Sleep and Rest
Complete Nursing Guide to Sleep Physiology, Disorders & Care Strategies
Physiology of Sleep
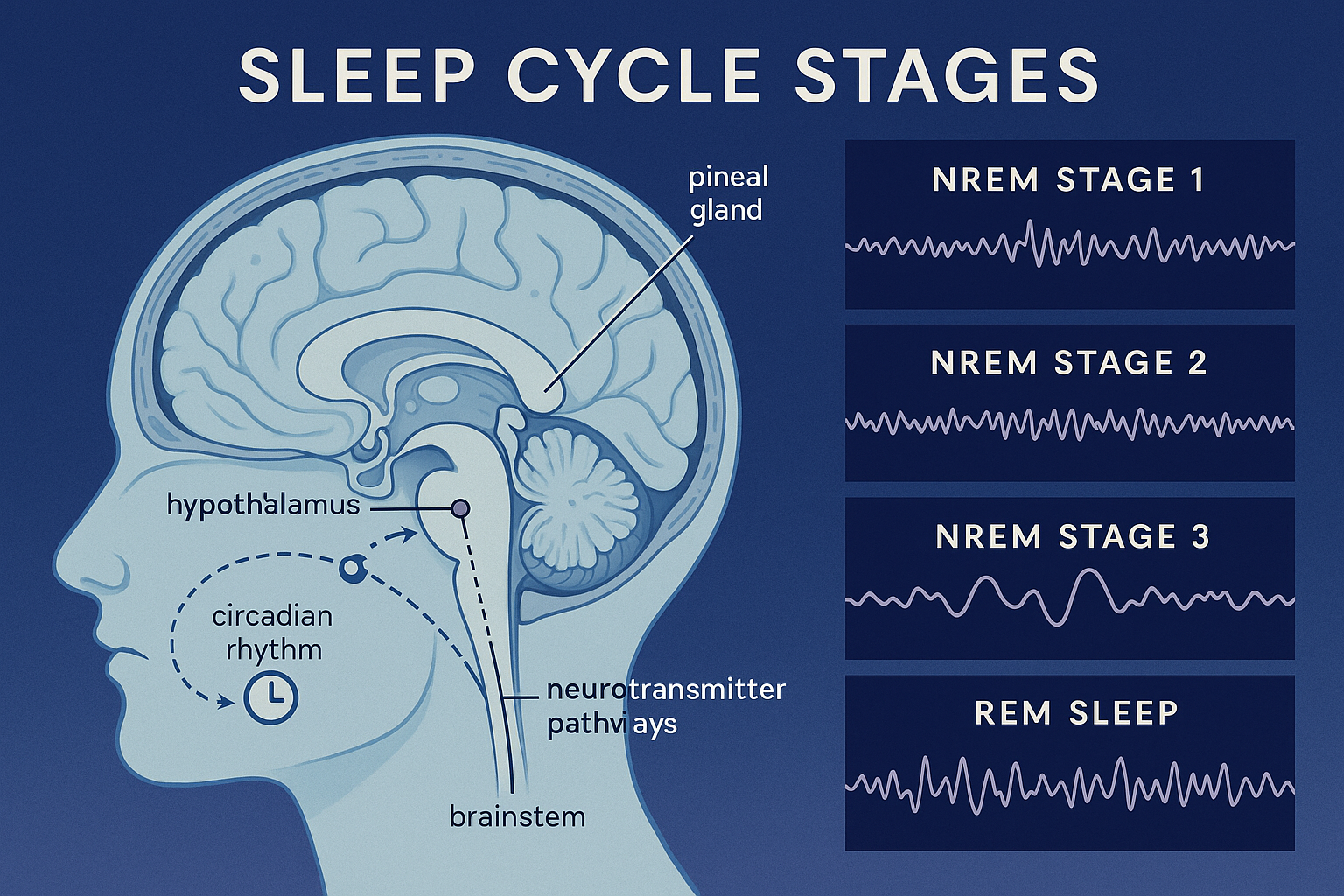
Sleep Cycle Stages and Brain Wave Patterns
Sleep is a naturally recurring state of mind and body characterized by altered consciousness, reduced sensory activity, and muscular relaxation. Understanding the complex physiology of sleep is crucial for nurses to provide optimal patient care and recognize when interventions are needed. The circadian rhythm, our internal biological clock, plays a fundamental role in regulating sleep-wake cycles and maintaining homeostasis.
🧠 Sleep Architecture
Sleep consists of two distinct states: Non-Rapid Eye Movement (NREM) and Rapid Eye Movement (REM) sleep. These stages cycle throughout the night, with each complete cycle lasting approximately 90-120 minutes. The circadian clock coordinates these cycles with environmental light-dark patterns, ensuring optimal timing for restorative processes.
| Sleep Stage | Duration | Brain Waves | Characteristics |
|---|---|---|---|
| NREM Stage 1 | 5-10 minutes | Alpha & Theta waves | Light sleep, easy to wake, drowsiness |
| NREM Stage 2 | 45-55% of sleep | Sleep spindles & K-complexes | Deeper sleep, reduced body temperature |
| NREM Stage 3 | 15-20% of sleep | Delta waves | Deep sleep, growth hormone release, tissue repair |
| REM Sleep | 20-25% of sleep | Beta waves (similar to wake) | Dreams, memory consolidation, brain development |
⚡ Neurochemistry of Sleep
Sleep regulation involves complex interactions between neurotransmitters, hormones, and brain structures. The circadian pacemaker in the suprachiasmatic nucleus (SCN) of the hypothalamus coordinates these processes with environmental cues.
💤 Melatonin
Produced by pineal gland, promotes sleepiness, regulated by light exposure
🧘 GABA
Primary inhibitory neurotransmitter, promotes calm and sleep onset
🏃 Adenosine
Builds up during wakefulness, creates sleep pressure
⚡ Acetylcholine
Promotes REM sleep and dreaming phases
🚀 Norepinephrine
Promotes wakefulness and alertness
☀️ Serotonin
Regulates mood and sleep-wake cycles
Memory Aid: Sleep Neurotransmitters
“My GABA Sleeps After Night”
- Melatonin – Sleep hormone
- GABA – Calming neurotransmitter
- Serotonin – Mood regulation
- Adenosine – Sleep pressure
- Norepinephrine – Wakefulness
🕐 Circadian Rhythm Regulation
The circadian rhythm is a 24-hour internal clock that regulates sleep-wake cycles, body temperature, hormone release, and other physiological processes. This rhythm is primarily controlled by the suprachiasmatic nucleus (SCN) in the hypothalamus, which responds to light and darkness signals from the environment. Understanding circadian rhythms is essential for nurses working with patients who have disrupted sleep patterns, such as those in intensive care units or patients with shift work sleep disorder.
Key Circadian Rhythm Facts:
- • Circadian rhythms are present in nearly all living organisms
- • Light exposure is the strongest circadian synchronizer
- • Core body temperature follows a circadian pattern
- • Disrupted circadian rhythms affect immune function
- • Age-related changes alter circadian amplitude
Factors Affecting Sleep
Multiple factors can influence sleep quality and duration, making it essential for nurses to assess these variables when caring for patients. Understanding these factors helps in developing individualized care plans and implementing appropriate interventions. Environmental, physiological, psychological, and lifestyle factors all play crucial roles in determining sleep patterns and can significantly impact the circadian rhythm regulation.
🌍 Environmental Factors
Temperature
- • Optimal: 60-67°F (15-19°C)
- • Core body temperature drops during sleep
- • Hot environments disrupt REM sleep
- • Cold environments cause frequent awakenings
Light Exposure
- • Blue light suppresses melatonin
- • Darkness triggers melatonin release
- • Light therapy can reset circadian rhythms
- • Hospital lighting affects patient sleep
Noise Levels
- • >40 dB can disrupt sleep
- • Sudden noises cause arousal
- • White noise can mask disruptive sounds
- • ICU noise levels often exceed 60 dB
Sleep Environment
- • Comfortable mattress and pillows
- • Familiar vs. unfamiliar settings
- • Privacy and security concerns
- • Air quality and ventilation
🩺 Physiological Factors
Age-Related Sleep Changes
| Age Group | Sleep Duration | Sleep Characteristics |
|---|---|---|
| Newborns (0-3 months) | 14-17 hours | 50% REM sleep, irregular patterns |
| Adults (18-64 years) | 7-9 hours | 25% REM, consolidated nighttime sleep |
| Older Adults (65+) | 7-8 hours | Decreased deep sleep, early bedtime |
🧠 Psychological Factors
Stress & Anxiety
Hyperarousal prevents sleep onset
Depression
Early morning awakening, fragmented sleep
Cognitive Load
Racing thoughts interfere with relaxation
🏃♀️ Lifestyle Factors
Sleep Promoting Factors
- ✅ Regular exercise (not close to bedtime)
- ✅ Consistent sleep schedule
- ✅ Relaxation techniques
- ✅ Avoiding large meals before bed
- ✅ Limiting fluid intake evening
Sleep Disrupting Factors
- ❌ Caffeine consumption (especially afternoon)
- ❌ Alcohol consumption
- ❌ Smoking/nicotine use
- ❌ Irregular sleep schedules
- ❌ Screen time before bed
⚕️ Medical Conditions Affecting Sleep
Respiratory
- • Sleep apnea
- • COPD
- • Asthma
Cardiovascular
- • Heart failure
- • Hypertension
- • Arrhythmias
Neurological
- • Parkinson’s disease
- • Dementia
- • Stroke
Endocrine
- • Diabetes
- • Thyroid disorders
- • Menopause
Pain Conditions
- • Chronic pain
- • Arthritis
- • Fibromyalgia
GI Disorders
- • GERD
- • Peptic ulcers
- • IBS
Promoting Rest and Sleep
Promoting optimal rest and sleep is a fundamental nursing responsibility that directly impacts patient recovery, immune function, and overall well-being. Effective sleep promotion strategies require a comprehensive understanding of sleep hygiene principles, environmental modifications, and individualized interventions. By supporting healthy circadian rhythms and addressing barriers to sleep, nurses can significantly improve patient outcomes and quality of life.
🛏️ Sleep Hygiene Principles
The 4 Pillars of Sleep Hygiene
Consistency
Regular sleep-wake schedule
Environment
Optimal sleep setting
Habits
Healthy lifestyle choices
Relaxation
Pre-sleep wind-down
🏥 Hospital-Specific Sleep Interventions
Environmental Modifications
- Dim lights during evening hours to support circadian rhythm
- Use earplugs or white noise machines
- Maintain comfortable room temperature
- Provide privacy with curtains/screens
- Minimize unnecessary nighttime interruptions
Nursing Care Strategies
- Cluster care activities to minimize disruptions
- Schedule medications to avoid sleep interruption
- Provide comfort measures (positioning, pillows)
- Address pain and discomfort proactively
- Encourage relaxation techniques
📋 Sleep Assessment Tools
| Assessment Tool | Purpose | Key Components | Clinical Use |
|---|---|---|---|
| Pittsburgh Sleep Quality Index (PSQI) | Overall sleep quality assessment | Sleep duration, latency, efficiency, disturbances | Comprehensive sleep evaluation |
| Epworth Sleepiness Scale | Daytime sleepiness measurement | Likelihood of dozing in various situations | Screen for sleep disorders |
| Sleep Diary | Track sleep patterns over time | Bedtime, wake time, sleep quality ratings | Monitor progress and identify patterns |
| STOP-BANG Questionnaire | Sleep apnea screening | Snoring, tiredness, observed apnea, BMI | Identify high-risk patients |
🌿 Non-Pharmacological Interventions
🧘♀️ Relaxation Techniques
- • Progressive muscle relaxation
- • Deep breathing exercises
- • Guided imagery
- • Meditation and mindfulness
💡 Light Therapy
- • Morning bright light exposure
- • Circadian rhythm regulation
- • Seasonal affective disorder treatment
- • Shift work adaptation
🎵 Sound Therapy
- • White noise machines
- • Nature sounds
- • Calming music
- • Noise masking techniques
Cognitive Behavioral Therapy for Insomnia (CBT-I)
Cognitive Components
- • Challenge negative thoughts about sleep
- • Address sleep-related anxiety
- • Develop realistic sleep expectations
- • Education about sleep myths
Behavioral Components
- • Sleep restriction therapy
- • Stimulus control techniques
- • Sleep hygiene education
- • Relaxation training
Memory Aid: Sleep Promotion Strategies
“SLEEP TIGHT”
- Schedule – Consistent sleep-wake times
- Light – Manage light exposure for circadian rhythms
- Environment – Optimize sleep setting
- Exercise – Regular physical activity (not before bed)
- Pain – Address discomfort and pain
- Temperature – Maintain cool room temperature
- Interruptions – Minimize nighttime disturbances
- Guidance – Provide sleep education
- Habits – Promote healthy sleep behaviors
- Tranquility – Encourage relaxation techniques
Sleep Disorders
Sleep disorders affect millions of people worldwide and can significantly impact health, safety, and quality of life. As nurses, understanding the pathophysiology, assessment, and management of common sleep disorders is essential for providing comprehensive patient care. These disorders often disrupt normal circadian rhythm patterns and require specialized interventions to restore healthy sleep architecture.
📋 Classification of Sleep Disorders
Insomnia Disorders
- • Acute insomnia
- • Chronic insomnia
- • Comorbid insomnia
Sleep-Related Breathing
- • Obstructive sleep apnea
- • Central sleep apnea
- • Sleep hypoventilation
Hypersomnolence
- • Narcolepsy
- • Idiopathic hypersomnia
- • Klein-Levin syndrome
Circadian Rhythm
- • Delayed sleep phase
- • Advanced sleep phase
- • Shift work disorder
🔍 Common Sleep Disorders
Insomnia
Definition
Difficulty initiating or maintaining sleep, or early morning awakening with inability to return to sleep, resulting in daytime impairment.
Types
- • Acute: <30 days
- • Chronic: ≥3 nights/week for ≥3 months
- • Comorbid: Associated with other conditions
Nursing Interventions
- • Sleep hygiene education
- • CBT-I techniques
- • Environmental modifications
- • Stress management
Obstructive Sleep Apnea (OSA)
Pathophysiology
Repetitive episodes of complete or partial upper airway obstruction during sleep, leading to:
- • Oxygen desaturation
- • Sleep fragmentation
- • Sympathetic nervous system activation
- • Disrupted circadian rhythm patterns
Clinical Manifestations
- • Loud snoring with gasping
- • Witnessed apneic episodes
- • Excessive daytime sleepiness
- • Morning headaches
- • Mood changes, irritability
- • Cognitive impairment
Treatment Options
First-Line
- • CPAP therapy
- • Weight reduction
- • Positional therapy
Alternative
- • Oral appliances
- • BiPAP devices
- • Lifestyle modifications
Surgical
- • UPPP surgery
- • Hypoglossal nerve stimulation
- • Maxillomandibular advancement
Narcolepsy
Core Symptoms (Tetrad)
-
1
Excessive Daytime Sleepiness: Overwhelming urge to sleep
-
2
Cataplexy: Sudden loss of muscle tone triggered by emotions
-
3
Sleep Paralysis: Temporary inability to move upon awakening
-
4
Hypnagogic Hallucinations: Vivid dreams at sleep onset
Management Strategies
- • Scheduled naps (15-20 minutes)
- • Regular sleep schedule
- • Stimulant medications
- • Safety precautions (driving restrictions)
- • Support group referrals
- • Workplace accommodations
Circadian Rhythm Sleep-Wake Disorders
These disorders involve misalignment between the person’s circadian rhythm and the external environment, resulting in sleep difficulties and daytime impairment.
Delayed Sleep-Wake Phase
- • Sleep onset: 2-6 AM
- • Wake time: 10 AM-2 PM
- • Common in adolescents
- • Treatment: Light therapy, melatonin
Advanced Sleep-Wake Phase
- • Sleep onset: 6-9 PM
- • Wake time: 2-5 AM
- • Common in elderly
- • Treatment: Evening light exposure
Shift Work Sleep Disorder
- • Rotating or night shifts
- • Insomnia and excessive sleepiness
- • Affects 10-40% of shift workers
- • Treatment: Strategic light, napping
📝 Nursing Assessment and Documentation
Comprehensive Sleep Assessment Components
Subjective Data
- • Sleep habits and patterns
- • Sleep quality rating (1-10 scale)
- • Daytime symptoms and functioning
- • Sleep environment description
- • Medications and substances
- • Stress levels and coping
Objective Data
- • Physical examination findings
- • Vital signs and BMI
- • Observed sleep behaviors
- • Sleep study results if available
- • Actigraphy data
- • Laboratory values (if indicated)
💊 Treatment Modalities
| Treatment Category | Examples | Indications | Nursing Considerations |
|---|---|---|---|
| Non-pharmacological | CBT-I, sleep hygiene, relaxation | First-line for chronic insomnia | Patient education, compliance monitoring |
| Pharmacological | Zolpidem, melatonin, antidepressants | Short-term insomnia, specific disorders | Monitor for side effects, dependency |
| Medical Devices | CPAP, BiPAP, oral appliances | Sleep apnea, breathing disorders | Equipment training, compliance support |
| Light Therapy | Bright light boxes, dawn simulators | Circadian rhythm disorders | Timing instructions, safety precautions |
Global Best Practices in Sleep Care
Healthcare systems worldwide have implemented innovative approaches to improve sleep care quality and patient outcomes. These evidence-based practices demonstrate the global commitment to addressing sleep health as a fundamental component of overall wellness and recovery.
Scandinavian Countries
“Quiet Time” Protocols
Hospitals implement structured quiet periods from 10 PM to 6 AM, with dimmed lighting, reduced noise levels, and clustered care activities to support natural circadian rhythms.
- • 40% reduction in sleep disruptions
- • Improved patient satisfaction scores
- • Decreased delirium rates in ICU patients
Japan
Sleep-Friendly Hospital Design
Integration of traditional Japanese design principles with modern sleep science, including natural materials, optimal acoustics, and circadian lighting systems.
- • Automated lighting that mimics natural patterns
- • Sound-dampening materials in patient rooms
- • Meditation spaces for relaxation
Canada
Sleep Champion Programs
Specialized nursing roles dedicated to sleep health, with advanced training in sleep assessment, intervention, and patient education across all care settings.
- • Dedicated sleep health specialists
- • Comprehensive sleep screening protocols
- • Staff education and mentorship programs
Netherlands
Technology Integration
Advanced use of wearable technology and smart room systems to monitor and optimize sleep environments in real-time for hospitalized patients.
- • Real-time sleep quality monitoring
- • Automated environmental adjustments
- • Data-driven care plan modifications
Evidence-Based Outcomes from Global Practices
Improvement in sleep quality scores
Reduction in length of stay
Decrease in readmission rates
Key Takeaways for Nursing Practice
Understand Physiology
Master sleep architecture and circadian rhythm regulation
Comprehensive Assessment
Evaluate all factors affecting patient sleep quality
Holistic Interventions
Implement evidence-based sleep promotion strategies
Recognize Disorders
Identify and manage common sleep disorders
Patient Education
Teach sleep hygiene and self-management strategies
Monitor Outcomes
Evaluate intervention effectiveness and adjust care plans
“Quality sleep is not a luxury—it’s a fundamental human need and a cornerstone of optimal health and recovery.”
