HPV Vaccination: Comprehensive Nursing Study Guide
Evidence-Based Immunization Protocols for Professional Practice
Table of Contents
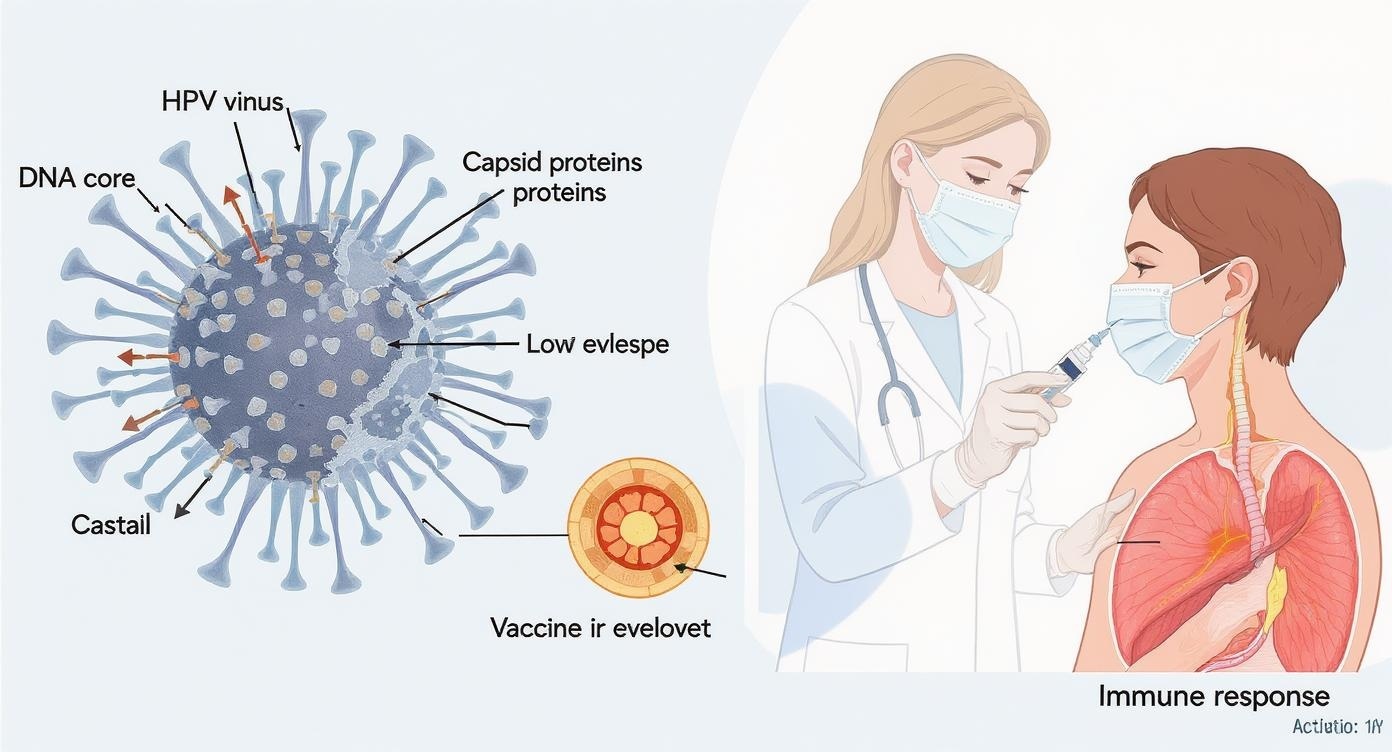
Educational illustration demonstrating HPV virus structure and vaccination immunization process
Introduction to Human Papillomavirus (HPV)
Human Papillomavirus (HPV) represents one of the most common sexually transmitted infections worldwide, affecting millions of individuals annually. As nursing professionals, understanding HPV immunization protocols is crucial for providing comprehensive patient care and promoting public health initiatives.
HPV encompasses over 200 related viruses, with approximately 40 types affecting the genital areas, mouth, and throat. The significance of HPV vaccination extends beyond individual protection, contributing to herd immunity and reducing healthcare burden globally.
Key Learning Objectives
- Understand HPV pathophysiology and transmission patterns
- Master evidence-based immunization administration techniques
- Develop effective patient education strategies
- Recognize contraindications and manage adverse reactions
HPV Impact Statistics
| Category | Statistics | Clinical Significance |
|---|---|---|
| Global Infections | 290 million women infected | High transmission rates necessitate preventive immunization |
| Cervical Cancer | 570,000 new cases annually | 99% caused by HPV, preventable through vaccination |
| Vaccine Efficacy | 90% reduction in targeted HPV types | Demonstrates strong evidence for immunization programs |
HPV Pathophysiology and Disease Progression
Viral Structure
- • Double-stranded DNA virus
- • Non-enveloped capsid structure
- • 55 nanometer diameter
- • L1 and L2 capsid proteins
Transmission Routes
- • Sexual contact (primary)
- • Skin-to-skin contact
- • Vertical transmission (rare)
- • Fomite transmission (minimal)
Disease Timeline
- • Incubation: 2-3 months
- • Peak infectivity: 6 months
- • Persistence: 12-24 months
- • Cancer development: 10-20 years
HPV Classification and Associated Conditions
High-Risk HPV Types
Types: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68
Associated Cancers:
- Cervical cancer (99% of cases)
- Anal cancer (90% of cases)
- Oropharyngeal cancer (70% of cases)
- Vaginal and vulvar cancers
- Penile cancer
Low-Risk HPV Types
Types: 6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81
Associated Conditions:
- Genital warts (90% caused by types 6 and 11)
- Recurrent respiratory papillomatosis
- Benign cervical lesions
- Low-grade cervical dysplasia
Memory Aid: HPV Types Classification
Remember: HPV types 16 and 18 are the most common high-risk types causing cervical cancer. They’re responsible for approximately 70% of all cervical cancer cases worldwide.
HPV Vaccine Types and Mechanisms of Action
Current HPV Vaccine Formulations
| Vaccine | HPV Types Covered | Manufacturer | Current Status |
|---|---|---|---|
| Gardasil 9 (9vHPV) | 6, 11, 16, 18, 31, 33, 45, 52, 58 | Merck & Co. | Primary Use |
| Gardasil (4vHPV) | 6, 11, 16, 18 | Merck & Co. | Phased Out |
| Cervarix (2vHPV) | 16, 18 | GlaxoSmithKline | Discontinued US |
Mechanism of Immunization
Virus-Like Particles (VLPs)
Recombinant L1 capsid proteins self-assemble into VLPs that mimic viral structure without containing genetic material
Antigen Presentation
Dendritic cells process VLPs and present antigens to naive T cells, initiating adaptive immune response
Antibody Production
B cells differentiate into plasma cells producing type-specific neutralizing antibodies
Memory Formation
Memory B and T cells provide long-lasting protection against future HPV exposure
Immunization Efficacy
Prevention of Targeted HPV Types:
• 95-100% efficacy in naive populations
• Sustained protection for 10+ years
Cancer Prevention:
• 90% reduction in cervical cancer incidence
• 70% reduction in high-grade lesions
Cross-Protection:
• Limited protection against related HPV types
• Variable efficacy (30-50%)
Vaccine Formulation Details
Active Ingredients
- • L1 capsid proteins (VLPs)
- • Type-specific antigens
- • Recombinant technology
Adjuvants
- • Aluminum hydroxyphosphate sulfate
- • Enhanced immune response
- • Improved antigen presentation
Excipients
- • Sodium chloride
- • L-histidine
- • Polysorbate 80
HPV Vaccine Administration Protocols
Ages 9-14 Years (2-Dose Schedule)
Optimal immunization window for enhanced immune response
Ages 15-26 Years (3-Dose Schedule)
Complete series for optimal immunization protection
Proper Administration Technique
Pre-Administration Assessment
- Verify patient identity and vaccination history
- Review contraindications and precautions
- Assess current health status and medications
- Obtain informed consent and address concerns
- Check vaccine storage temperature and expiration
Injection Technique
- Site: Deltoid muscle (preferred)
- Needle: 22-25 gauge, 1-1.5 inch
- Volume: 0.5 mL intramuscular
- Angle: 90-degree insertion
- Alternative: Anterolateral thigh (ages 9-18)
Critical Storage Requirements
Temperature Control
- • Store at 2-8°C (36-46°F)
- • Never freeze
- • Protect from light
- • Monitor continuously
Cold Chain Management
- • Use within 8 hours at room temperature
- • Transport in approved containers
- • Document temperature logs
- • Report excursions immediately
Quality Control
- • Check expiration dates
- • Inspect for particles/discoloration
- • Rotate stock (FIFO method)
- • Maintain inventory records
Memory Aid: VACCINE Administration Steps
- V – Verify patient identity and history
- A – Assess contraindications and health status
- C – Check vaccine storage and expiration
- C – Consent obtained and documented
- I – Inject using proper technique
- N – Note injection site and observe patient
- E – Educate patient about next steps and side effects
Patient and Family Education Strategies
Educational Priorities
HPV Disease Understanding
Explain transmission, cancer risks, and prevalence using age-appropriate language
Vaccine Benefits
Emphasize cancer prevention, immunization efficacy, and long-term protection
Safety Profile
Discuss common side effects, safety monitoring, and risk-benefit ratio
Schedule Adherence
Stress importance of completing the immunization series for optimal protection
Target Audience Considerations
Adolescents (9-17 years)
- • Use simple, non-judgmental language
- • Address vaccine myths and peer concerns
- • Emphasize cancer prevention benefits
- • Respect developmental considerations
Young Adults (18-26 years)
- • Discuss sexual health comprehensively
- • Address catch-up immunization benefits
- • Provide evidence-based information
- • Support autonomous decision-making
Parents/Guardians
- • Address safety concerns and misconceptions
- • Provide comprehensive benefit information
- • Respect cultural and religious considerations
- • Encourage shared decision-making
Frequently Asked Questions and Evidence-Based Responses
“Is the HPV vaccine safe for my child?”
Evidence-based response: HPV vaccines have an excellent safety profile with over 270 million doses administered globally. The most common side effects are mild local reactions. Extensive safety monitoring through VAERS and VSD systems demonstrates no serious safety concerns. The immunization benefits far outweigh minimal risks.
“Why does my child need the vaccine if they’re not sexually active?”
Evidence-based response: HPV immunization is most effective when administered before exposure to the virus. The immune response is stronger in younger individuals, and the vaccine provides optimal protection before potential exposure. This represents preventive care similar to other childhood immunizations.
“Can the vaccine cause cancer or fertility problems?”
Evidence-based response: No scientific evidence supports these claims. HPV vaccines contain no live virus and cannot cause cancer. Large-scale studies involving millions of women show no impact on fertility. The vaccine prevents cancer – it does not cause it. These myths have been thoroughly debunked by extensive research.
“My child already had one dose years ago. Do they need to restart?”
Evidence-based response: No restart is necessary. The immunization series can be completed regardless of the interval between doses. Immune memory persists, and the remaining doses can be administered to complete the series. Extended intervals do not reduce vaccine effectiveness.
Post-Vaccination Patient Instructions
Immediate Care (First 24 hours)
- • Apply cold compress to injection site if needed
- • Use arm normally to prevent stiffness
- • Monitor for immediate adverse reactions
- • Take acetaminophen or ibuprofen for discomfort
- • Remain in clinic for 15 minutes after immunization
Follow-up Care
- • Schedule next dose appointment before leaving
- • Contact healthcare provider for concerning symptoms
- • Continue routine cervical cancer screening
- • Maintain vaccination record for future reference
- • Report any adverse events to healthcare provider
Side Effects, Contraindications, and Adverse Event Management
Common Side Effects (>10%)
- Local: Pain, swelling, redness at injection site
- Systemic: Fatigue, headache, myalgia
- Duration: 1-3 days, self-limiting
- Management: Symptomatic care, cold compress
Uncommon Side Effects (1-10%)
- Gastrointestinal: Nausea, vomiting, diarrhea
- Neurological: Dizziness, syncope
- Dermatological: Pruritus, urticaria
- Monitoring: Observe for resolution
Rare Side Effects (<1%)
- Allergic: Anaphylaxis (1 in 1 million)
- Neurological: Shoulder injury (SIRVA)
- Hematological: Idiopathic thrombocytopenic purpura
- Action: Immediate medical attention required
Contraindications and Precautions
Absolute Contraindications
- Severe allergic reaction to previous HPV vaccine dose
- Known severe allergy to any vaccine component
- Yeast allergy (for specific formulations)
- Current moderate to severe acute illness
Immunization should be permanently deferred for absolute contraindications
Precautions (Not Contraindications)
- Pregnancy (defer until after delivery)
- Immunocompromised status (may receive vaccine)
- History of syncope with injections
- Bleeding disorders (subcutaneous route consideration)
Benefits typically outweigh risks; individualized assessment recommended
Emergency Response Protocol for Severe Adverse Reactions
Anaphylaxis Recognition
- • Rapid onset (minutes to hours)
- • Respiratory: Wheezing, stridor, dyspnea
- • Cardiovascular: Hypotension, tachycardia
- • Dermatological: Urticaria, angioedema
- • Gastrointestinal: Vomiting, diarrhea, cramping
- • Neurological: Altered mental status
Immediate Management
- Assess airway, breathing, circulation
- Administer epinephrine 0.01 mg/kg IM (max 0.5 mg)
- Call emergency services (911)
- Position patient supine with legs elevated
- Establish IV access and administer normal saline
- Administer oxygen if available
- Prepare for second epinephrine dose if needed
- Document incident thoroughly
Memory Aid: ADVERSE Event Assessment
- A – Assess severity and timing of reaction
- D – Document all symptoms and interventions
- V – Vital signs monitoring and stabilization
- E – Emergency protocols if severe reaction
- R – Report to VAERS and healthcare provider
- S – Support patient and family throughout
- E – Educate about future immunization considerations
Clinical Considerations and Special Populations
Immunocompromised Patients
HPV vaccination is recommended for immunocompromised individuals, including those with HIV, organ transplant recipients, and patients receiving immunosuppressive therapy.
Considerations:
- • May have reduced immune response
- • Three-dose series recommended regardless of age
- • Higher risk of HPV-related malignancies
- • Monitor closely for adverse reactions
- • Coordinate with specialist care teams
Pregnancy and Lactation
HPV vaccine is not recommended during pregnancy but is safe for breastfeeding mothers.
Guidelines:
- • Defer immunization until after delivery
- • No evidence of harm if given unknowingly during pregnancy
- • Safe to administer during breastfeeding
- • Resume or start series postpartum
- • Pregnancy testing not required before vaccination
Vaccine Co-administration and Timing
| Vaccine Type | Co-administration | Site Considerations | Special Notes |
|---|---|---|---|
| Other inactivated vaccines | Simultaneous OK | Different anatomical sites | No interference with immune response |
| Live vaccines (MMR, Varicella) | Simultaneous OK | Different anatomical sites | HPV vaccine does not affect live vaccine efficacy |
| Meningococcal vaccines | Preferred | Same visit, different sites | Common adolescent immunization schedule |
| Tdap | Recommended | Different arms preferred | Adolescent platform approach |
Ages 9-14 Years
- • Optimal immunization window
- • Two-dose series (0, 6-12 months)
- • Strongest immune response
- • Routine recommendation
- • Parent/guardian consent required
Ages 15-26 Years
- • Catch-up immunization population
- • Three-dose series (0, 1-2, 6 months)
- • Shared clinical decision-making
- • Cost-effectiveness considerations
- • Individual risk assessment
Ages 27-45 Years
- • Shared clinical decision-making
- • Consider individual risk factors
- • Limited benefit if previously exposed
- • Not routinely recommended
- • Discuss with healthcare provider
Clinical Decision-Making Framework
Assessment Factors
- • Patient age and vaccination history
- • Sexual health history and risk factors
- • Immune status and comorbidities
- • Previous HPV-related disease
- • Patient preferences and concerns
Shared Decision Elements
- • Discuss benefits and limitations
- • Address individual risk assessment
- • Consider cost and insurance coverage
- • Respect patient autonomy
- • Provide evidence-based information
Documentation, Follow-up, and Quality Assurance
Required Documentation Elements
Pre-Vaccination
- • Screening questionnaire completion
- • Contraindication assessment
- • Informed consent obtained
- • Previous vaccination history verified
- • VIS (Vaccine Information Statement) provided
Vaccine Administration
- • Date and time of administration
- • Vaccine manufacturer and lot number
- • Expiration date verification
- • Route, site, and dose administered
- • Administrator name and credentials
Registry and Reporting Systems
Immunization Information Systems (IIS)
- • Report to state/local IIS within 24-48 hours
- • Ensure data accuracy and completeness
- • Support population health monitoring
- • Enable coverage assessment
Adverse Event Reporting
- • VAERS reporting for significant events
- • Document all adverse reactions
- • Follow institutional protocols
- • Maintain detailed records
Follow-up and Monitoring Protocols
Immediate Follow-up
- • 15-minute observation period
- • Monitor for immediate reactions
- • Document any adverse events
- • Provide post-vaccination instructions
- • Schedule next appointment
Short-term Follow-up
- • 24-48 hour check-in call
- • Assess for delayed reactions
- • Address patient concerns
- • Reinforce importance of series completion
- • Document outcomes
Long-term Monitoring
- • Series completion tracking
- • Reminder/recall systems
- • Coverage rate monitoring
- • Population health outcomes
- • Quality improvement initiatives
Quality Assurance Metrics and Performance Indicators
Process Metrics
- • Vaccination coverage rates by age group
- • Series completion rates
- • Time intervals between doses
- • Documentation completeness
- • Adverse event reporting timeliness
Outcome Metrics
- • Patient satisfaction scores
- • Missed opportunity reduction
- • Healthcare provider knowledge
- • Cost-effectiveness analysis
- • Population health impact
Electronic Health Record (EHR) Integration
Clinical Decision Support
- • Age-based recommendations
- • Contraindication alerts
- • Due date calculations
Order Sets
- • Standardized protocols
- • Co-administration guidance
- • Patient education materials
Registry Integration
- • Automated IIS reporting
- • Real-time data exchange
- • Coverage monitoring
Quality Reporting
- • Performance dashboards
- • Compliance tracking
- • Outcome measurement
Global Best Practices in HPV Immunization Programs
Australia’s National Program
Australia implemented the world’s first national HPV immunization program in 2007, achieving remarkable success in reducing HPV infections and related diseases.
Key Strategies:
- • School-based vaccination delivery
- • Gender-neutral vaccination policy
- • Comprehensive public education campaigns
- • Free vaccine provision
- • Strong surveillance systems
Outcomes:
- • 77% reduction in vaccine-type HPV infections
- • 50% decrease in high-grade cervical lesions
- • Significant reduction in genital warts
- • Evidence of herd immunity effects
Canada’s Provincial Approaches
Canadian provinces have implemented diverse approaches to HPV immunization, demonstrating flexibility in program design while maintaining high coverage rates.
Innovation Highlights:
- • Multi-modal delivery systems
- • Indigenous community-specific programs
- • Healthcare provider education initiatives
- • Parent engagement strategies
- • Real-time coverage monitoring
Lessons Learned:
- • Importance of stakeholder engagement
- • Cultural sensitivity in program design
- • Continuous quality improvement
- • Integration with existing health services
Low and Middle-Income Country Implementation Models
Rwanda’s School-Based Program
- • 98.5% coverage achieved in first year
- • Strong government commitment
- • Community health worker involvement
- • Integration with existing immunization infrastructure
- • Cost-effective implementation model
Kenya’s Multi-Platform Approach
- • School-based and health facility delivery
- • Community outreach programs
- • Religious leader engagement
- • Media advocacy campaigns
- • Partnership with international organizations
Bhutan’s Comprehensive Strategy
- • Integration with cervical cancer screening
- • Healthcare worker training programs
- • Parent and community education
- • Monitoring and evaluation systems
- • Sustainable financing mechanisms
World Health Organization (WHO) Strategic Framework
Core Implementation Principles
- • Target girls aged 9-14 years as primary population
- • Achieve ≥90% coverage with complete vaccine series
- • Integrate with existing immunization programs
- • Ensure sustainable financing mechanisms
- • Implement robust monitoring and evaluation systems
Global Elimination Strategy
- • 90% of girls vaccinated by age 15
- • 70% of women screened by age 35 and 45
- • 90% of women with cervical disease receive treatment
- • Comprehensive approach combining prevention and treatment
- • Country-specific implementation roadmaps
Common Implementation Challenges
- Vaccine hesitancy and misinformation
- Healthcare provider knowledge gaps
- Funding and resource constraints
- Cold chain management in remote areas
- Cultural and religious opposition
Evidence-Based Solutions
- Multi-stakeholder communication strategies
- Comprehensive provider education programs
- Public-private partnership models
- Technology solutions for supply chain management
- Community engagement and cultural adaptation
Conclusion and Future Directions
Key Takeaways for Nursing Practice
HPV vaccination represents one of the most significant advances in cancer prevention, offering nurses the opportunity to make a profound impact on public health. Effective immunization programs require comprehensive understanding of vaccine science, meticulous attention to administration protocols, and skillful patient education.
As nursing professionals, our role extends beyond vaccine administration to encompass patient advocacy, education, and quality improvement. The evidence overwhelmingly supports HPV vaccination as a safe, effective intervention that can eliminate cervical cancer and reduce the burden of other HPV-related diseases.
Essential Competencies
- Master evidence-based immunization protocols and safety procedures
- Develop effective communication strategies for diverse populations
- Recognize and manage adverse reactions appropriately
- Maintain accurate documentation and participate in quality improvement
- Stay current with evolving recommendations and best practices
Future Directions in HPV Prevention
Vaccine Development
- • Next-generation vaccines with broader protection
- • Therapeutic vaccines for existing infections
- • Alternative delivery methods (oral, intranasal)
- • Longer-lasting immune protection
Technology Integration
- • Digital health platforms for education
- • AI-powered decision support systems
- • Mobile applications for tracking and reminders
- • Telemedicine for remote populations
Global Health Impact
- • Elimination of cervical cancer as public health problem
- • Expanded access in low-resource settings
- • Integration with comprehensive cancer control
- • One Health approaches to prevention
Nursing Excellence in HPV Prevention
Through evidence-based practice, compassionate care, and commitment to continuous learning, nurses play a crucial role in achieving the global goal of eliminating cervical cancer. Every immunization administered represents hope for a healthier future and demonstrates the profound impact of nursing on population health outcomes.
