Mineral Deficiency Diseases
Comprehensive Nursing Notes on Iron, Iodine, and Calcium Deficiencies
Introduction to Mineral Deficiency Diseases
Mineral deficiency diseases represent a significant global health challenge affecting millions of people worldwide. These conditions arise when the body lacks essential minerals required for optimal physiological function, leading to a cascade of metabolic disruptions and clinical manifestations.
Key Learning Objectives
- Understand the pathophysiology of mineral deficiencies
- Identify clinical signs and symptoms
- Implement evidence-based nursing interventions
- Develop prevention strategies
- Apply knowledge in clinical practice
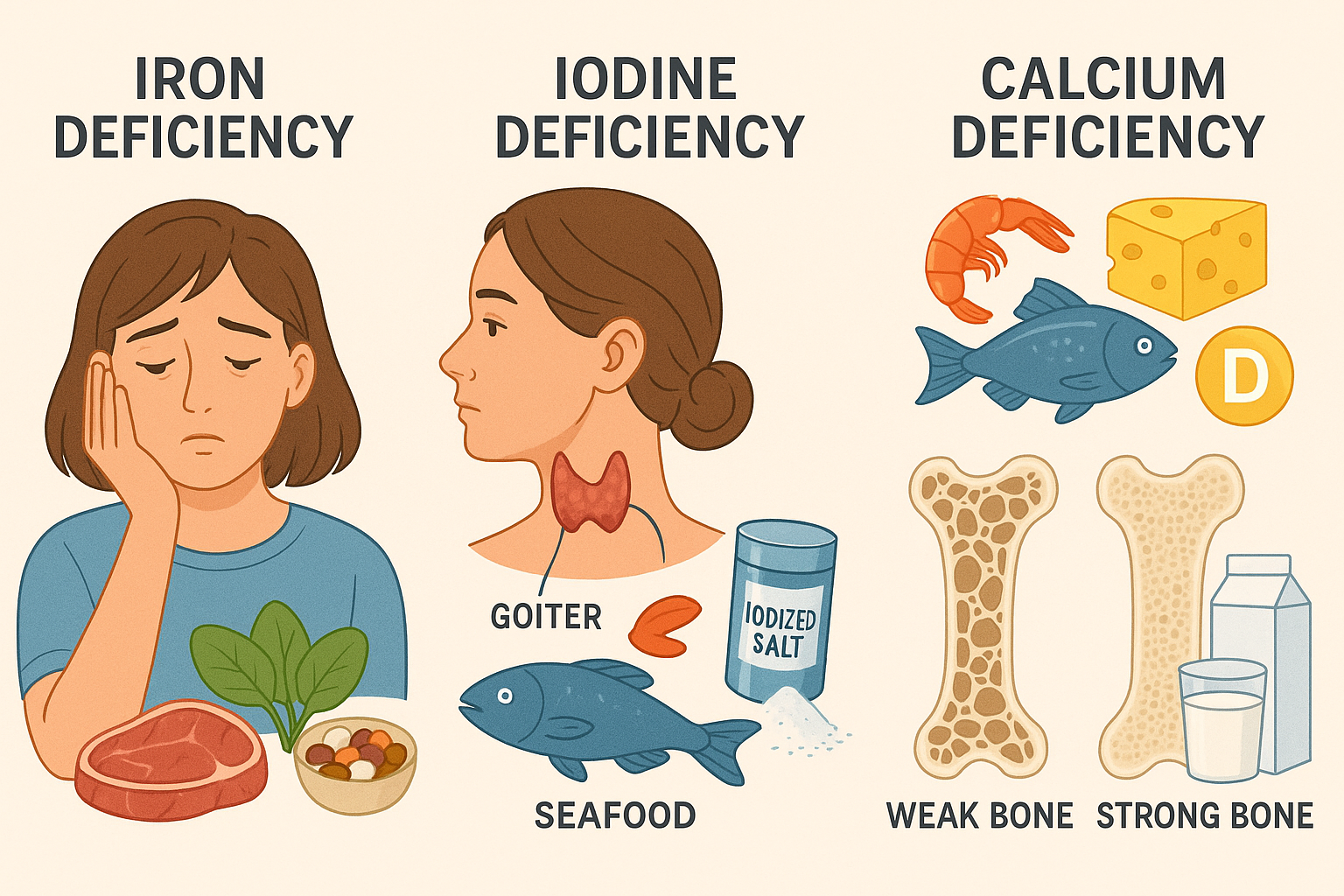
Visual overview of the three major mineral deficiency diseases covered in this study guide
Memory Aid – “ICE” Framework
Iron Deficiency Anemia
Pathophysiology
Iron deficiency anemia occurs when the body lacks sufficient iron to produce healthy red blood cells. Iron is essential for hemoglobin synthesis, which carries oxygen throughout the body. The condition develops in three stages:
- Iron Depletion: Reduced iron stores (low serum ferritin)
- Iron Deficient Erythropoiesis: Impaired red blood cell production
- Iron Deficiency Anemia: Reduced hemoglobin levels
Causes and Risk Factors
Blood Loss
- Gastrointestinal bleeding (ulcers, cancer)
- Heavy menstrual periods
- Frequent blood donation
- Trauma or surgery
- Chronic nosebleeds
Inadequate Intake/Absorption
- Poor dietary iron intake
- Vegetarian/vegan diets without supplementation
- Celiac disease
- Inflammatory bowel disease
- Pregnancy and breastfeeding
Signs and Symptoms
Cardiovascular
- • Fatigue and weakness
- • Palpitations
- • Shortness of breath
- • Chest pain
Physical Appearance
- • Pale skin, nails, inner eyelids
- • Brittle or spoon-shaped nails
- • Hair loss
- • Cold hands and feet
Neurological
- • Dizziness
- • Headaches
- • Difficulty concentrating
- • Restless leg syndrome
Unusual Cravings
- • Ice (pagophagia)
- • Starch
- • Dirt or cornstarch
- • Non-food items (pica)
Laboratory Findings
Decreased Values
- • Hemoglobin: <12 g/dL (women), <14 g/dL (men)
- • Hematocrit: <36% (women), <42% (men)
- • Serum ferritin: <15 ng/mL
- • Serum iron: <50 μg/dL
- • Transferrin saturation: <16%
Increased Values
- • Total iron-binding capacity (TIBC): >450 μg/dL
- • Transferrin: >360 mg/dL
- • Red cell distribution width (RDW): >14.5%
Management and Treatment
Pharmacological Treatment
Oral Iron Supplements
- • Ferrous sulfate: 325mg TID
- • Ferrous gluconate: 300mg TID
- • Ferrous fumarate: 200mg TID
- • Take on empty stomach with vitamin C
Parenteral Iron
- • Iron dextran (IV/IM)
- • Iron sucrose (IV only)
- • Reserved for severe cases
Dietary Interventions
Heme Iron Sources (Better Absorbed)
- • Red meat (beef, lamb)
- • Poultry (chicken, turkey)
- • Fish and shellfish
- • Organ meats (liver, kidney)
Non-Heme Iron Sources
- • Dark leafy greens (spinach, kale)
- • Legumes (lentils, chickpeas)
- • Fortified cereals
- • Dried fruits (raisins, apricots)
Nursing Interventions and Role
Assessment and Monitoring
- • Monitor vital signs, especially heart rate and blood pressure
- • Assess for signs of fatigue, weakness, and activity intolerance
- • Monitor laboratory values (Hgb, Hct, ferritin, iron studies)
- • Evaluate dietary intake and nutritional status
- • Assess for sources of blood loss
Medication Administration
- • Administer iron supplements as prescribed
- • Educate about taking iron on empty stomach with vitamin C
- • Monitor for side effects (constipation, nausea, dark stools)
- • Ensure proper IV iron administration techniques
- • Watch for allergic reactions with parenteral iron
Activity and Safety
- • Encourage gradual increase in activity as tolerated
- • Provide assistance with activities of daily living
- • Implement fall prevention measures
- • Plan rest periods between activities
- • Monitor for signs of cardiac decompensation
Patient Education
- • Teach about iron-rich foods and meal planning
- • Explain factors that enhance/inhibit iron absorption
- • Discuss importance of medication compliance
- • Educate about signs of improvement and complications
- • Provide resources for ongoing nutritional support
Prevention Strategies
Dietary Prevention
- • Consume iron-rich foods regularly
- • Combine vitamin C with iron-rich meals
- • Avoid tea/coffee with iron-rich foods
- • Use iron-fortified products
High-Risk Groups
- • Pregnant and lactating women
- • Infants and toddlers
- • Adolescents (growth spurts)
- • Women with heavy menstrual periods
Memory Aid: “TIRED” for Iron Deficiency Signs
Iodine Deficiency Disorders
Pathophysiology
Iodine is essential for thyroid hormone synthesis (T3 and T4). When iodine intake is insufficient, the thyroid gland enlarges (goiter) as it attempts to capture more iodine from the bloodstream. This leads to hypothyroidism and various metabolic disruptions.
Normal Process: Iodine → Thyroglobulin → T4 and T3 → Cellular metabolism
Deficiency Process: Low iodine → ↑TSH → Thyroid enlargement → ↓T4/T3 → Metabolic dysfunction
Causes and Risk Factors
Environmental Factors
- Geographic regions with iodine-poor soil
- Mountainous areas (Alps, Himalayas)
- Areas with frequent flooding
- Distance from ocean/seafood sources
- Volcanic soil regions
Dietary and Lifestyle
- Inadequate iodized salt consumption
- Vegan diets without iodine supplementation
- Excessive consumption of goitrogens
- Limited seafood intake
- Processed foods with non-iodized salt
Spectrum of Iodine Deficiency Disorders (IDD)
Pregnancy/Fetal
- • Miscarriage
- • Stillbirth
- • Congenital anomalies
- • Cretinism
Childhood
- • Goiter
- • Hypothyroidism
- • Impaired growth
- • Delayed development
Adult
- • Goiter
- • Hypothyroidism
- • Decreased fertility
- • Mental impairment
Signs and Symptoms
Metabolic
- • Weight gain
- • Cold intolerance
- • Decreased metabolism
- • Bradycardia
Neurological
- • Mental retardation (severe cases)
- • Decreased cognitive function
- • Poor concentration
- • Memory problems
Physical
- • Visible goiter (neck swelling)
- • Dry skin and hair
- • Muscle weakness
- • Edema
Developmental
- • Growth retardation
- • Delayed puberty
- • Reproductive problems
- • Hearing impairment
Diagnostic Tests
Laboratory Tests
- • TSH: Elevated (>4.0 mIU/L)
- • Free T4: Decreased (<0.8 ng/dL)
- • Free T3: Decreased (<2.3 pg/mL)
- • Urinary iodine: <100 μg/L
- • Thyroglobulin: Elevated
Imaging Studies
- • Thyroid ultrasound
- • Radioactive iodine uptake scan
- • CT/MRI for large goiters
- • Chest X-ray if respiratory symptoms
Management and Treatment
Medical Treatment
Iodine Supplementation
- • Potassium iodide (KI): 150-300 μg daily
- • Lugol’s iodine: 1-2 drops daily
- • Iodized oil: Single annual dose
Thyroid Hormone Replacement
- • Levothyroxine: 1.6 μg/kg/day
- • Monitor TSH levels
- • Adjust dose based on response
Surgical Intervention
- • Total/partial thyroidectomy
- • For large, obstructive goiters
- • Malignancy concerns
Dietary Interventions
Iodine-Rich Foods
- • Seaweed (kelp, nori)
- • Seafood (fish, shellfish)
- • Dairy products
- • Eggs
- • Iodized salt
Goitrogens to Limit
- • Cruciferous vegetables (raw)
- • Soy products
- • Cassava
- • Millet
Nursing Interventions and Role
Assessment and Monitoring
- • Assess for goiter size and respiratory compromise
- • Monitor vital signs, weight, and metabolic markers
- • Evaluate cognitive function and development
- • Check for signs of hypothyroidism
- • Monitor thyroid function tests
Airway Management
- • Position patient to optimize breathing
- • Monitor for signs of tracheal compression
- • Prepare for emergency airway management
- • Assess swallowing ability
- • Monitor oxygen saturation
Metabolic Support
- • Provide warm environment
- • Monitor for hypothermia
- • Assess for bradycardia
- • Monitor fluid balance
- • Encourage adequate rest
Community Health Education
- • Educate about iodine-rich foods
- • Promote use of iodized salt
- • Teach about medication compliance
- • Discuss importance of prenatal care
- • Provide resources for ongoing support
Prevention Strategies
Public Health Measures
- • Universal salt iodization programs
- • Iodine supplementation in endemic areas
- • Monitoring of population iodine status
- • Education campaigns
Individual Prevention
- • Use iodized salt in cooking
- • Include seafood in diet regularly
- • Prenatal iodine supplementation
- • Regular thyroid screening
Memory Aid: “GOITER” for Iodine Deficiency
Calcium Deficiency Disorders
Pathophysiology
Calcium deficiency affects bone mineralization, muscle function, and nerve transmission. The body maintains serum calcium levels by mobilizing calcium from bones, leading to weakened bone structure. This results in rickets in children and osteomalacia in adults.
Normal Process: Calcium intake → Vitamin D activation → Intestinal absorption → Bone mineralization
Deficiency Process: Low calcium → ↑PTH → Bone resorption → ↓Bone density → Fractures
Types of Calcium Deficiency Disorders
Rickets (Children)
- • Defective bone mineralization
- • Occurs during growth periods
- • Affects growth plates
- • Causes bone deformities
Osteomalacia (Adults)
- • Softening of existing bones
- • Occurs after growth completion
- • Affects mature bone tissue
- • Causes bone pain and weakness
Causes and Risk Factors
Nutritional Causes
- Inadequate dietary calcium intake
- Vitamin D deficiency
- Phosphate deficiency
- Magnesium deficiency
- Lactose intolerance
- Vegan diet without supplementation
Medical Conditions
- Malabsorption syndromes
- Chronic kidney disease
- Liver disease
- Hyperparathyroidism
- Certain medications (anticonvulsants)
- Limited sun exposure
Signs and Symptoms
Rickets in Children
Skeletal Deformities
- • Bowing of legs (genu varum/valgum)
- • Craniotabes (soft skull)
- • Delayed fontanelle closure
- • Pectus carinatum (pigeon chest)
- • Kyphoscoliosis
Growth and Development
- • Delayed tooth eruption
- • Dental caries
- • Short stature
- • Delayed walking
- • Muscle weakness
Osteomalacia in Adults
Bone and Joint
- • Persistent bone pain
- • Muscle weakness
- • Fractures with minimal trauma
- • Joint stiffness
- • Bone tenderness
Functional
- • Difficulty walking
- • Waddling gait
- • Climbing stairs difficulty
- • Muscle cramps
- • Fatigue
Diagnostic Tests
Laboratory Tests
- • Serum calcium: Low-normal
- • Serum phosphate: Low (<2.5 mg/dL)
- • Alkaline phosphatase: Elevated
- • 25(OH)D: Low (<20 ng/mL)
- • PTH: Elevated
- • 24-hour urine calcium: Low
Radiographic Findings
- • Pseudofractures (Looser zones)
- • Delayed ossification
- • Coarse trabecular pattern
- • Bone deformities
- • Osteopenia
Bone Studies
- • Bone density scan (DEXA)
- • Bone biopsy (if needed)
- • Quantitative CT scan
- • Ultrasound densitometry
Management and Treatment
Pharmacological Treatment
Calcium Supplementation
- • Calcium carbonate: 1000-1200 mg/day
- • Calcium citrate: Better absorption
- • Divide doses throughout day
- • Take with meals
Vitamin D Supplementation
- • Ergocalciferol (D2): 50,000 IU weekly
- • Cholecalciferol (D3): 1000-2000 IU daily
- • Calcitriol: 0.25-0.5 μg BID
- • Monitor 25(OH)D levels
Adjuvant Therapy
- • Phosphate supplementation
- • Magnesium supplementation
- • Bisphosphonates (if indicated)
Non-Pharmacological Treatment
Dietary Modifications
- • Dairy products (milk, yogurt, cheese)
- • Leafy green vegetables
- • Fortified foods
- • Canned fish with bones
- • Almonds and sesame seeds
Lifestyle Modifications
- • Regular sun exposure
- • Weight-bearing exercises
- • Physical therapy
- • Fall prevention measures
Surgical Treatment
- • Corrective osteotomy
- • Fracture fixation
- • Joint replacement
- • Spinal fusion (if needed)
Nursing Interventions and Role
Assessment and Monitoring
- • Assess for bone pain, muscle weakness, and fractures
- • Monitor growth and development in children
- • Evaluate gait and mobility
- • Check for signs of tetany and muscle spasms
- • Monitor laboratory values (calcium, phosphate, vitamin D)
Safety and Fall Prevention
- • Implement fall prevention strategies
- • Ensure safe environment (remove hazards)
- • Provide assistive devices as needed
- • Educate about fracture risk
- • Monitor for signs of pathological fractures
Mobility and Rehabilitation
- • Encourage weight-bearing activities
- • Assist with range of motion exercises
- • Coordinate with physical therapy
- • Provide pain management strategies
- • Monitor exercise tolerance
Patient and Family Education
- • Teach about calcium-rich foods
- • Explain importance of vitamin D
- • Discuss medication compliance
- • Educate about sun exposure benefits
- • Provide resources for ongoing nutrition support
Prevention Strategies
Pediatric Prevention
- • Adequate calcium intake during growth
- • Vitamin D supplementation
- • Promote outdoor activities
- • Regular growth monitoring
- • Nutritional counseling
Adult Prevention
- • Maintain adequate calcium intake
- • Regular bone density screening
- • Weight-bearing exercise
- • Limit risk factors (smoking, alcohol)
- • Hormone replacement therapy (if indicated)
Memory Aid: “BONES” for Calcium Deficiency
Clinical Application and Case Studies
Iron Deficiency Case
Patient: 28-year-old female, heavy menstrual periods, fatigue, pale conjunctiva
Labs: Hgb 8.2 g/dL, Ferritin 8 ng/mL, TIBC elevated
Nursing Priority: Activity intolerance, knowledge deficit, medication compliance
Iodine Deficiency Case
Patient: 45-year-old male, visible goiter, cold intolerance, weight gain
Labs: TSH 12.5 mIU/L, Free T4 0.6 ng/dL, Low urinary iodine
Nursing Priority: Airway assessment, metabolic support, education
Calcium Deficiency Case
Patient: 65-year-old female, hip fracture, bone pain, limited mobility
Labs: Low 25(OH)D, elevated PTH, low phosphate
Nursing Priority: Fall prevention, pain management, rehabilitation
Priority Nursing Diagnoses
Iron Deficiency Anemia
Primary Nursing Diagnoses
- • Activity intolerance related to decreased oxygen-carrying capacity
- • Fatigue related to decreased hemoglobin levels
- • Imbalanced nutrition: less than body requirements
- • Deficient knowledge regarding iron therapy
Expected Outcomes
- • Patient will demonstrate improved activity tolerance
- • Hemoglobin levels will increase to normal range
- • Patient will verbalize understanding of iron therapy
- • Patient will maintain adequate nutritional intake
Iodine Deficiency
Primary Nursing Diagnoses
- • Ineffective airway clearance related to goiter compression
- • Disturbed body image related to visible goiter
- • Hypothermia related to decreased metabolic rate
- • Deficient knowledge regarding iodine supplementation
Expected Outcomes
- • Patient will maintain patent airway
- • Thyroid function tests will normalize
- • Patient will demonstrate understanding of treatment
- • Patient will maintain normal body temperature
Calcium Deficiency
Primary Nursing Diagnoses
- • Risk for injury related to bone fragility
- • Chronic pain related to bone demineralization
- • Impaired physical mobility related to bone weakness
- • Deficient knowledge regarding calcium supplementation
Expected Outcomes
- • Patient will remain free from fractures
- • Pain levels will decrease to manageable levels
- • Patient will demonstrate improved mobility
- • Calcium and vitamin D levels will normalize
Key Takeaways for Nursing Practice
Critical Concepts
- • Early Recognition: Identify at-risk populations and subtle symptoms
- • Holistic Assessment: Consider nutritional, cultural, and socioeconomic factors
- • Patient Safety: Prioritize fall prevention and airway management
- • Education Focus: Emphasize prevention through nutrition and lifestyle
- • Interdisciplinary Care: Collaborate with dietitians, physicians, and social workers
Quality Indicators
- • Medication Compliance: Monitor adherence to supplementation regimens
- • Laboratory Monitoring: Track improvement in relevant biomarkers
- • Functional Status: Assess improvements in activities of daily living
- • Patient Satisfaction: Evaluate understanding and comfort with treatment
- • Complication Prevention: Minimize adverse effects and complications
References and Further Reading
1. World Health Organization. (2024). Iron deficiency anemia: Assessment, prevention and control. WHO Press.
2. American Thyroid Association. (2024). Iodine deficiency disorders: Clinical practice guidelines. Thyroid Journal.
3. Institute of Medicine. (2024). Dietary reference intakes for calcium and vitamin D. National Academies Press.
4. Nurseslabs. (2024). Iron deficiency anemia nursing care management. Retrieved from https://nurseslabs.com/iron-deficiency-anemia/
5. Cleveland Clinic. (2024). Iodine deficiency: Symptoms, causes & treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/23417-iodine-deficiency
6. National Institutes of Health. (2024). Calcium fact sheet for health professionals. Retrieved from https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
7. Medscape. (2024). Iodine deficiency treatment & management. Retrieved from https://emedicine.medscape.com/article/122714-treatment
8. NCBI. (2024). Osteomalacia: Pathophysiology and clinical management. StatPearls Publishing.
