Endometriosis
Complete Nursing Guide for Students
Table of Contents
Introduction and Definition
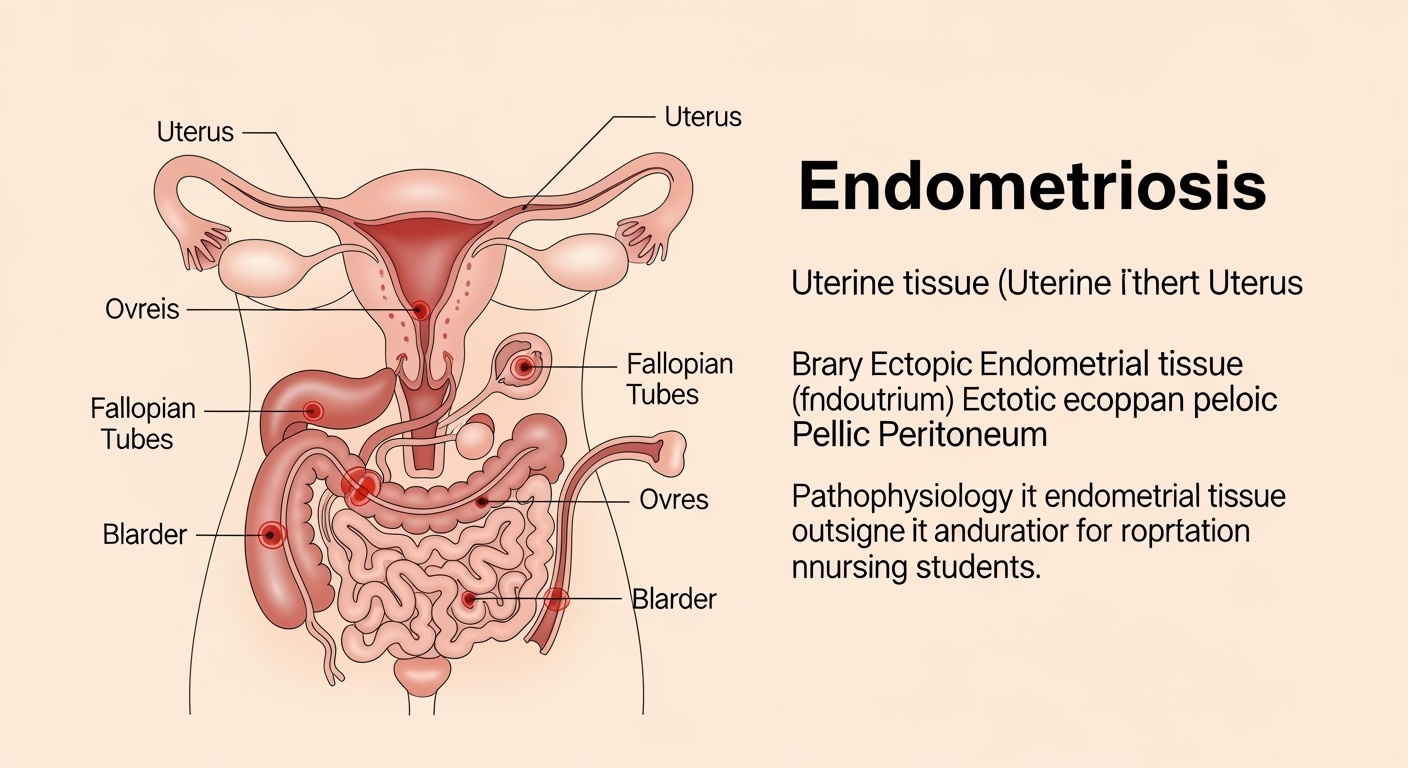
Endometriosis is a chronic gynecological condition characterized by the presence of endometrial tissue (the lining of the uterus) growing outside the uterine cavity. This ectopic endometrial tissue responds to hormonal changes throughout the menstrual cycle, causing inflammation, pain, and potentially leading to fertility issues. As a nursing professional, understanding endometriosis is crucial for providing comprehensive women’s health care.
Key Definition
Endometriosis affects approximately 10-15% of reproductive-age women globally, making it one of the most common gynecological conditions. The condition can significantly impact quality of life, fertility, and overall well-being, requiring specialized nursing care and patient education.
The condition was first described in medical literature in the 1860s, but comprehensive understanding has evolved significantly. Modern nursing practice emphasizes patient-centered care, pain management, and support for women living with endometriosis throughout their reproductive years and beyond.
Pathophysiology
The exact pathogenesis of endometriosis remains incompletely understood, but several theories explain how endometrial tissue develops outside the uterine cavity. Understanding these mechanisms helps nurses appreciate the complex nature of endometriosis and its varied presentations.
Retrograde Menstruation Theory
The most widely accepted theory suggests that menstrual blood flows backward through the fallopian tubes into the pelvic cavity, carrying viable endometrial cells that implant and grow on pelvic organs.
Immune System Dysfunction
Altered immune function may fail to clear ectopic endometrial tissue, allowing implantation and growth. This explains why some women develop endometriosis while others with retrograde menstruation do not.
Hormonal Influences
Endometriosis is an estrogen-dependent condition. Ectopic endometrial tissue responds to cyclical hormonal changes, particularly estrogen and progesterone, leading to:
- Proliferation during the follicular phase
- Secretory changes during the luteal phase
- Breakdown and bleeding during menstruation
- Inflammatory response and scar tissue formation
This cyclical process creates chronic inflammation, adhesion formation, and pain that characterizes endometriosis. The inflammatory environment also affects surrounding tissues and organs, contributing to the diverse symptoms associated with the condition.
Types and Classifications
Endometriosis classification systems help healthcare providers communicate about disease severity and guide treatment decisions. The American Society for Reproductive Medicine (ASRM) classification is most commonly used in clinical practice.
| Stage | Point Range | Description | Nursing Implications |
|---|---|---|---|
| Stage I (Minimal) | 1-5 points | Few superficial implants, minimal adhesions | Focus on pain management and patient education |
| Stage II (Mild) | 6-15 points | More implants, deeper lesions, mild adhesions | Monitor symptoms, support medication compliance |
| Stage III (Moderate) | 16-40 points | Multiple deep implants, moderate adhesions, ovarian endometriomas | Coordinate care, prepare for surgical interventions |
| Stage IV (Severe) | ≥40 points | Extensive implants, large endometriomas, dense adhesions | Complex care coordination, fertility counseling |
Anatomical Locations
Superficial Peritoneal
- • Pelvic peritoneum
- • Ovarian surface
- • Uterosacral ligaments
Ovarian Endometriomas
- • Chocolate cysts
- • Can be bilateral
- • Impact fertility
Deep Infiltrating
- • Rectovaginal septum
- • Bowel involvement
- • Bladder involvement
Signs and Symptoms
Endometriosis presents with diverse symptoms that can significantly impact quality of life. Many women experience years of symptoms before receiving an accurate diagnosis, highlighting the importance of thorough nursing assessment and patient advocacy.
Primary Symptoms
- Dysmenorrhea: Severe menstrual pain that worsens over time
- Chronic Pelvic Pain: Persistent pain lasting >6 months
- Dyspareunia: Pain during or after sexual intercourse
- Infertility: Difficulty conceiving after 12 months of trying
Associated Symptoms
- Heavy Menstrual Bleeding: Menorrhagia or metrorrhagia
- Bowel Symptoms: Diarrhea, constipation, painful defecation
- Urinary Symptoms: Dysuria, urgency, frequency
- Fatigue: Chronic exhaustion affecting daily activities
Nursing Assessment Pearl
Symptom severity doesn’t always correlate with disease stage. Women with minimal endometriosis may experience severe pain, while those with extensive disease may have minimal symptoms. Always validate the patient’s experience and avoid minimizing their concerns.
Cyclical Nature of Symptoms
Many endometriosis symptoms follow a cyclical pattern related to the menstrual cycle. Pain typically worsens during menstruation and may improve during the follicular phase. However, as the condition progresses, pain may become constant rather than cyclical.
Understanding the relationship between hormonal fluctuations and symptom patterns helps nurses provide targeted education and support for pain management strategies throughout the menstrual cycle.
Risk Factors
While the exact cause of endometriosis remains unknown, several risk factors have been identified that may increase a woman’s likelihood of developing the condition. Understanding these factors helps nurses provide appropriate screening and early intervention.
| Category | Risk Factors | Mechanism |
|---|---|---|
| Reproductive |
• Early menarche (<12 years) • Short cycles (<27 days) • Heavy flow (>7 days) • Nulliparity |
Increased estrogen exposure and retrograde menstruation |
| Genetic |
• Family history (mother/sister) • Genetic polymorphisms • Caucasian ethnicity |
Hereditary predisposition and immune dysfunction |
| Anatomical |
• Cervical stenosis • Uterine anomalies • Vaginal outflow obstruction |
Increased retrograde menstruation |
| Environmental |
• Low BMI (<20 kg/m²) • Alcohol consumption • Caffeine intake |
Hormonal influences and inflammatory processes |
Protective Factors
- • Multiple pregnancies and breastfeeding
- • Late menarche (>14 years)
- • Early menopause
- • Regular exercise and higher BMI
- • Omega-3 fatty acid consumption
Genetic Considerations
Women with a first-degree relative with endometriosis have a 7-10 times higher risk of developing the condition. Genetic counseling may be appropriate for families with multiple affected members.
Diagnostic Methods
Diagnosing endometriosis can be challenging, as symptoms often overlap with other gynecological conditions. A comprehensive approach combining clinical assessment, imaging studies, and sometimes surgical evaluation is necessary for accurate diagnosis.
Clinical Assessment
History Taking
- • Detailed menstrual history
- • Pain characteristics and timing
- • Sexual and reproductive history
- • Family history of endometriosis
- • Impact on quality of life
Physical Examination
- • Pelvic examination during menstruation
- • Uterosacral ligament nodularity
- • Fixed, retroverted uterus
- • Ovarian masses or tenderness
- • Rectovaginal examination
Imaging Studies
| Imaging Method | Sensitivity | Best Use | Limitations |
|---|---|---|---|
| Transvaginal Ultrasound | 90% for endometriomas | First-line imaging, ovarian assessment | Poor for superficial implants |
| MRI | 95% for endometriomas, 85% for DIE | Deep infiltrating disease, surgical planning | Expensive, time-consuming |
| CT Scan | Limited utility | Complications assessment | Radiation exposure, poor soft tissue contrast |
Laboratory Tests
Currently, no specific blood test can definitively diagnose endometriosis. However, certain biomarkers may support the diagnosis:
- CA-125: Elevated in 50% of cases, but non-specific
- CA 19-9: May be elevated in severe disease
- Anti-endometrial antibodies: Research stage, limited clinical use
- Inflammatory markers: CRP, IL-6 may be elevated
Gold Standard Diagnosis
Laparoscopy with histopathological confirmation remains the gold standard for endometriosis diagnosis. However, many clinicians now support empirical treatment based on clinical presentation to avoid unnecessary surgical procedures.
Nursing Assessment
Comprehensive nursing assessment forms the foundation of quality care for women with endometriosis. Nurses play a crucial role in gathering detailed information about symptoms, functional impact, and psychosocial effects of the condition.
Systematic Assessment Framework
Pain Assessment
- • Use validated pain scales (VAS, NRS)
- • Document pain patterns and triggers
- • Assess functional impact on daily activities
- • Evaluate current pain management strategies
- • Note relationship to menstrual cycle
Psychosocial Assessment
- • Screen for anxiety and depression
- • Assess impact on relationships
- • Evaluate coping mechanisms
- • Identify support systems
- • Assess work/school attendance
Comprehensive Assessment Areas
| Assessment Domain | Key Components | Tools/Methods |
|---|---|---|
| Physical Symptoms |
Pain intensity, location, quality Menstrual patterns GI and GU symptoms |
Pain diary, symptom tracking apps, standardized questionnaires |
| Functional Impact |
Activities of daily living Work/school performance Sexual function |
Functional assessment scales, quality of life measures |
| Reproductive Health |
Fertility desires Contraceptive needs Pregnancy history |
Reproductive health assessment, fertility counseling |
| Psychological Well-being |
Mental health status Stress levels Coping strategies |
Depression/anxiety screens, stress assessments |
Key Nursing Questions
- “How has endometriosis affected your daily life?” – Assesses functional impact
- “What strategies have you tried for pain management?” – Evaluates current coping methods
- “How is your relationship with your partner affected?” – Identifies relationship impacts
- “What are your concerns about future fertility?” – Addresses reproductive goals
Documentation and Communication
Accurate documentation of assessment findings facilitates communication among healthcare team members and supports continuity of care. Use objective language, include patient’s own words when describing pain and symptoms, and document the impact on quality of life metrics to support treatment decisions and insurance approvals.
Treatment Options
Endometriosis treatment requires an individualized approach based on symptom severity, fertility desires, age, and patient preferences. Treatment strategies focus on pain management, fertility preservation, and improving quality of life through medical and surgical interventions.
Medical Management
| Category | Medications | Mechanism | Nursing Considerations |
|---|---|---|---|
| NSAIDs |
Ibuprofen, naproxen Celecoxib (COX-2 selective) |
Anti-inflammatory, analgesic | Monitor GI symptoms, renal function, take with food |
| Hormonal Contraceptives |
Combined OCs Progestin-only pills Levonorgestrel IUD |
Suppresses ovulation, reduces estrogen | Assess contraindications, monitor breakthrough bleeding |
| GnRH Agonists |
Leuprolide, goserelin Nafarelin |
Creates pseudomenopause | Monitor bone density, vasomotor symptoms, mood changes |
| GnRH Antagonists |
Elagolix Relugolix combination |
Blocks GnRH receptors | Newer agents with add-back therapy to minimize side effects |
Surgical Management
Conservative Surgery
- • Laparoscopic excision of implants
- • Ovarian cystectomy for endometriomas
- • Lysis of adhesions
- • Preserves reproductive organs
- • Suitable for fertility preservation
Definitive Surgery
- • Total hysterectomy
- • Bilateral salpingo-oophorectomy
- • Reserved for severe cases
- • When fertility not desired
- • May require hormone replacement
Complementary and Alternative Therapies
Evidence-Based Complementary Approaches
- • Pelvic floor physical therapy
- • Acupuncture
- • Yoga and stretching
- • Heat therapy
- • Anti-inflammatory diet
- • Regular exercise
- • Stress management
- • Omega-3 supplementation
Treatment Selection Considerations
Treatment decisions should be individualized based on patient age, symptom severity, fertility desires, previous treatments, and quality of life impact. A multidisciplinary approach involving gynecologists, pain specialists, mental health professionals, and nurses provides comprehensive care that addresses all aspects of endometriosis management.
Nursing Interventions
Nursing interventions for endometriosis focus on holistic care addressing physical symptoms, psychological well-being, and quality of life. Nurses serve as patient advocates, educators, and coordinators of care throughout the treatment journey.
Priority Nursing Diagnoses
| Nursing Diagnosis | Related Factors | Expected Outcomes |
|---|---|---|
| Chronic Pain | Endometrial implants, inflammation, adhesions | Patient reports pain level ≤4/10, demonstrates effective coping strategies |
| Activity Intolerance | Pain, fatigue, decreased energy | Patient participates in daily activities with minimal limitations |
| Anxiety | Uncertain prognosis, fertility concerns, chronic pain | Patient demonstrates reduced anxiety levels, uses effective coping mechanisms |
| Sexual Dysfunction | Dyspareunia, fear of pain, relationship strain | Patient reports improved sexual satisfaction and intimacy |
Specific Nursing Interventions
Pain Management
- • Administer medications as prescribed
- • Teach non-pharmacological pain relief methods
- • Position for comfort and relaxation
- • Apply heat therapy as appropriate
- • Monitor pain levels and document patterns
- • Coordinate with pain management specialists
Psychosocial Support
- • Provide emotional support and active listening
- • Validate patient’s experiences and concerns
- • Facilitate support group connections
- • Screen for depression and anxiety
- • Refer to mental health professionals as needed
- • Encourage stress management techniques
Collaborative Care Interventions
Multidisciplinary Team Coordination
Nurses play a central role in coordinating care among various specialists involved in endometriosis management:
Pre and Post-operative Care
Pre-operative Interventions
- • Complete comprehensive assessment
- • Provide surgical education and counseling
- • Address anxiety and concerns
- • Ensure informed consent understanding
- • Coordinate pre-operative testing
Post-operative Interventions
- • Monitor for complications and infection
- • Manage post-operative pain effectively
- • Provide incision care education
- • Support early mobilization
- • Plan discharge and follow-up care
Effective nursing interventions for endometriosis require ongoing assessment, individualized care planning, and regular evaluation of outcomes. Nurses must maintain current knowledge about treatment advances and provide compassionate, evidence-based care that supports women throughout their endometriosis journey.
Patient Education
Comprehensive patient education empowers women with endometriosis to actively participate in their care, manage symptoms effectively, and make informed decisions about treatment options. Education should be tailored to individual learning needs and cultural preferences.
Core Educational Components
Disease Understanding
- • Basic anatomy and physiology
- • Pathophysiology of endometriosis
- • Natural history and progression
- • Genetic and environmental factors
- • Myth dispelling and fact clarification
Treatment Education
- • Medication actions and side effects
- • Proper administration techniques
- • Importance of adherence
- • When to contact healthcare providers
- • Alternative therapy options
Self-Management Strategies
| Strategy Category | Specific Interventions | Teaching Points |
|---|---|---|
| Pain Management |
Heat therapy, relaxation techniques Exercise, stress reduction Medication timing |
Start treatments early in pain cycle, track effectiveness, combine approaches |
| Lifestyle Modifications |
Anti-inflammatory diet Regular exercise routine Sleep hygiene |
Gradual implementation, realistic goal setting, track improvements |
| Fertility Planning |
Timing considerations Preconception counseling Assisted reproduction options |
Early consultation with fertility specialists, preserve options, realistic expectations |
| Emotional Well-being |
Support groups Mental health resources Communication strategies |
Normalize emotional responses, encourage professional help, build support networks |
Medication Education Priorities
Critical Teaching Points for Common Medications
- • Take at same time daily for effectiveness
- • Report breakthrough bleeding patterns
- • Monitor mood changes and depression
- • Understand contraindications and risks
- • Expect temporary symptom worsening initially
- • Manage menopausal-like side effects
- • Importance of bone health monitoring
- • Duration limitations and follow-up needs
Communication and Advocacy
Healthcare Communication
- • Keep detailed symptom diaries
- • Prepare questions before appointments
- • Communicate treatment goals clearly
- • Advocate for appropriate referrals
- • Understand when to seek urgent care
Workplace/School Considerations
- • Know rights regarding medical accommodations
- • Communicate needs appropriately
- • Plan for symptom management during work/school
- • Access to workplace/school health resources
- • Manage attendance and productivity concerns
Educational Resources and Support
Provide patients with reliable, evidence-based resources including reputable websites, patient education materials, support group information, and mobile applications for symptom tracking. Encourage patients to become informed advocates for their health while maintaining realistic expectations about treatment outcomes and disease management.
Complications
Endometriosis can lead to various complications that significantly impact a woman’s health and quality of life. Understanding these potential complications helps nurses provide comprehensive care and educate patients about warning signs and when to seek medical attention.
Reproductive Complications
Fertility Issues
- • Affects 30-50% of women with endometriosis
- • Distorted pelvic anatomy from adhesions
- • Impaired ovarian function
- • Altered inflammatory environment
- • Decreased egg quality and quantity
- • May require assisted reproductive technology
Pregnancy Complications
- • Increased risk of ectopic pregnancy
- • Higher rates of miscarriage
- • Preterm birth complications
- • Placental abnormalities
- • Increased cesarean delivery rates
- • Requires specialized obstetric care
Anatomical and Functional Complications
| Complication | Mechanism | Clinical Presentation | Nursing Management |
|---|---|---|---|
| Adhesion Formation | Chronic inflammation, repeated bleeding | Pelvic pain, bowel obstruction, infertility | Pain assessment, patient education, surgical preparation |
| Ovarian Endometriomas | Cystic collections of endometrial tissue | Pelvic mass, pain, ovarian dysfunction | Monitor size changes, fertility counseling |
| Bowel Involvement | Deep infiltrating endometriosis | Cyclic rectal bleeding, obstruction | Coordinate with gastroenterology, dietary counseling |
| Bladder Involvement | Endometrial implants on bladder | Cyclic hematuria, urinary symptoms | Monitor urinary function, coordinate with urology |
Psychological and Social Complications
Mental Health Impact
Women with endometriosis experience significantly higher rates of depression, anxiety, and decreased quality of life compared to the general population. The chronic pain, fertility concerns, and impact on relationships contribute to psychological distress.
- • Depression and anxiety disorders
- • Chronic pain syndrome
- • Grief and loss related to fertility
- • Body image concerns
- • Relationship strain and sexual dysfunction
- • Work/school absenteeism
- • Social isolation and activity limitation
- • Financial burden of treatment
Rare but Serious Complications
Malignant Transformation
- • Risk of ovarian cancer (especially clear cell and endometrioid types)
- • Occurs in <1% of cases
- • Higher risk with endometriomas >9cm
- • Regular surveillance recommended
Emergency Complications
- • Ovarian torsion from large endometriomas
- • Bowel obstruction from adhesions
- • Spontaneous pneumothorax (thoracic endometriosis)
- • Massive hemorrhage from ruptured endometriomas
Prevention and Early Detection
While many complications cannot be prevented, early recognition and treatment of endometriosis can minimize progression and impact. Nurses play crucial roles in patient education about warning signs, promoting adherence to treatment plans, and facilitating regular follow-up care to monitor for potential complications and intervene early when problems arise.
Prognosis and Follow-up
The prognosis for women with endometriosis varies significantly based on disease severity, age at diagnosis, treatment response, and individual factors. Understanding long-term outcomes helps nurses provide realistic expectations and support informed decision-making about treatment options.
Long-term Outcomes
| Outcome Measure | Conservative Treatment | Surgical Treatment | Factors Affecting Outcome |
|---|---|---|---|
| Pain Relief | 60-80% experience improvement with hormonal therapy | 80-90% experience pain reduction post-surgery | Disease stage, patient age, treatment adherence |
| Fertility | Natural conception rates vary by severity | Improved conception rates post-conservative surgery | Age, ovarian reserve, disease location |
| Disease Recurrence | Symptoms return when treatment discontinued | 10-20% recurrence rate within 5 years | Completeness of excision, hormonal suppression |
| Quality of Life | Significant improvement with effective treatment | Substantial improvement in most patients | Psychological support, treatment compliance |
Factors Influencing Prognosis
Positive Prognostic Factors
- • Early diagnosis and treatment initiation
- • Minimal to mild disease stage
- • Young age at diagnosis
- • Good response to initial treatment
- • Strong support system and coping skills
- • Adherence to treatment recommendations
Challenging Prognostic Factors
- • Advanced disease stage at diagnosis
- • Deep infiltrating endometriosis
- • Multiple previous surgeries
- • Severe adhesive disease
- • Comorbid conditions (adenomyosis, fibroids)
- • Poor treatment tolerance or response
Follow-up Care Planning
Structured Follow-up Schedule
- • Monthly visits for symptom assessment
- • Monitor treatment tolerance
- • Adjust medications as needed
- • Address side effects promptly
- • Quarterly visits for monitoring
- • Annual pelvic examinations
- • Imaging as clinically indicated
- • Fertility counseling if appropriate
- • Biannual or annual visits
- • Cancer screening as appropriate
- • Bone density monitoring (if on GnRH therapy)
- • Menopause transition planning
Menopause and Endometriosis
Natural menopause typically leads to improvement in endometriosis symptoms due to decreased estrogen production. However, hormone replacement therapy (HRT) decisions require careful consideration of benefits and risks. Post-menopausal women with a history of endometriosis should be monitored for rare malignant transformation.
Menopause Management
- • Symptoms typically improve with menopause
- • HRT decisions require individualization
- • Consider progestin-containing HRT
- • Monitor for symptom recurrence
Long-term Monitoring
- • Annual gynecological examinations
- • Appropriate cancer screening
- • Cardiovascular and bone health assessment
- • Mental health support as needed
Patient Empowerment and Self-Advocacy
Successful long-term management of endometriosis requires active patient participation in care decisions and ongoing self-monitoring. Nurses should encourage patients to maintain symptom diaries, communicate openly about treatment concerns, and advocate for appropriate specialist referrals when needed. Regular follow-up care, combined with patient education and support, optimizes outcomes and quality of life for women living with endometriosis.
