Vitamin Deficiency Disorders
Comprehensive Nursing Study Notes
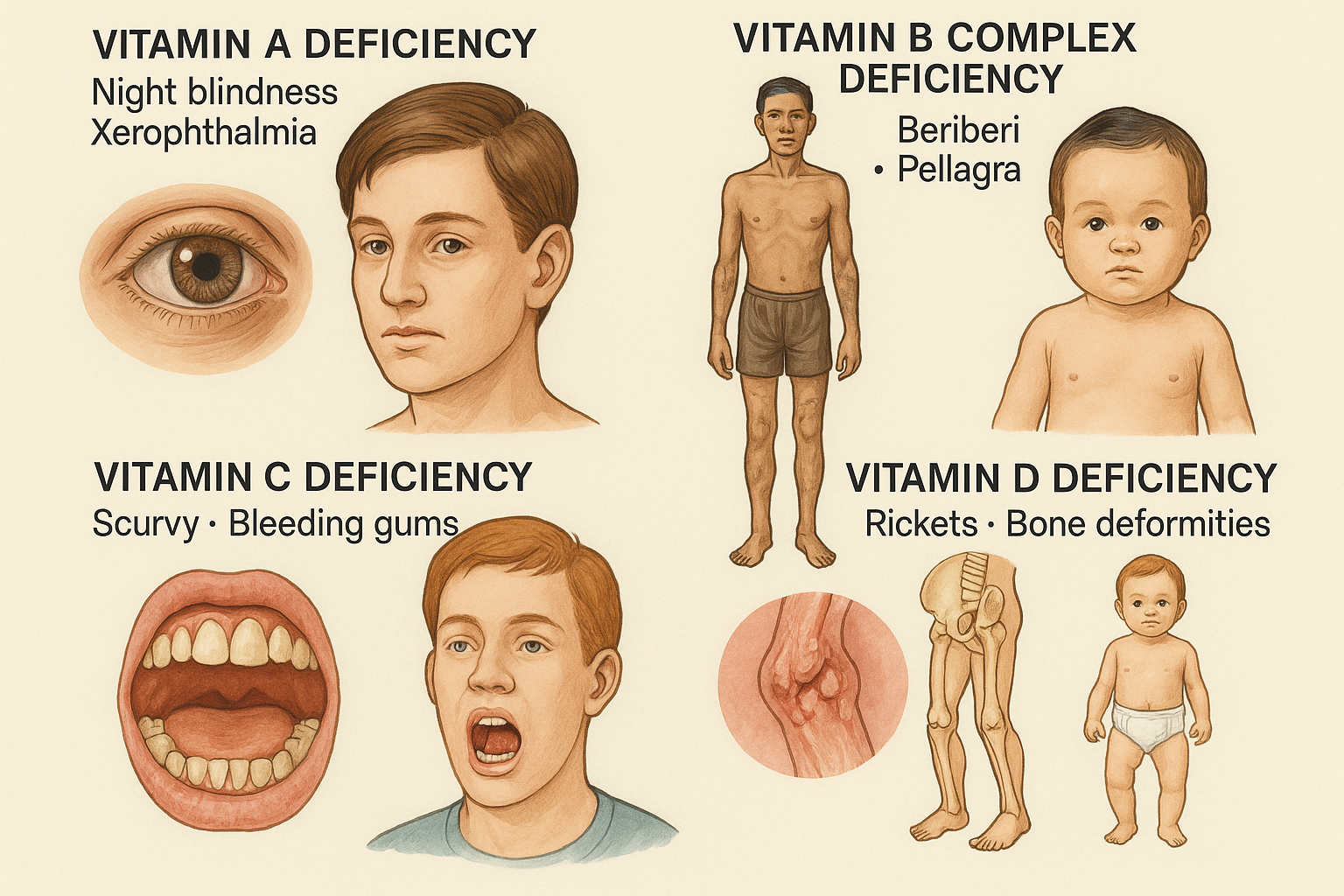
Overview of Major Vitamin Deficiency Disorders
Introduction to Vitamin Deficiency Disorders
Vitamin deficiency disorders represent a significant global health challenge, affecting millions of people worldwide. As nursing professionals, understanding these conditions is crucial for providing comprehensive patient care, early recognition, and effective intervention strategies. This comprehensive guide covers the four major vitamin deficiency disorders: Vitamin A, B-complex, C, and D deficiencies.
Key Learning Objectives
- Identify causes and risk factors for each vitamin deficiency
- Recognize signs and symptoms for early detection
- Understand management and treatment protocols
- Implement prevention strategies
- Apply nursing interventions and patient education
Master Mnemonic: “ABCD Prevention”
Assess nutrition status regularly
Balanced diet education
Community health promotion
Detect early signs and symptoms
Vitamin A Deficiency
Xerophthalmia and Night Blindness
Causes and Risk Factors
Primary Causes
- • Inadequate dietary intake of vitamin A-rich foods
- • Poor absorption due to malabsorption syndromes
- • Chronic liver disease affecting vitamin A storage
- • Protein-energy malnutrition
High-Risk Populations
- • Children under 5 years old
- • Pregnant and lactating women
- • Individuals with chronic diarrhea
- • Populations in developing countries
Signs and Symptoms
Ocular Manifestations
- • Night blindness (nyctalopia)
- • Xerophthalmia (dry eyes)
- • Bitot’s spots
- • Corneal ulceration
- • Keratomalacia
Systemic Manifestations
- • Follicular hyperkeratosis
- • Increased susceptibility to infections
- • Growth retardation in children
- • Reproductive dysfunction
- • Anemia
Management and Treatment
Vitamin A Supplementation Protocols
| Age Group | Dosage | Frequency |
|---|---|---|
| 6-11 months | 100,000 IU | Single dose |
| 12-59 months | 200,000 IU | Every 6 months |
| Adults | 10,000 IU | Daily for 2 weeks |
Emergency Treatment
For severe deficiency with corneal involvement, immediate high-dose vitamin A supplementation is critical to prevent permanent blindness.
Prevention Strategies
Dietary Sources
- • Liver and organ meats
- • Fish liver oils
- • Fortified dairy products
- • Eggs
- • Dark green leafy vegetables
- • Orange vegetables (carrots, sweet potatoes)
- • Yellow fruits (mangoes, papayas)
- • Red palm oil
Nursing Role and Interventions
Assessment
- • Comprehensive nutritional assessment
- • Visual acuity testing
- • Skin and mucous membrane examination
- • Growth monitoring in children
Intervention
- • Administer vitamin A supplements as prescribed
- • Monitor for signs of toxicity
- • Coordinate with dietitian for meal planning
- • Educate on food preparation methods
Evaluation
- • Improvement in night vision
- • Resolution of xerophthalmia
- • Adequate dietary intake
- • Reduced infection rates
Vitamin A Mnemonic: “NIGHT”
Night blindness
Infections increase
Growth retardation
Hyperkeratosis
Tear production decreased
Vitamin B Complex Deficiency
Beriberi, Pellagra, and Neurological Disorders
Important Note
B-complex vitamins work synergistically and deficiencies often occur together. Each B vitamin has specific functions and deficiency symptoms.
Major B-Complex Deficiencies
Thiamine (B1) Deficiency – Beriberi
- • Congestive heart failure
- • Peripheral edema
- • Tachycardia
- • Dyspnea
- • Peripheral neuropathy
- • Muscle weakness
- • Wrist drop, foot drop
- • Confabulation
Riboflavin (B2) Deficiency
- • Angular cheilitis (cracks at mouth corners)
- • Glossitis (inflamed tongue)
- • Seborrheic dermatitis
- • Photophobia
- • Corneal vascularization
Niacin (B3) Deficiency – Pellagra
Dermatitis, Diarrhea, Dementia, Death
Additional B-Complex Deficiencies
Pyridoxine (B6) Deficiency
- • Peripheral neuropathy
- • Seborrheic dermatitis
- • Confusion and irritability
- • Microcytic anemia
- • Seizures in infants
Cobalamin (B12) Deficiency
- • Megaloblastic anemia
- • Subacute combined degeneration
- • Peripheral neuropathy
- • Psychiatric symptoms
- • Glossitis
Folate (B9) Deficiency
- • Megaloblastic anemia
- • Neural tube defects in pregnancy
- • Glossitis
- • Diarrhea
- • Poor wound healing
Treatment Protocols
B-Complex Supplementation
| Vitamin | Deficiency Dose | Maintenance Dose |
|---|---|---|
| Thiamine (B1) | 100mg IV/IM daily | 1-2mg PO daily |
| Riboflavin (B2) | 10-20mg PO daily | 1.3-1.7mg daily |
| Niacin (B3) | 300-500mg PO daily | 14-18mg daily |
| B12 | 1000mcg IM weekly | 2.4mcg daily |
| Folate (B9) | 5mg PO daily | 400mcg daily |
Dietary Sources
Nursing Management
Assessment Priorities
Intervention Strategies
- • Immediate thiamine for suspected Wernicke’s encephalopathy
- • Cardiac monitoring for wet beriberi
- • Neurological monitoring for B12 deficiency
- • Medication administration and monitoring
- • Nutritional counseling and education
- • Symptom monitoring and documentation
B-Complex Mnemonic: “BRAIN POWER”
B1 – Beriberi (heart and nerves)
Riboflavin (B2) – Red, raw tongue
Anemia (B12, folate)
Infections increase
Niacin (B3) – 4 D’s of pellagra
Pyridoxine (B6) – Peripheral neuropathy
Oral lesions (multiple B vitamins)
Wernicke’s encephalopathy (B1)
Energy metabolism affected
Red blood cell formation (B12, folate)
Vitamin C Deficiency
Scurvy and Collagen Disorders
Pathophysiology
Role of Vitamin C
- • Essential for collagen synthesis
- • Antioxidant properties
- • Enhances iron absorption
- • Immune system support
- • Wound healing acceleration
Risk Factors
- • Inadequate fruit and vegetable intake
- • Chronic illness and stress
- • Smoking (increases requirement)
- • Alcoholism
- • Elderly populations
- • Food processing and storage issues
Clinical Manifestations
Early Signs
- • Fatigue and weakness
- • Irritability
- • Weight loss
- • Muscle and joint pain
- • Delayed wound healing
Advanced Scurvy
- • Petechial hemorrhages
- • Gum bleeding and swelling
- • Loosening of teeth
- • Bone pain and deformities
- • Impaired wound healing
Treatment and Management
Vitamin C Supplementation
| Condition | Dose | Duration |
|---|---|---|
| Scurvy Treatment | 300-1000mg daily | Until symptoms resolve |
| Prevention | 65-90mg daily | Ongoing |
| Smokers | 125mg daily | Ongoing |
| Pregnancy | 85mg daily | Throughout pregnancy |
Monitoring Parameters
- • Clinical symptom resolution
- • Wound healing progress
- • Gum health improvement
- • Serum vitamin C levels
- • Iron status (vitamin C enhances absorption)
Dietary Sources and Prevention
Excellent Sources (>90mg/100g)
- • Guava
- • Kiwi fruit
- • Citrus fruits
- • Strawberries
- • Papaya
- • Red bell peppers
- • Broccoli
- • Brussels sprouts
- • Cauliflower
- • Cabbage
Important Notes
- • Vitamin C is water-soluble and heat-sensitive
- • Cooking and storage reduce vitamin C content
- • Fresh, raw fruits and vegetables are best sources
- • Smokers need 35mg additional vitamin C daily
Nursing Care Plan
Assessment
- • Oral cavity examination
- • Skin assessment for petechiae
- • Wound healing evaluation
- • Nutritional intake assessment
- • Pain assessment
Interventions
- • Administer vitamin C supplements
- • Provide oral care for gum health
- • Wound care and monitoring
- • Dietary education and counseling
- • Pain management
Outcomes
- • Improved wound healing
- • Reduced bleeding and bruising
- • Better oral health
- • Increased energy levels
- • Adequate dietary intake
Vitamin C Mnemonic: “SCURVY”
Scorbutic gums (bleeding, swollen)
Collagen defects
Unhealed wounds
Redness and petechiae
Vitamin C deficiency
Yellow teeth, loose teeth
Vitamin D Deficiency
Rickets, Osteomalacia, and Bone Health
Pathophysiology and Causes
Vitamin D Metabolism
- • Skin synthesis via UV-B exposure
- • Dietary intake (limited sources)
- • Liver hydroxylation (25-OH-D3)
- • Kidney activation (1,25-(OH)2-D3)
- • Calcium and phosphorus homeostasis
Risk Factors
- • Limited sun exposure
- • Dark skin pigmentation
- • Geographical location (high latitude)
- • Age (elderly, infants)
- • Dietary restrictions
- • Malabsorption syndromes
- • Chronic kidney or liver disease
- • Medications (anticonvulsants, steroids)
Clinical Manifestations
Children (Rickets)
- • Delayed tooth eruption
- • Dental caries
- • Bone deformities (bow legs, knock knees)
- • Enlarged wrists and ankles
- • Delayed growth
- • Muscle weakness
- • Increased fracture risk
Adults (Osteomalacia)
- • Bone pain and tenderness
- • Muscle weakness
- • Increased fracture risk
- • Osteoporosis
- • Fatigue
- • Depression
- • Immune dysfunction
Treatment Protocols
Vitamin D Supplementation
| Population | Deficiency Treatment | Maintenance |
|---|---|---|
| Infants (0-12 months) | 2000 IU/day × 6 weeks | 400-1000 IU/day |
| Children (1-18 years) | 2000 IU/day × 6 weeks | 600-1000 IU/day |
| Adults (19-70 years) | 6000 IU/day × 8 weeks | 1500-2000 IU/day |
| Elderly (>70 years) | 6000 IU/day × 8 weeks | 2000 IU/day |
Laboratory Values
- • Serum 25(OH)D3 levels:
- – Deficiency: <20 ng/mL (<50 nmol/L)
- – Insufficiency: 20-29 ng/mL (50-74 nmol/L)
- – Sufficiency: 30-100 ng/mL (75-250 nmol/L)
- • Elevated alkaline phosphatase
- • Elevated parathyroid hormone (PTH)
- • Low or normal serum calcium
Prevention Strategies
Sun Exposure Guidelines
- • 10-30 minutes of midday sun exposure
- • Several times per week
- • Expose arms, legs, or back
- • Without sunscreen initially
- • Avoid overexposure and burning
Dietary Sources
- • Fatty fish (salmon, mackerel)
- • Fish liver oils
- • Egg yolks
- • Mushrooms (UV-treated)
- • Fortified milk and dairy
- • Fortified cereals
- • Fortified plant milks
- • Fortified margarine
Comprehensive Nursing Care
Assessment Focus Areas
Musculoskeletal System
- • Bone deformities in children
- • Muscle weakness and pain
- • Gait abnormalities
- • Fracture history
- • Joint pain and stiffness
Risk Assessment
- • Sun exposure habits
- • Dietary intake patterns
- • Medication history
- • Chronic disease presence
- • Age and ethnicity factors
Intervention Strategies
Immediate Actions
- • Assess for tetany and seizures
- • Fall risk evaluation
- • Pain management
- • Medication administration
Ongoing Care
- • Monitor supplement compliance
- • Educate on safe sun exposure
- • Dietary counseling
- • Bone density monitoring
Vitamin D Mnemonic: “BONES”
Bow legs (rickets)
Osteomalacia in adults
No sun exposure
Elevated alkaline phosphatase
Supplementation needed
Comparative Analysis of Vitamin Deficiencies
| Vitamin | Primary Function | Deficiency Disease | Key Symptoms | At-Risk Groups |
|---|---|---|---|---|
| Vitamin A | Vision, immune function | Xerophthalmia, night blindness | Night blindness, dry eyes, infections | Children, pregnant women |
| Vitamin B | Energy metabolism, nerve function | Beriberi, pellagra, anemia | Neuropathy, anemia, dermatitis | Alcoholics, elderly, vegans |
| Vitamin C | Collagen synthesis, antioxidant | Scurvy | Bleeding gums, poor wound healing | Elderly, smokers, limited diet |
| Vitamin D | Calcium homeostasis, bone health | Rickets, osteomalacia | Bone deformities, muscle weakness | Children, elderly, limited sun |
Nursing Implementation in Practice
Community Health Nursing
Screening Programs
- • Implement vitamin deficiency screening in high-risk populations
- • Develop culturally appropriate assessment tools
- • Coordinate with local health departments
- • Establish referral networks for treatment
Health Education
- • Develop community education programs
- • Create culturally sensitive materials
- • Conduct nutrition workshops
- • Collaborate with schools and community centers
Clinical Nursing Practice
Patient Assessment
- • Conduct comprehensive nutritional assessments
- • Recognize early signs of deficiency
- • Monitor laboratory values
- • Assess compliance with supplementation
Interdisciplinary Collaboration
- • Work with dietitians for meal planning
- • Collaborate with physicians for treatment protocols
- • Coordinate with social services for food access
- • Engage pharmacists for medication management
Evidence-Based Practice Guidelines
Assessment Standards
- • Use validated nutritional assessment tools
- • Follow evidence-based screening protocols
- • Document findings systematically
- • Monitor patient outcomes
Intervention Protocols
- • Implement standardized treatment plans
- • Use evidence-based dosing guidelines
- • Monitor for adverse effects
- • Adjust interventions based on response
Quality Improvement
- • Participate in quality improvement initiatives
- • Collect and analyze outcome data
- • Implement best practice changes
- • Engage in continuous education
Special Populations and Considerations
Pediatric Populations
Infants and Toddlers
- • Vitamin D deficiency risk in breastfed infants
- • Iron-deficiency anemia affects B vitamin status
- • Growth and development monitoring essential
- • Parental education crucial for prevention
School-Age Children
- • Vitamin A deficiency affects learning
- • B-complex deficiencies impact cognitive development
- • School nutrition programs important
- • Screen for eating disorders
Elderly Populations
Unique Risk Factors
- • Decreased absorption capacity
- • Medication interactions
- • Social isolation affecting nutrition
- • Chronic disease complications
Nursing Considerations
- • Assess for polypharmacy interactions
- • Monitor for cognitive changes
- • Evaluate fall risk from bone disease
- • Coordinate with family and caregivers
Pregnant and Lactating Women
Pregnancy Considerations
- • Folate deficiency increases neural tube defect risk
- • Vitamin D deficiency affects fetal bone development
- • Vitamin A excess can be teratogenic
- • Iron supplementation may affect other vitamins
Lactation Considerations
- • Maternal vitamin status affects breast milk composition
- • Vitamin B12 deficiency risk in vegan mothers
- • Vitamin D supplementation for both mother and infant
- • Monitor infant growth and development
Emergency Situations and Critical Care
Acute Presentations
Wernicke’s Encephalopathy (Thiamine Deficiency)
- • Classic triad: confusion, ataxia, ophthalmoplegia
- • Medical emergency requiring immediate thiamine
- • Give thiamine before glucose to prevent worsening
- • Monitor for Korsakoff’s psychosis development
Severe Vitamin D Deficiency
- • Hypocalcemic tetany and seizures
- • Laryngospasm and respiratory compromise
- • Cardiac arrhythmias possible
- • Immediate calcium and vitamin D replacement
Critical Care Considerations
Monitoring Parameters
- • Neurological status and mental state
- • Cardiovascular stability
- • Electrolyte balance
- • Respiratory function
Nursing Priorities
- • Airway protection and oxygenation
- • Hemodynamic monitoring
- • Seizure precautions
- • Medication administration and monitoring
Patient and Family Education
Educational Strategies
Teaching Methods
- • Use visual aids and demonstrations
- • Provide written materials in appropriate languages
- • Employ teach-back method for comprehension
- • Utilize technology and mobile apps
- • Incorporate cultural preferences
Key Educational Topics
- • Importance of vitamin-rich foods
- • Proper supplement usage
- • Recognition of deficiency symptoms
- • When to seek medical attention
- • Lifestyle modifications
Compliance Strategies
Enhancing Adherence
- • Simplify supplement regimens
- • Address cost and access barriers
- • Involve family and support systems
- • Provide regular follow-up
- • Celebrate small successes
Monitoring and Follow-up
- • Schedule regular reassessments
- • Monitor laboratory values
- • Track symptom improvement
- • Adjust interventions as needed
- • Provide ongoing support
Summary and Key Takeaways
Essential Nursing Competencies
Assessment Skills
- • Recognize early signs of vitamin deficiencies
- • Conduct comprehensive nutritional assessments
- • Interpret laboratory values appropriately
- • Assess risk factors in various populations
Intervention Skills
- • Implement evidence-based treatment protocols
- • Provide culturally sensitive patient education
- • Monitor treatment effectiveness
- • Coordinate interdisciplinary care
Clinical Pearls
Remember
- • Prevention is more cost-effective than treatment
- • Multiple deficiencies often coexist
- • Early intervention prevents irreversible damage
- • Patient education is crucial for long-term success
Always Consider
- • Underlying causes of deficiency
- • Drug-nutrient interactions
- • Special population needs
- • Socioeconomic factors affecting nutrition
Master Summary Mnemonic: “VITAL CARE”
Vitamin deficiencies are preventable
Identify at-risk populations
Teach patients about nutrition
Assess comprehensively
Collaborate with healthcare team
Administer supplements safely
Recognize emergency situations
Evaluate outcomes regularly
References and Further Reading
Professional Guidelines and Resources
- • World Health Organization. (2023). Vitamin and mineral deficiency: A global damage assessment report.
- • National Institute of Health. (2023). Dietary supplements: Health professional fact sheets.
- • American Nurses Association. (2023). Scope and standards of practice for nutrition nursing.
- • Academy of Nutrition and Dietetics. (2023). Evidence-based nutrition practice guidelines.
- • Centers for Disease Control and Prevention. (2023). Micronutrient deficiencies: Prevention and control.
