
- Saline infusion sonography
- MRI (if indicated)
- Hysteroscopy
- CT scan (specific cases)
Specialized Procedures
- Endometrial biopsy
- Dilation and curettage
- Hysteroscopic evaluation
- Cervical cytology
- Endocrine evaluation
Age-Specific Diagnostic Considerations
Adolescents
Focus on bleeding disorders, pregnancy, and anovulation. Structural causes less common.
Reproductive Age
Rule out pregnancy, assess for structural and hormonal causes, consider malignancy risk factors.
Postmenopausal
High priority for endometrial sampling to rule out malignancy and precancerous conditions.
Treatment Management Approaches
Management of abnormal uterine bleeding follows a stepwise approach, beginning with conservative measures and progressing to more invasive interventions based on symptom severity, patient preferences, and treatment response. The goal is to restore normal bleeding patterns while preserving fertility when desired.
Medical Management
Hormonal Therapies
- • Combined oral contraceptives
- • Levonorgestrel intrauterine system
- • Progestin therapy (oral, injectable)
- • GnRH agonists (short-term use)
Non-Hormonal Options
- • Tranexamic acid (antifibrinolytic)
- • NSAIDs (mefenamic acid, ibuprofen)
- • Iron supplementation
- • Desmopressin (bleeding disorders)
Surgical Interventions
Minimally Invasive
- • Endometrial ablation
- • Hysteroscopic polypectomy
- • Myomectomy (hysteroscopic, laparoscopic)
- • Uterine artery embolization
Definitive Procedures
- • Total hysterectomy
- • Bilateral salpingo-oophorectomy
- • Radical procedures (malignancy)
| Treatment Approach | Indications | Effectiveness | Considerations |
|---|---|---|---|
| Levonorgestrel IUS | Heavy menstrual bleeding, contraception desired | 80-90% reduction in bleeding | Initial irregular bleeding, long-term contraception |
| Tranexamic Acid | Heavy bleeding, contraception not needed | 40-50% reduction in bleeding | Taken during menstruation only, well-tolerated |
| Endometrial Ablation | Completed childbearing, failed medical therapy | 85% satisfaction rate | Contraception required, pregnancy dangerous |
| Hysterectomy | Failed conservative treatment, patient preference | 100% effective for bleeding | Major surgery, loss of fertility, hormone considerations |
Evidence-Based Nursing Interventions
Nursing care for patients with abnormal uterine bleeding extends beyond medication administration to include comprehensive holistic care, patient advocacy, education, and psychosocial support. Effective nursing interventions can significantly improve patient outcomes and quality of life.
Acute Care Interventions
Hemodynamic Monitoring
Assess vital signs, orthostatic changes, signs of hypovolemia
IV Access & Fluid Management
Establish IV access, fluid resuscitation, blood product administration
Bleeding Assessment
Quantify blood loss, monitor pad counts, clot assessment
Ongoing Care Management
Medication Management
Administer treatments, monitor effectiveness, manage side effects
Symptom Monitoring
Track bleeding patterns, pain levels, functional status
Psychosocial Support
Address anxiety, body image concerns, relationship impacts
Nursing Care Plan Framework
Priority Diagnoses
- • Risk for deficient fluid volume
- • Acute pain related to uterine contractions
- • Anxiety related to bleeding
- • Deficient knowledge regarding condition
Expected Outcomes
- • Hemodynamic stability maintained
- • Pain controlled to acceptable levels
- • Anxiety reduced through education
- • Patient demonstrates self-care knowledge
Evaluation Criteria
- • Vital signs within normal limits
- • Bleeding controlled or decreased
- • Pain score <4/10
- • Patient verbalizes understanding
Documentation Essentials
Accurate documentation is crucial for tracking treatment effectiveness and ensuring continuity of care. Key elements include:
- • Detailed bleeding assessment (amount, character, timing)
- • Pain assessment using standardized scales
- • Vital signs and hemodynamic status
- • Response to interventions and medications
- • Patient education provided and understanding demonstrated
- • Psychosocial concerns and interventions
- • Communication with healthcare team
- • Discharge planning and follow-up arrangements
Patient Education & Self-Management
Comprehensive patient education is fundamental to successful management of abnormal uterine bleeding. Empowering patients with knowledge about their condition, treatment options, and self-care strategies improves adherence to treatment plans and enhances quality of life.
Understanding the Condition
What is Normal?
Help patients understand normal menstrual patterns and recognize deviations that require medical attention.
Causes & Risk Factors
Explain specific causes relevant to the patient’s diagnosis and modifiable risk factors.
Treatment Options
Discuss available treatments, expected outcomes, and potential side effects in understandable terms.
Self-Management Strategies
Bleeding Tracking
Teach methods for monitoring bleeding patterns, including menstrual calendars and mobile apps.
Lifestyle Modifications
Discuss stress management, nutrition, exercise, and weight management strategies.
Emergency Preparedness
Provide clear guidelines for when to seek immediate medical attention.
| Education Topic | Key Teaching Points | Teaching Methods |
|---|---|---|
| Medication Adherence | Importance of consistent timing, managing side effects, when to contact provider | Pill organizers, reminder apps, written instructions |
| Menstrual Hygiene | Product selection, changing frequency, infection prevention | Product samples, demonstrations, educational brochures |
| Sexual Health | Impact on intimacy, contraception needs, communication with partner | Private discussion, written resources, counseling referrals |
| Follow-up Care | Appointment importance, monitoring parameters, long-term management | Appointment scheduling, written follow-up plan, contact information |
Red Flag Symptoms
Educate patients to seek immediate medical attention for:
- • Soaking through a pad or tampon every hour for several hours
- • Bleeding for more than 7 days
- • Clots larger than a quarter
- • Severe cramping or pelvic pain
- • Signs of anemia (fatigue, shortness of breath, dizziness)
- • Fever or signs of infection
- • Bleeding after menopause
- • Fainting or severe weakness
Complications & Long-term Consequences
Untreated or inadequately managed abnormal uterine bleeding can lead to significant complications affecting multiple body systems and overall quality of life. Early recognition and intervention are essential to prevent these serious consequences.
Immediate Complications
Acute Blood Loss
Hypovolemic shock, requiring emergency transfusion and intensive monitoring
Severe Anemia
Iron deficiency anemia causing fatigue, weakness, and cardiac complications
Infection Risk
Increased susceptibility to infections due to compromised immune status
Long-term Consequences
Fertility Impact
Potential effects on reproductive capacity and pregnancy outcomes
Cardiovascular Effects
Chronic anemia leading to cardiac stress and potential heart failure
Psychological Impact
Depression, anxiety, and reduced quality of life due to chronic symptoms
| Complication | Risk Factors | Prevention Strategies | Management |
|---|---|---|---|
| Iron Deficiency Anemia | Heavy bleeding, poor diet, malabsorption | Early treatment, iron supplementation, dietary counseling | Iron therapy, treat underlying cause, monitor response |
| Social Dysfunction | Unpredictable bleeding, fear of embarrassment | Education, support groups, counseling | Symptom control, psychological support, workplace accommodations |
| Endometrial Hyperplasia | Unopposed estrogen, PCOS, obesity | Regular monitoring, progestin therapy, lifestyle modifications | Hormonal treatment, endometrial sampling, possible surgery |
| Missed Malignancy | Delayed diagnosis, inadequate workup | Age-appropriate screening, prompt evaluation | Immediate oncology referral, staging, treatment planning |
Quality of Life Impact
Abnormal uterine bleeding significantly affects multiple domains of life, requiring comprehensive assessment and intervention:
Physical Effects
- • Chronic fatigue and weakness
- • Sleep disturbances
- • Activity limitations
- • Pain and discomfort
Emotional Impact
- • Anxiety about bleeding episodes
- • Depression and mood changes
- • Body image concerns
- • Stress and worry about health
Social Consequences
- • Work absenteeism
- • Social isolation
- • Relationship strain
- • Economic burden
Key Points Summary
Essential Nursing Knowledge
- Abnormal uterine bleeding affects 14-25% of reproductive-age women
- PALM-COEIN classification guides systematic evaluation
- Early intervention prevents serious complications
- Multiple treatment options available from conservative to surgical
- Patient education is crucial for successful outcomes
Clinical Practice Applications
- Thorough assessment guides appropriate intervention
- Hemodynamic monitoring is priority in acute bleeding
- Psychosocial support addresses quality of life impact
- Documentation supports continuity of care
- Interdisciplinary collaboration optimizes outcomes
Future Nursing Practice
As healthcare continues to evolve, nurses play an increasingly vital role in managing abnormal uterine bleeding through evidence-based practice, patient advocacy, and comprehensive care coordination. Understanding the complex interplay of physiological, psychological, and social factors enables nurses to provide holistic care that addresses the full spectrum of patient needs. Continued education and clinical expertise in women’s health ensure optimal outcomes for patients experiencing this common yet complex condition.
