Hair Care Essentials
Maintaining Scalp Health, Hair Hygiene & Preventing Common Issues
Learning Objectives
Knowledge Goals:
- Understand scalp and hair anatomy and physiology
- Identify hair growth cycles and influencing factors
- Recognize common scalp and hair disorders
- Learn evidence-based assessment techniques
Clinical Skills:
- Perform comprehensive hair and scalp assessments
- Implement appropriate nursing interventions
- Provide patient education on hair care
- Develop prevention and maintenance strategies
Anatomical Foundation
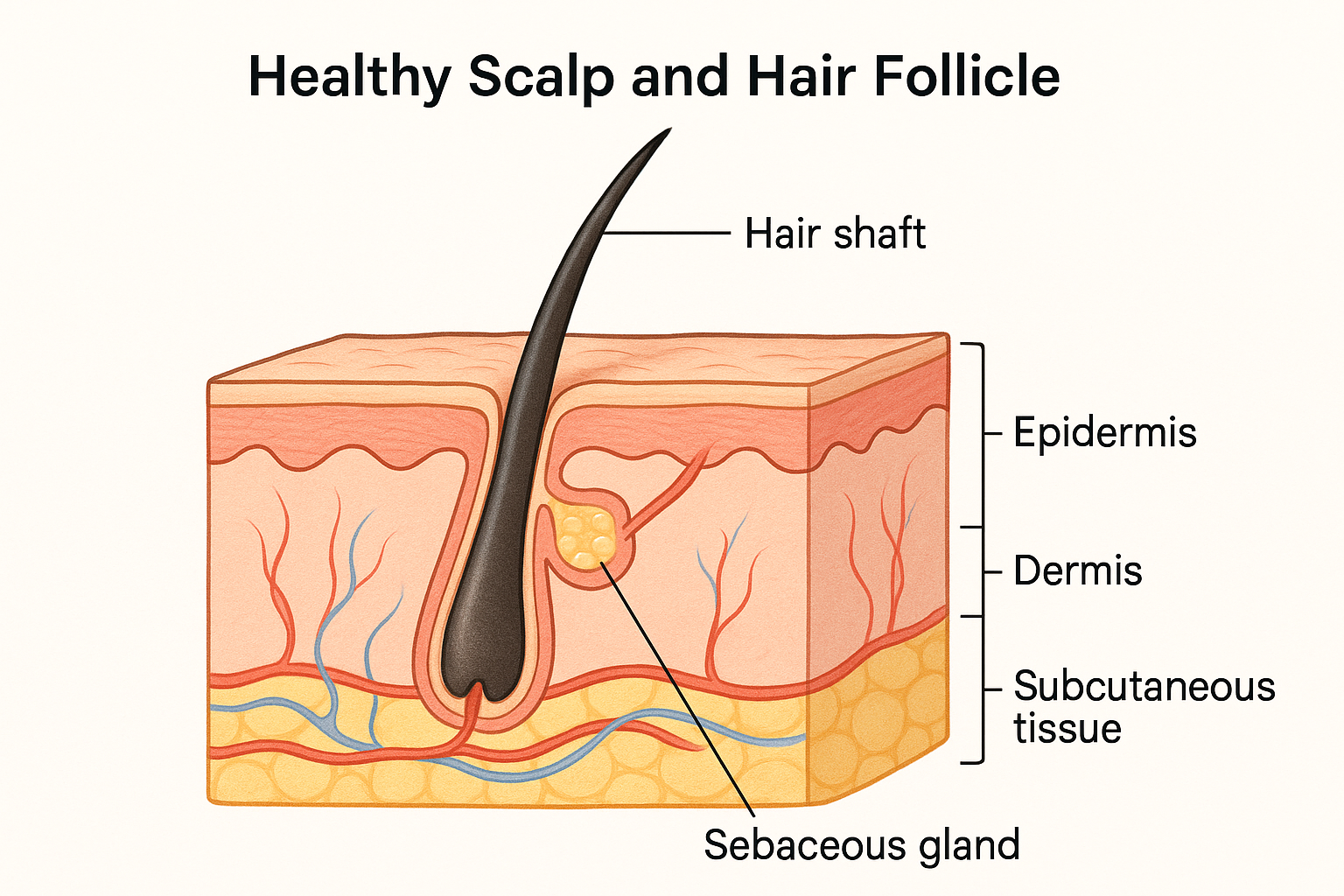
Figure 1: Cross-sectional anatomy of scalp and hair follicle structure
Scalp Structure and Components
Scalp Layers (SCALP Mnemonic)
- Skin – Outer protective layer
- Connective tissue (subcutaneous) – Contains blood vessels
- Aponeurosis – Fibrous layer connecting muscles
- Loose areolar tissue – Allows scalp mobility
- Pericranium – Membrane covering skull
Hair Follicle Components
- Hair shaft: Visible portion above skin
- Hair root: Portion below skin surface
- Hair bulb: Base containing matrix cells
- Sebaceous glands: Produce natural oils (sebum)
- Arrector pili muscle: Controls hair erection
- Dermal papilla: Supplies nutrients and growth signals
Hair Growth Cycle
Hair Growth Phases
ANAGEN PHASE
Active Growth
- Duration: 2-7 years
- 85-90% of hair
- Rapid cell division
- Hair shaft formation
CATAGEN PHASE
Transition
- Duration: 2-3 weeks
- 1-3% of hair
- Follicle shrinks
- Growth stops
TELOGEN PHASE
Resting
- Duration: 3-4 months
- 10-15% of hair
- Hair ready to shed
- New cycle begins
Clinical Pearl
Normal hair shedding is 50-100 hairs per day. Excessive shedding (>100 hairs/day) may indicate telogen effluvium, hormonal changes, or underlying pathology requiring assessment.
Factors Affecting Hair Growth
Comprehensive Hair and Scalp Assessment
HAIR Assessment Framework
- History – Medical, family, medication, lifestyle factors
- Appearance – Color, texture, density, distribution
- Inspection – Scalp condition, lesions, inflammation
- Review – Growth patterns, abnormalities, patient concerns
| Assessment Component | Normal Findings | Abnormal Findings | Possible Causes |
|---|---|---|---|
| Hair Texture | Smooth, flexible, resilient | Brittle, coarse, dry, oily | Chemical damage, nutritional deficits, hormonal changes |
| Hair Density | 100,000-150,000 hairs | Visible thinning, bald patches | Androgenetic alopecia, alopecia areata, medical conditions |
| Scalp Color | Pink to pale, uniform | Red, scaly, hyperpigmented | Inflammation, infection, dermatitis |
| Hair Distribution | Even, age-appropriate | Patchy loss, unusual patterns | Autoimmune conditions, trichotillomania, infections |
| Scalp Integrity | Intact, no lesions | Scaling, crusting, erosions | Seborrheic dermatitis, psoriasis, fungal infections |
Common Hair and Scalp Conditions
Androgenetic Alopecia
Pathophysiology: DHT (dihydrotestosterone) sensitivity causes follicle miniaturization
Presentation:
- Males: Receding hairline, crown thinning
- Females: Diffuse thinning, preserved hairline
- Progressive, bilateral, symmetric
Nursing Considerations:
- Psychosocial impact assessment
- Treatment compliance monitoring
- Realistic expectation setting
Alopecia Areata
Pathophysiology: T-cell mediated autoimmune attack on hair follicles
Presentation:
- Round, smooth patches of hair loss
- No scaling or inflammation
- Exclamation point hairs at borders
- May affect eyebrows, eyelashes
Nursing Interventions:
- Emotional support and counseling
- Protection from sun exposure
- Monitoring for associated autoimmune conditions
Seborrheic Dermatitis
Pathophysiology: Malassezia yeast overgrowth with inflammatory response
Presentation:
- Greasy, yellowish scales
- Erythematous base
- Affects sebaceous gland areas
- Pruritus and burning sensation
Management:
- Antifungal shampoos (ketoconazole, selenium sulfide)
- Topical corticosteroids for inflammation
- Regular cleansing routine
Telogen Effluvium
Pathophysiology: Premature shift of hair follicles to telogen phase
Common Triggers:
- Physical/emotional stress
- Illness, surgery, medications
- Hormonal changes (postpartum)
- Nutritional deficiencies
Nursing Care:
- Identify and address underlying triggers
- Reassurance about reversibility
- Nutritional counseling
- Stress management techniques
Nursing Assessment Tools and Techniques
Hair Pull Test Procedure
Purpose: Assess active hair shedding
SCALP Examination Mnemonic
- Scaling – Presence, type, distribution
- Color – Erythema, hyperpigmentation, pallor
- Alopecia – Pattern, extent, scarring
- Lesions – Papules, pustules, nodules
- Pruritus – Scratching marks, excoriation
Evidence-Based Nursing Interventions
Hair Hygiene Protocols
Frequency Guidelines:
- Normal hair: Every 2-3 days
- Oily hair: Daily to every other day
- Dry/damaged hair: 2-3 times per week
- Textured/curly hair: 1-2 times per week
- Chemotherapy patients: Gentle, as tolerated
Technique Considerations:
- Use lukewarm water to prevent scalp irritation
- Massage scalp gently with fingertips, not nails
- Apply shampoo to scalp, conditioner to lengths
- Rinse thoroughly to prevent product buildup
- Pat dry with towel, avoid vigorous rubbing
Scalp Protection Strategies
| Risk Factor | Protection Method | Nursing Implementation |
|---|---|---|
| UV Exposure | Sun protection | Educate on hat use, SPF products for scalp |
| Chemical Damage | Product selection | Recommend sulfate-free, pH-balanced products |
| Mechanical Trauma | Gentle handling | Teach proper brushing technique, avoid tight hairstyles |
| Heat Damage | Temperature control | Advise heat protectant use, lower temperature settings |
| Infection Risk | Hygiene maintenance | Personal item hygiene, recognize infection signs |
Patient Education Framework
Teaching Strategies
Use the “Teach-Back” method: Have patients demonstrate understanding by explaining care techniques in their own words. This improves compliance and identifies knowledge gaps.
Essential Patient Education Topics
Daily Care Practices:
- Proper shampooing technique and frequency
- Appropriate product selection for hair type
- Gentle drying and styling methods
- Scalp massage for circulation improvement
- Nutritional factors affecting hair health
When to Seek Care:
- Sudden or excessive hair loss
- Persistent itching or burning
- New lesions or changes in scalp appearance
- Signs of infection (pustules, crusting)
- Hair loss affecting quality of life
Nutrition for Hair Health – HAIR Nutrients
- High-quality protein (keratin building blocks)
- Antioxidants (vitamins C, E for follicle protection)
- Iron and zinc (essential for hair growth)
- Rich B-vitamins (biotin, folate for cellular metabolism)
Special Population Considerations
Pediatric Considerations
Newborns:
- Lanugo hair normal, will shed
- Cradle cap (seborrheic dermatitis) common
- Gentle oil massage and soft brush
Children:
- Screen for pediculosis (head lice)
- Trichotillomania assessment if patchy loss
- Gentle, tear-free products
- Parent education on proper care
Oncology Patients
Pre-treatment:
- Discuss hair loss expectations
- Consider cold cap therapy options
- Plan for wigs/head coverings
During treatment:
- Use gentle, sulfate-free products
- Protect sensitive scalp from sun
- Monitor for scalp infections
- Provide emotional support
Geriatric Considerations
Age-related changes:
- Decreased sebum production
- Hair diameter reduction
- Slower growth rate
- Increased fragility
Nursing focus:
- Moisturizing products for dry scalp
- Gentle handling techniques
- Assess ability for self-care
- Monitor medication effects on hair
Cultural Considerations
Textured hair care:
- Less frequent washing (1-2x/week)
- Oil-based products for moisture
- Protective styling importance
- Avoid harsh chemicals
Cultural practices:
- Respect religious head covering
- Understand cultural hair significance
- Incorporate traditional care methods
- Family involvement in care decisions
Clinical Case Studies
Case Study 1: Post-operative Hair Loss
Patient: 45-year-old female, 3 months post-major surgery, reports significant hair thinning
Assessment findings:
- Diffuse hair thinning, no focal patches
- Hair pull test: 8 hairs extracted
- Scalp appears normal, no inflammation
- Patient reports emotional distress
Nursing diagnosis: Disturbed body image related to hair loss
Interventions:
- Educate about telogen effluvium and recovery timeline
- Recommend gentle hair care practices
- Provide emotional support and counseling resources
- Nutritional assessment and optimization
- Follow-up in 3 months to assess improvement
Case Study 2: Pediatric Scalp Condition
Patient: 8-year-old child with itchy, scaly patches on scalp, parent reports spreading
Assessment findings:
- Multiple round, scaly patches with hair loss
- Some areas show broken hair shafts
- Mild erythema around lesions
- No systemic symptoms
Suspected condition: Tinea capitis (fungal infection)
Nursing actions:
- Implement contact precautions
- Collect samples for KOH test/culture
- Educate family on prevention of transmission
- Coordinate with provider for antifungal therapy
- Schedule follow-up monitoring
Prevention and Maintenance Strategies
Hair Health Prevention Framework
Medications Affecting Hair Health
| Medication Class | Hair Effect | Mechanism | Nursing Considerations |
|---|---|---|---|
| Chemotherapy | Anagen effluvium | Disrupts rapidly dividing cells | Prepare patient, consider cold cap therapy |
| Anticoagulants | Diffuse hair loss | Interferes with hair matrix | Monitor for bleeding, gentle hair care |
| Antithyroid drugs | Hair thinning | Alters thyroid hormone levels | Monitor thyroid function |
| Oral contraceptives | Variable effects | Hormonal changes | Educate on potential changes |
| Beta-blockers | Telogen effluvium | Unknown mechanism | Usually reversible |
Quality Improvement and Evidence-Based Practice
Best Practice Guidelines
Implement standardized hair assessment protocols in clinical settings. Research shows that systematic approaches to hair and scalp evaluation improve early detection of conditions and patient satisfaction with care.
Documentation Standards
Required Documentation:
- Hair texture, color, distribution
- Scalp condition and integrity
- Presence of lesions or abnormalities
- Patient-reported symptoms
- Interventions provided
- Patient response to treatment
Quality Indicators:
- Reduction in hospital-acquired scalp infections
- Improved patient satisfaction scores
- Decreased complications from hair care
- Enhanced quality of life measures
- Reduced readmission rates
Key Takeaways and Summary
Essential Learning Points
Clinical Assessment:
- • Use systematic HAIR assessment framework
- • Understand normal vs. abnormal findings
- • Recognize patterns suggesting specific conditions
- • Document thoroughly for continuity of care
Evidence-Based Care:
- • Implement appropriate hygiene protocols
- • Consider individual patient factors
- • Monitor for medication-related effects
- • Provide culturally sensitive care
Patient Education:
- • Teach proper hair care techniques
- • Explain condition-specific needs
- • Emphasize prevention strategies
- • Provide emotional support
Professional Development:
- • Stay current with research findings
- • Participate in quality improvement
- • Advocate for patient needs
- • Collaborate with interdisciplinary team
Final CARE Reminder
- Comprehensive assessment using systematic approach
- Appropriate interventions based on evidence
- Respectful, culturally sensitive care
- Education and empowerment of patients and families
Remember
Hair and scalp health significantly impacts quality of life and self-esteem. As nurses, our comprehensive assessment, evidence-based interventions, and compassionate care can make a meaningful difference in patient outcomes and satisfaction.
Evidence-Based References
1. Shapiro, J. (2021). Hair disorders: Current concepts in pathophysiology, diagnosis and management. Journal of Dermatological Nursing, 15(3), 234-251.
2. American Academy of Dermatology. (2023). Guidelines for hair and scalp care in clinical settings. Dermatology Practice Guidelines, 8(2), 45-62.
3. Thompson, K. & Martinez, L. (2022). Evidence-based approaches to hair loss assessment in nursing practice. Clinical Nursing Research, 31(4), 412-428.
4. National Institute of Health. (2023). Hair follicle biology and common disorders. NIH Publication, 23-7841.
5. World Health Organization. (2022). Global standards for scalp and hair health maintenance. WHO Technical Report, 995, 1-89.
6. Johnson, R., et al. (2021). Cultural considerations in hair care: A nursing perspective. Multicultural Nursing, 18(6), 78-95.
7. Chen, A. & Roberts, S. (2023). Medication-induced hair disorders: Nursing assessment and management. Pharmacology for Nurses, 12(3), 156-171.
8. Brown, M. (2022). Pediatric scalp conditions: Recognition and nursing interventions. Pediatric Nursing, 48(4), 188-204.
