Diabetes Mellitus
Comprehensive Nursing Notes
A Complete Guide for Nursing Students
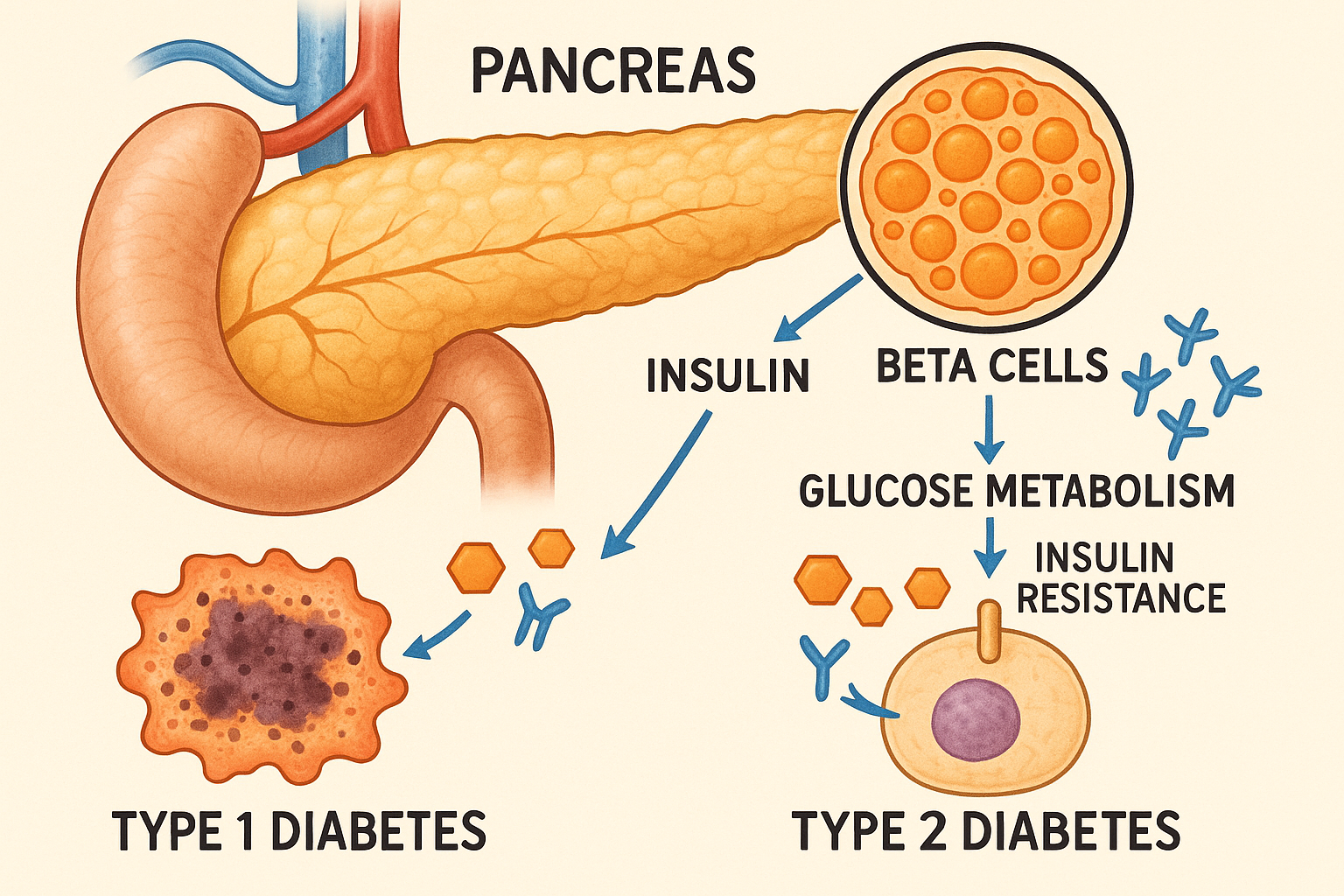
Comprehensive illustration showing pancreatic beta cells, insulin pathways, and diabetes mechanisms
Learning Objectives
- Understand Type 1 & Type 2 Diabetes
- Recognize Symptoms & Complications
- Master Management Strategies
- Perform Diagnostic Investigations
- Interpret OGTT Results
- Understand HbA1c Significance
- Manage Hypoglycemia
- Apply Nursing Interventions
Introduction to Diabetes Mellitus
Diabetes Mellitus is a group of metabolic disorders characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. It affects over 463 million people worldwide and represents one of the most significant health challenges of the 21st century. As nursing professionals, understanding diabetes is crucial for providing comprehensive patient care and education.
Key Definition
Diabetes Mellitus is defined as a fasting plasma glucose ≥126 mg/dL (7.0 mmol/L) or a 2-hour plasma glucose ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test, or HbA1c ≥6.5% (48 mmol/mol).
Pathophysiology of Diabetes
Normal Glucose Homeostasis
- Pancreatic β-cells secrete insulin
- Insulin facilitates glucose uptake
- Glucose stored as glycogen
- Blood glucose maintained 70-110 mg/dL
Diabetic Dysfunction
- Impaired insulin secretion/action
- Decreased glucose uptake
- Increased hepatic glucose production
- Chronic hyperglycemia
Type 1 vs Type 2 Diabetes
Type 1 Diabetes
Pathogenesis
Autoimmune destruction of pancreatic β-cells leading to absolute insulin deficiency.
- • T-cell mediated destruction
- • Genetic predisposition (HLA-DR3, HLA-DR4)
- • Environmental triggers (viruses, stress)
Characteristics
- • Age of onset: Usually <30 years
- • Body weight: Normal or underweight
- • Onset: Acute, rapid
- • Ketosis: Prone to DKA
- • Insulin requirement: Absolute
Clinical Pearl
Remember “THIN” – Type 1 patients are typically Thin, Have Insulin deficiency, and Need insulin immediately.
Type 2 Diabetes
Pathogenesis
Insulin resistance with progressive β-cell dysfunction and relative insulin deficiency.
- • Peripheral insulin resistance
- • Impaired insulin secretion
- • Increased hepatic glucose production
Characteristics
- • Age of onset: Usually >40 years
- • Body weight: Often obese
- • Onset: Insidious, gradual
- • Ketosis: Rare, except under stress
- • Insulin requirement: May be needed
Clinical Pearl
Remember “THICK” – Type 2 patients are typically Thick (obese), Have Insulin resistance, and Can be managed with lifestyle changes initially.
Symptoms and Clinical Presentation
Memory Aid: “4 P’s of Diabetes”
Primary Symptoms
- Polyuria – Excessive urination
- Polydipsia – Excessive thirst
- Polyphagia – Excessive hunger
- Pound loss – Unexplained weight loss
Secondary Symptoms
- Blurred vision
- Fatigue and weakness
- Slow-healing wounds
- Frequent infections
Polyuria
Mechanism: Osmotic diuresis due to glycosuria
Threshold: Blood glucose >180 mg/dL
Frequency: >3L/day or >50mL/kg/day
Polydipsia
Mechanism: Compensatory response to dehydration
Trigger: Increased plasma osmolality
Volume: Often >3-4L/day
Polyphagia
Mechanism: Cellular starvation despite hyperglycemia
Cause: Ineffective glucose utilization
Paradox: Increased hunger with weight loss
Complications of Diabetes
Acute Complications
Diabetic Ketoacidosis (DKA)
Triad: Hyperglycemia, Ketonemia, Acidosis
Glucose: >250 mg/dL
pH: <7.3
Ketones: >3 mmol/L
Mortality: 1-5%
Hyperosmolar Hyperglycemic State (HHS)
Glucose: >600 mg/dL
Osmolality: >320 mOsm/kg
pH: >7.3 (no significant ketosis)
Mortality: 5-20%
Hypoglycemia
Definition: <70 mg/dL
Severe: <54 mg/dL
Symptoms: Sweating, palpitations, confusion
Treatment: 15g fast-acting carbs
Chronic Complications
Microvascular
- Retinopathy: Leading cause of blindness
- Nephropathy: CKD, dialysis, transplant
- Neuropathy: Peripheral, autonomic
Macrovascular
- CAD: 2-4x increased risk
- Stroke: 2-3x increased risk
- PAD: Amputation risk
Other Complications
- Increased infection risk
- Periodontal disease
- Depression (2x risk)
Management of Diabetes
Type 1 Management
Insulin Therapy
| Type | Onset | Peak | Duration |
|---|---|---|---|
| Rapid-Acting | 15 min | 1-2 hr | 3-4 hr |
| Short-Acting | 30-60 min | 2-4 hr | 5-8 hr |
| Long-Acting | 2 hr | No peak | 24 hr |
Basal-Bolus Regimen
- • Basal: 40-50% of total daily dose
- • Bolus: 50-60% divided among meals
- • Correction factor: 1800 rule
- • Carb ratio: 500 rule
Type 2 Management
Stepwise Approach
Medication Classes
- • Metformin: First-line, ↓ hepatic glucose
- • Sulfonylureas: ↑ insulin secretion
- • SGLT2i: ↑ glucose excretion
- • GLP-1 RA: ↑ insulin, ↓ glucagon
- • DPP-4i: ↑ incretin activity
Glycemic Targets
HbA1c
<7%
(53 mmol/mol)
Fasting Glucose
80-130
mg/dL
Postprandial
<180
mg/dL
Investigations of Diabetes Mellitus
Oral Glucose Tolerance Test (OGTT)
Indications
- • Impaired fasting glucose (100-125 mg/dL)
- • Gestational diabetes screening
- • Borderline HbA1c (5.7-6.4%)
- • Strong family history + normal glucose
- • Polycystic ovary syndrome
- • Previous gestational diabetes
Procedure
- 1. Preparation: 8-12 hour fast
- 2. Baseline: Draw fasting glucose
- 3. Load: 75g glucose solution
- 4. Timing: Draw at 1hr, 2hr
- 5. Activity: Patient sits quietly
- 6. Restrictions: No smoking/caffeine
Interpretation
| Category | Fasting (mg/dL) | 2-Hour (mg/dL) | HbA1c (%) |
|---|---|---|---|
| Normal | <100 | <140 | <5.7 |
| Prediabetes | 100-125 | 140-199 | 5.7-6.4 |
| Diabetes | ≥126 | ≥200 | ≥6.5 |
Types of GTT Curves
Normal Curve
- • Fasting: 70-100 mg/dL
- • Peak: 120-140 mg/dL at 1 hour
- • 2-hour: Returns to <140 mg/dL
- • Shape: Smooth rise and fall
Diabetic Curve
- • Fasting: ≥126 mg/dL
- • Peak: >200 mg/dL sustained
- • 2-hour: ≥200 mg/dL
- • Shape: High, delayed return
Special GTT Variations
Mini GTT
- • Dose: 50g glucose
- • Duration: 1 hour only
- • Use: Screening test
- • Threshold: <140 mg/dL normal
Extended GTT
- • Duration: 3-5 hours
- • Samples: Every 30-60 minutes
- • Use: Reactive hypoglycemia
- • Indication: Post-prandial symptoms
Glucose Challenge Test (GCT)
- • Timing: 24-28 weeks gestation
- • Dose: 50g glucose (non-fasting)
- • Threshold: ≥140 mg/dL abnormal
- • Follow-up: 3-hour OGTT if positive
Intravenous GTT (IVGTT)
- • Route: IV glucose bolus
- • Advantage: Bypasses GI absorption
- • Use: Research, malabsorption
- • Calculation: K-value (glucose disposal)
HbA1c (Hemoglobin A1c)
Definition of HbA1c
HbA1c is a form of hemoglobin that is covalently bound to glucose. It represents the average plasma glucose concentration over the preceding 2-3 months, providing a reliable measure of long-term glycemic control.
Formation Process
- • Non-enzymatic glycation of hemoglobin
- • Irreversible process
- • Proportional to glucose exposure
- • Reflects 120-day RBC lifespan
Clinical Significance
- • Diagnostic tool (≥6.5% = diabetes)
- • Monitoring glycemic control
- • Predicts complications risk
- • No fasting required
Normal
<5.7%
(<39 mmol/mol)
Prediabetes
5.7-6.4%
(39-47 mmol/mol)
Diabetes
≥6.5%
(≥48 mmol/mol)
Hypoglycemia
Definition
Glucose Levels
- • Level 1: 54-69 mg/dL (3.0-3.8 mmol/L)
- • Level 2: <54 mg/dL (<3.0 mmol/L)
- • Level 3: Severe cognitive impairment
Whipple’s Triad
- 1. Symptoms consistent with hypoglycemia
- 2. Low plasma glucose level
- 3. Resolution with glucose administration
Causes
Diabetes-Related
- • Insulin overdose
- • Sulfonylurea excess
- • Missed meals
- • Excessive exercise
- • Alcohol consumption
Non-Diabetes Related
- • Insulinoma
- • Adrenal insufficiency
- • Liver disease
- • Renal failure
- • Sepsis
Hypoglycemia Symptoms: “SWEATING”
Autonomic Symptoms
- Sweating, shakiness
- Weakness, fatigue
- Excess hunger
- Anxiety, irritability
Neuroglycopenic
- Tremor, palpitations
- Inability to concentrate
- Neurological changes
- Gait instability, coma
Nursing Implementation in Diabetes Care
Assessment & Monitoring
Glucose Monitoring
- • Capillary blood glucose testing
- • Continuous glucose monitoring (CGM)
- • Urine ketones in Type 1 diabetes
- • Document patterns and trends
Physical Assessment
- • Foot examination daily
- • Skin integrity assessment
- • Vital signs monitoring
- • Weight and BMI tracking
Patient Education
Nutrition Education
- • Carbohydrate counting
- • Meal planning and timing
- • Reading food labels
- • Portion control techniques
Medication Management
- • Insulin administration techniques
- • Rotation of injection sites
- • Proper storage of medications
- • Recognition of side effects
Emergency Management
Hypoglycemia Protocol
- 1. Assess: Glucose <70 mg/dL
- 2. Treat: 15g fast-acting carbs
- 3. Wait: 15 minutes
- 4. Recheck: Blood glucose
- 5. Repeat: If still <70 mg/dL
- 6. Follow-up: Complex carbs/meal
DKA Recognition
- • Symptoms: N/V, abdominal pain
- • Signs: Kussmaul breathing, fruity odor
- • Labs: Glucose >250, ketones +
- • Action: Immediate physician notification
Documentation Requirements
Glucose Monitoring
- • Time and glucose value
- • Relation to meals
- • Insulin given
- • Patient response
Patient Teaching
- • Topics covered
- • Patient understanding
- • Return demonstration
- • Areas needing reinforcement
Complications
- • Signs and symptoms
- • Interventions provided
- • Patient outcome
- • Physician notification
Clinical Pearls for Nursing Practice
Quick Assessment Tips
- Hyperglycemia: “Hot and dry, sugar high”
- Hypoglycemia: “Cold and clammy, need some candy”
- DKA breath: Fruity/acetone odor
- Foot care: Daily inspection essential
- Sick day rules: Never skip insulin
Monitoring Priorities
- Blood glucose: Before meals and bedtime
- Ketones: When glucose >250 mg/dL
- Blood pressure: Target <130/80
- Lipids: LDL <100 mg/dL
- Kidney function: Annual screening
Summary
Key Takeaways
- Diabetes is a complex metabolic disorder requiring comprehensive management
- Early recognition and intervention prevent complications
- Patient education is crucial for successful diabetes management
- Regular monitoring and assessment guide treatment decisions
Nursing Excellence
- Master glucose monitoring techniques and interpretation
- Develop expertise in patient education and counseling
- Recognize and respond to diabetes emergencies
- Advocate for patients and their families
Continue Learning
These comprehensive notes provide a foundation for excellent diabetes care. Remember to always follow your institution’s protocols and evidence-based guidelines for optimal patient outcomes.
