Pelvic Organ Prolapse: Complete Nursing Guide
Comprehensive Study Notes on Cystocele, Urethrocele, and Rectocele
Understanding Pelvic Organ Prolapse
Pelvic organ prolapse represents a significant healthcare concern affecting millions of women worldwide. This condition occurs when the pelvic floor muscles and connective tissues become weakened or damaged, resulting in the descent of pelvic organs into or beyond the vaginal canal.
Key Statistics
- Affects up to 20% of women over age 20
- Prevalence increases to 40% in women over 50
- Risk factors include childbirth, aging, and genetic predisposition
- Significantly impacts quality of life and daily activities
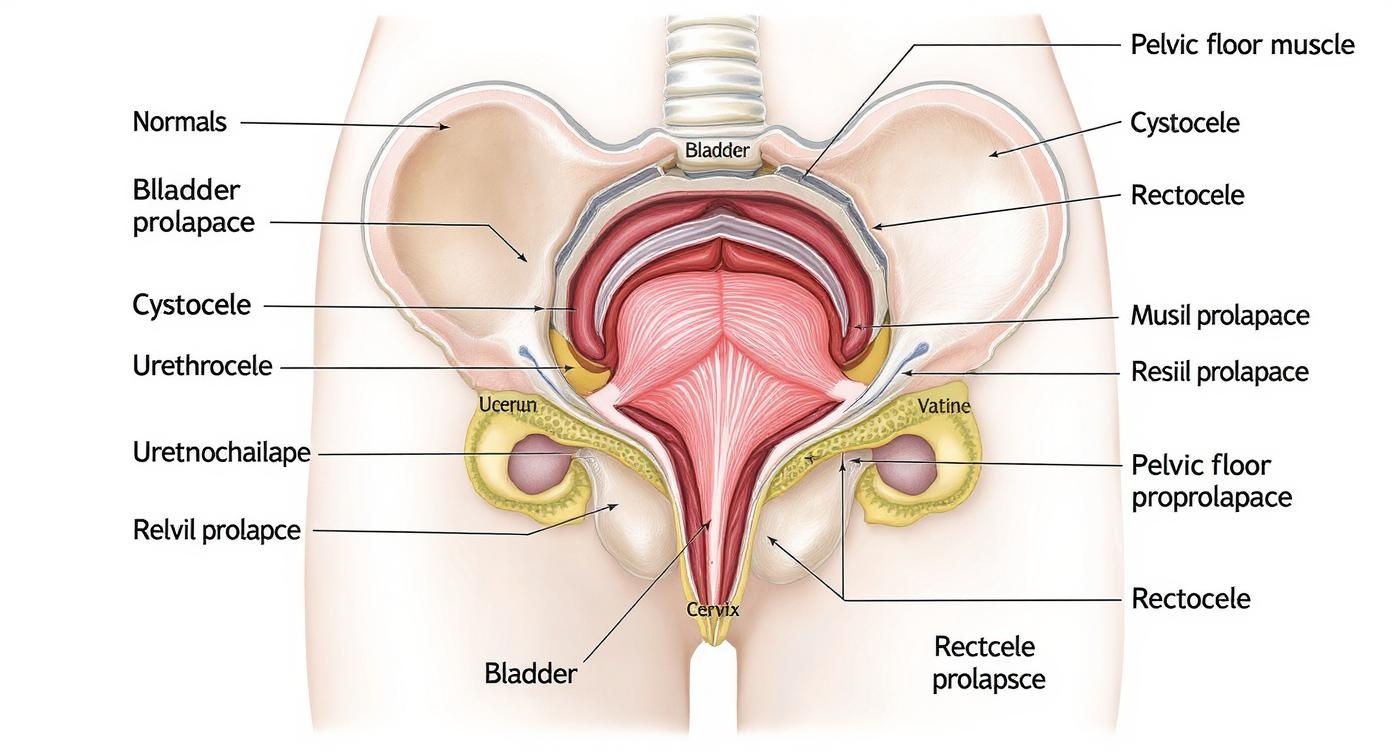
Anatomical comparison showing normal pelvic anatomy and various types of prolapse conditions
Clinical Pearl
Early recognition and intervention for pelvic organ prolapse can significantly improve patient outcomes and prevent progression to more severe stages requiring surgical intervention.
Anatomy and Pathophysiology
Normal Pelvic Floor Support
The pelvic floor consists of three levels of support that work together to maintain organ position and function. Understanding this normal anatomy is crucial for recognizing how prolapse develops and progresses.
Level I Support (Suspension)
Cardinal and uterosacral ligaments provide apical support
Level II Support (Attachment)
Endopelvic fascia attaches vagina to pelvic sidewalls
Level III Support (Fusion)
Perineal body and levator ani muscles provide floor support
Pathophysiology of Prolapse
Pelvic organ prolapse occurs when any of these support mechanisms become compromised, leading to organ descent and dysfunction.
Prolapse Grading System (POP-Q)
| Stage | Description | Clinical Significance |
|---|---|---|
| Stage 0 | No prolapse | Normal anatomy |
| Stage I | >1 cm above hymen | Minimal descent |
| Stage II | ≤1 cm of hymen | Moderate prolapse |
| Stage III | >1 cm beyond hymen | Severe prolapse |
| Stage IV | Complete prolapse | Total organ eversion |
Cystocele (Bladder Prolapse)
Definition and Mechanism
A cystocele, also known as anterior vaginal wall prolapse, occurs when the bladder herniates into the vaginal space due to weakening of the pubocervical fascia. This type of prolapse represents the most common form of pelvic organ prolapse, affecting the anterior compartment of the pelvis.
Pathophysiology
The pubocervical fascia, which normally supports the bladder, becomes stretched or torn during childbirth or chronic straining. This creates a weakness that allows the bladder to descend and bulge into the anterior vaginal wall.
Risk Factors
Modifiable Factors
- Chronic constipation and straining
- Obesity (BMI >30)
- Heavy lifting occupations
- Chronic cough
- Smoking
Non-modifiable Factors
- Advancing age
- Vaginal childbirth
- Genetic predisposition
- Connective tissue disorders
- Menopausal status
Memory Aid: BLADDER
- Bulge in anterior wall
- Loss of urine control
- Aging and childbirth risks
- Difficulty emptying bladder
- Discomfort and pressure
- Estrogen deficiency impact
- Recurrent infections
Clinical Note
Cystocele often occurs with stress urinary incontinence, but some patients may experience urinary retention due to bladder kinking.
Signs and Symptoms
Urinary Symptoms
Physical Symptoms
Urethrocele (Urethral Prolapse)
Pathophysiology and Presentation
Urethrocele involves the downward displacement of the urethra, often occurring in conjunction with cystocele. This condition results from weakness in the urethrovesical support structures, leading to loss of normal urethral anatomy and function. The prolapse typically affects the distal urethra and can significantly impact urinary continence mechanisms.
Diagnostic Characteristics
- Loss of normal urethral support and hypermobility
- Urethral descent >30 degrees from horizontal
- Associated with stress incontinence in 80% of cases
- May present with recurrent urinary tract infections
- Often accompanied by anterior vaginal wall prolapse
Unique Features
Unlike isolated cystocele, urethrocele specifically involves urethral hypermobility and loss of the normal urethrovesical angle, making stress incontinence a predominant symptom.
Memory Aid: URETHRA
- Urethral hypermobility
- Recurrent infections
- Evacuation difficulties
- Time to void increased
- Hypermobility on exam
- Reduced continence
- Angle loss (urethrovesical)
Clinical Assessment Tools
Management Considerations
| Severity | Conservative Management | Surgical Options | Expected Outcomes |
|---|---|---|---|
| Mild | Pelvic floor exercises, lifestyle modification | Usually not indicated | Good response to conservative care |
| Moderate | Pessary, bladder training, weight management | Consideration for sling procedures | Variable success with conservative measures |
| Severe | Pessary for non-surgical candidates | Urethropexy, sling procedures | High success rate with surgical intervention |
Rectocele (Rectal Prolapse)
Understanding Posterior Wall Prolapse
Rectocele represents a posterior vaginal wall prolapse where the rectum herniates into the vaginal space due to weakness or separation of the rectovaginal fascia. This condition significantly impacts bowel function and quality of life, often requiring multidisciplinary management involving nursing, gynecology, and colorectal specialists.
Anatomical Defect
The rectovaginal septum, which normally separates the rectum from the vagina, becomes weakened or disrupted. This allows the rectal wall to bulge into the posterior vaginal space, creating a pocket that can trap stool and interfere with normal defecation.
Classification by Location
- Low Rectocele: Near the perineal body
- Mid Rectocele: At the mid-vaginal level
- High Rectocele: Near the vaginal apex
Memory Aid: RECTUM
- Rectal pressure and bulging
- Evacuation difficulties
- Constipation and straining
- Trapping of stool in pocket
- Unique splinting maneuvers
- Manual assistance for defecation
Clinical Insight
Many patients with rectocele develop compensatory behaviors like digital splinting or changing body position during defecation to facilitate bowel movements.
Symptoms and Impact on Daily Life
Bowel Symptoms
Physical Discomfort
Functional Impact
Comprehensive Nursing Assessment
History Taking and Interview
A thorough nursing assessment for pelvic organ prolapse requires sensitive communication and systematic evaluation. The assessment should be conducted in a private, comfortable environment where patients feel safe to discuss intimate symptoms and concerns.
Essential Assessment Areas
Nursing Communication Tips
- Use open-ended questions to encourage discussion
- Validate patient concerns and normalize symptoms
- Maintain professional yet compassionate demeanor
- Respect cultural and personal boundaries
Physical Assessment Components
Visual Inspection
- Patient in lithotomy position
- Observe at rest and with Valsalva maneuver
- Assess vaginal opening and perineum
- Document presence and extent of any bulge
Palpation Assessment
- Single-finger examination initially
- Assess anterior, posterior, and apical walls
- Evaluate prolapse with patient straining
- Check for associated organ involvement
Functional Testing
- Cough stress test for incontinence
- Post-void residual measurement
- Pelvic floor muscle strength assessment
- Rectal examination if rectocele suspected
Assessment Tools and Questionnaires
| Assessment Tool | Purpose | Key Features |
|---|---|---|
| PFDI-20 | Pelvic floor distress | 20 questions, symptom severity |
| PFIQ-7 | Quality of life impact | Life impact assessment |
| PISQ-12 | Sexual function | Relationship and intimacy |
Assessment Mnemonic: PROLAPSE
- Pressure sensations
- Rectal/bladder symptoms
- Organ visibility
- Lifestyle impact
- Activity limitations
- Pain or discomfort
- Sexual function changes
- Emotional well-being
Evidence-Based Nursing Interventions
Conservative Management Approaches
Nursing interventions for pelvic organ prolapse focus on conservative management strategies that can significantly improve symptoms and quality of life. These evidence-based approaches often serve as first-line treatments, particularly for mild to moderate prolapse conditions.
Pelvic Floor Muscle Training (PFMT)
- Protocol: 3 sets of 10 contractions, 3 times daily
- Technique: 10-second hold, 10-second rest cycles
- Progression: Gradual increase in hold time and repetitions
- Evidence: 70% improvement in mild to moderate prolapse
Lifestyle Modifications
- Weight management (target BMI <25)
- Constipation prevention strategies
- Proper lifting techniques education
- Smoking cessation support
Pessary Management
- Proper fitting and placement techniques
- Regular cleaning and maintenance schedules
- Signs of complications monitoring
- Patient education on self-care
Patient Education Strategies
Education Focus: EMPOWER
- Explain condition and treatment options
- Motivate lifestyle changes
- Provide practical skill training
- Offer ongoing support resources
- Work collaboratively on goals
- Evaluate progress regularly
- Reinforce positive behaviors
Teaching Methods
- Visual aids and anatomical models
- Demonstration and return demonstration
- Written instructions and resources
- Digital health apps for tracking
Behavioral Strategies
- Goal setting and action planning
- Self-monitoring techniques
- Problem-solving skill development
- Stress management and coping
Nursing Care Plans by Condition
Cystocele Care Plan
Urethrocele Care Plan
Rectocele Care Plan
Comprehensive Management Strategies
Multidisciplinary Approach
Effective management of pelvic organ prolapse requires a coordinated multidisciplinary approach. Nurses play a central role in coordinating care, providing education, and supporting patients through their treatment journey. The management strategy should be individualized based on symptom severity, patient preferences, and overall health status.
Healthcare Team Members
- Nurses: Assessment, education, conservative management
- Physicians: Medical evaluation and surgical consultation
- Physical Therapists: Specialized pelvic floor therapy
- Dietitians: Weight management and nutrition counseling
- Mental Health: Coping strategies and quality of life support
Evidence-Based Practice
Conservative management should be the first-line approach for most patients, with surgery reserved for those who fail conservative measures or have severe symptoms significantly impacting quality of life.
Treatment Decision Algorithm
Mild Symptoms (Stage I-II)
- Conservative management trial (6-12 weeks)
- Lifestyle modifications and PFMT
- Pessary consideration if exercises insufficient
- Regular monitoring and reassessment
Moderate Symptoms (Stage II-III)
- Intensive conservative management
- Pessary fitting and trial
- Specialized physical therapy referral
- Surgical consultation if conservative fails
Severe Symptoms (Stage III-IV)
- Surgical evaluation and consultation
- Pessary as bridge or alternative
- Comprehensive preoperative assessment
- Patient preference and shared decision-making
Monitoring and Follow-up Protocol
| Timeframe | Assessment Focus | Key Interventions | Expected Outcomes |
|---|---|---|---|
| Week 1-2 | Initial response to treatment | Technique refinement, motivation | Improved understanding and compliance |
| Week 6 | Symptom improvement assessment | Treatment adjustment, encouragement | Measurable symptom reduction |
| Week 12 | Treatment efficacy evaluation | Plan modification or escalation | Significant functional improvement |
| 6 Months | Long-term maintenance | Lifestyle integration, support | Sustained improvement and satisfaction |
Quality of Life Enhancement
Psychosocial Support
- Normalize symptoms and validate concerns
- Provide realistic expectations for improvement
- Connect with support groups and resources
- Address relationship and intimacy concerns
- Screen for depression and anxiety
QOL Improvement: BETTER
- Behavioral modifications
- Education and understanding
- Treatment adherence support
- Time for gradual improvement
- Emotional support and counseling
- Regular monitoring and adjustment
Global Best Practices and Innovations
International Standards and Guidelines
Healthcare systems worldwide have developed innovative approaches to managing pelvic organ prolapse, with evidence-based practices showing remarkable success in improving patient outcomes and reducing healthcare costs.
Nordic Countries Model
Comprehensive population-based screening and early intervention programs
- Standardized assessment protocols in primary care
- Nurse-led conservative management programs
- 95% success rate in preventing surgical intervention
Australian Initiative
National continence program with specialized nurse practitioners
- Community-based education and support
- Telehealth consultations for rural areas
- Significant improvement in patient satisfaction scores
Canadian Best Practice
Integrated care pathways with multidisciplinary teams
- Standardized outcome measurements
- Patient-centered care planning
- Reduced wait times and improved access
Innovative Technologies and Approaches
Digital Health Solutions
- Mobile apps for pelvic floor exercise tracking
- Biofeedback devices for real-time muscle training
- Telemedicine platforms for remote monitoring
- Virtual reality for patient education
Research Innovations
- 3D printed customized pessaries
- Advanced imaging for assessment
- Biomarker development for early detection
- Minimally invasive surgical techniques
Future Directions
- Personalized medicine approaches
- Regenerative therapy research
- Artificial intelligence in diagnosis
- Prevention-focused healthcare models
Key Takeaways for Nursing Practice
Essential Clinical Competencies
- Comprehensive assessment skills for pelvic organ prolapse conditions
- Evidence-based conservative management strategies implementation
- Patient education and empowerment techniques
- Multidisciplinary care coordination and advocacy
Professional Development
Understanding pelvic organ prolapse enhances nursing practice across multiple specialties. These conditions affect millions of women and require compassionate, knowledgeable care that addresses both physical symptoms and quality of life impacts.
“Excellence in nursing care for prolapse patients comes from combining clinical expertise with genuine empathy and patient-centered approaches to improve outcomes and restore confidence.”
