Administration of Medications in Nursing
Master the Art of Safe Medication Administration: Understanding Definitions, Effects, Forms & Pharmacokinetics
Table of Contents
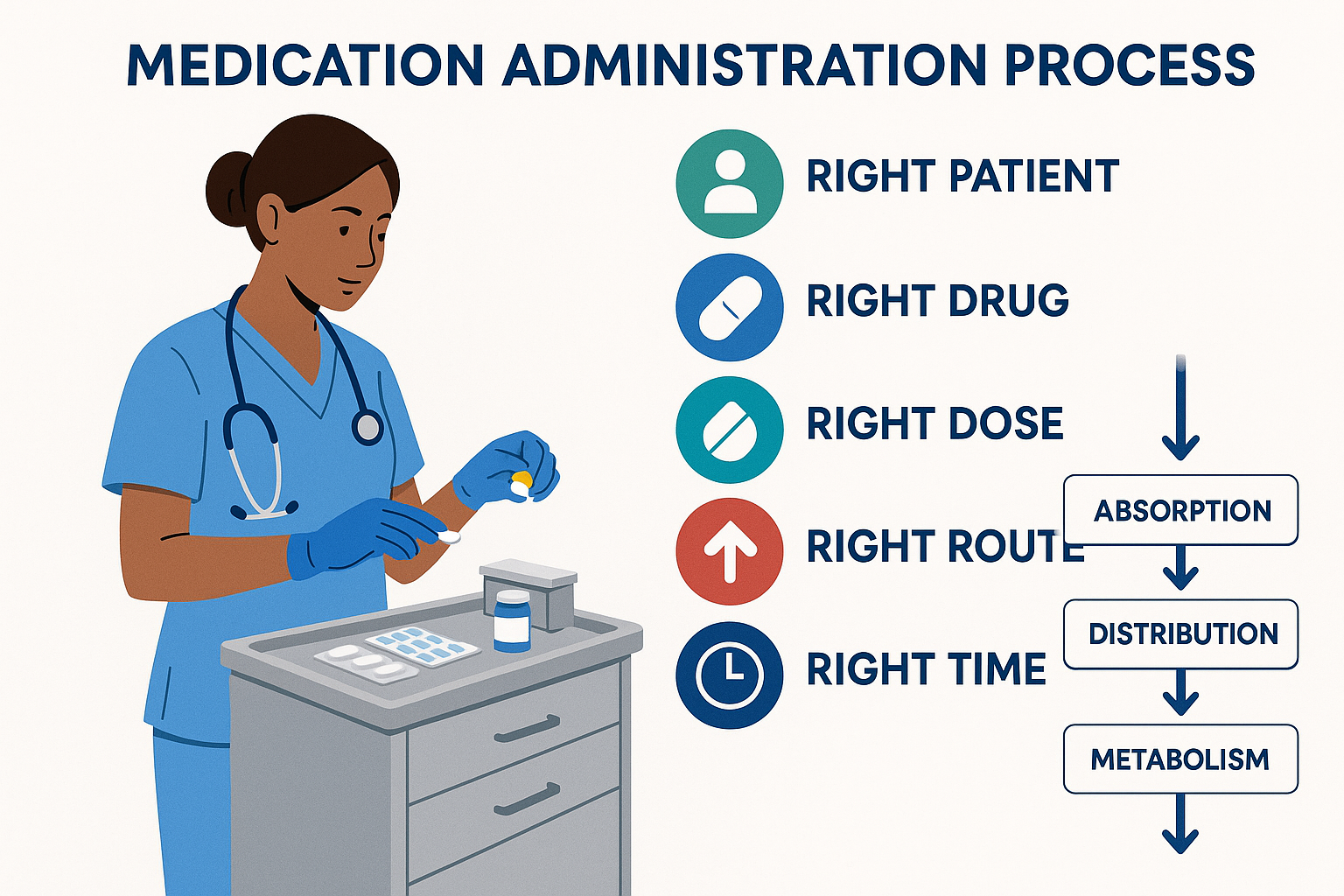
Medication Administration Process Overview
Introduction to Medication Administration
Welcome to the Foundation of Nursing Practice
Medication administration represents one of the most critical responsibilities in nursing practice. Understanding the complex interplay between drug properties, patient physiology, and therapeutic outcomes through pharmacokinetics principles is essential for safe and effective patient care.
Learning Objectives
- Master drug nomenclature and classification systems
- Understand various medication forms and their applications
- Comprehend pharmacokinetics and pharmacodynamics
- Implement safe medication administration practices
Safety First Mindset
Every medication administration decision must prioritize patient safety. The principles of pharmacokinetics guide us in understanding how drugs move through the body, ensuring optimal therapeutic outcomes while minimizing adverse effects.
Drug Nomenclature & Classification
Chemical Name
Describes the exact molecular structure and composition of the drug compound.
Example: N-acetyl-para-aminophenol (Acetaminophen)
Generic Name
Official non-proprietary name assigned by regulatory authorities.
Example: Acetaminophen (USA), Paracetamol (International)
Brand Name
Proprietary name given by the pharmaceutical manufacturer.
Example: Tylenol, Panadol, Calpol
Memory Aid: Drug Name Types
Chemical = Complex molecular structure
Generic = Government approved official name
Brand = Business marketing name
| Classification System | Basis | Example | Nursing Relevance |
|---|---|---|---|
| Therapeutic | Clinical use/indication | Antibiotics, Analgesics | Helps understand treatment goals |
| Pharmacological | Mechanism of action | Beta-blockers, ACE inhibitors | Predicts drug interactions |
| Chemical | Molecular structure | Penicillins, Sulfonamides | Identifies allergy patterns |
| Legal | Regulatory control | Controlled substances | Determines handling requirements |
Forms of Medications
Understanding medication forms is crucial for proper administration and affects pharmacokinetics significantly. Different formulations influence absorption rates, bioavailability, and therapeutic outcomes.
Solid Dosage Forms
Tablets
Compressed powder; convenient, stable, accurate dosing
Capsules
Encapsulated powder/liquid; masks taste, easier swallowing
Granules
Small particles; pediatric-friendly, adjustable doses
Powders
Dry form; reconstitution required, bulk compounding
Liquid Dosage Forms
Solutions
Homogeneous mixtures; rapid absorption, easy dosing
Suspensions
Particles in liquid; shake before use, controlled release
Emulsions
Oil-water mixtures; improved palatability, absorption
Syrups
Sweet solutions; pediatric use, cough preparations
Specialized Forms
Injectables
Sterile solutions for parenteral use
Topical
Creams, ointments, patches
Inhalants
Aerosols, dry powder inhalers
Drug Effects & Actions
Critical Understanding
Drug effects are the measurable changes that occur in the body after medication administration. These effects are directly influenced by pharmacokinetics processes and determine therapeutic success or failure.
Therapeutic Effects
-
Primary Effect: Intended therapeutic action
-
Secondary Effect: Additional beneficial actions
-
Prophylactic Effect: Disease prevention
-
Palliative Effect: Symptom management
Adverse Effects
-
Side Effects: Predictable unwanted effects
-
Toxic Effects: Dose-related harmful effects
-
Allergic Reactions: Immune system responses
-
Idiosyncratic: Unusual individual responses
Memory Aid: Drug Effect Types
TSPA for Therapeutic Effects:
Therapeutic (primary)
Secondary (additional benefits)
Prophylactic (prevention)
Adverse (harmful)
Pharmacokinetics: The Journey of Drugs
Understanding Pharmacokinetics
Pharmacokinetics is the study of how the body handles drugs – what the body does to the drug. This fundamental concept encompasses four key processes that determine drug effectiveness and safety in clinical practice.
Absorption
Drug movement from administration site into systemic circulation
Distribution
Drug transport throughout body tissues and organs
Metabolism
Chemical transformation of drugs, primarily in liver
Excretion
Elimination of drugs and metabolites from body
| Pharmacokinetic Phase | Primary Location | Factors Affecting Process | Nursing Considerations |
|---|---|---|---|
| Absorption | GI tract, muscle, subcutaneous tissue | pH, blood flow, surface area, food | Timing with meals, route selection |
| Distribution | Bloodstream, tissues, organs | Protein binding, tissue perfusion | Monitor for drug interactions |
| Metabolism | Liver (primarily), kidneys, lungs | Enzyme activity, genetic factors | Assess liver function, drug history |
| Excretion | Kidneys, lungs, bile, sweat | Renal function, urine pH | Monitor kidney function, hydration |
Memory Aid: Pharmacokinetics Process
ADME – The Four Pillars of Pharmacokinetics:
Absorption – Drug enters the body
Distribution – Drug spreads throughout body
Metabolism – Drug is chemically changed
Excretion – Drug leaves the body
Key Pharmacokinetic Parameters
Time-Related Parameters
- Half-life (t½): Time for drug concentration to reduce by half
- Onset of action: Time until therapeutic effect begins
- Duration of action: Length of therapeutic effect
- Peak time: Time to reach maximum concentration
Concentration-Related Parameters
- Bioavailability: Fraction of drug reaching systemic circulation
- Clearance: Rate of drug elimination from body
- Volume of distribution: Apparent space drug occupies
- Steady state: Equilibrium between input and elimination
Pharmacodynamics: How Drugs Work
While pharmacokinetics explains what the body does to the drug, pharmacodynamics describes what the drug does to the body. This relationship determines therapeutic outcomes and guides dosing decisions.
Mechanisms of Action
Receptor Binding
Drugs bind to specific cellular receptors to produce effects
Enzyme Inhibition
Drugs block specific enzymes to alter biochemical processes
Ion Channel Modulation
Drugs affect ion movement across cell membranes
Gene Expression
Drugs influence protein synthesis and cellular function
Dose-Response Relationships
Therapeutic Window
Range between minimum effective dose and toxic dose
ED50 (Effective Dose 50%)
Dose producing therapeutic effect in 50% of population
LD50 (Lethal Dose 50%)
Dose causing death in 50% of test subjects
Therapeutic Index
Ratio of toxic dose to therapeutic dose (LD50/ED50)
Drug Interactions and Pharmacodynamics
Synergism
Combined effect greater than sum of individual effects
Antagonism
One drug reduces or blocks another’s effect
Additive
Combined effect equals sum of individual effects
Purposes of Medication
Understanding medication purposes helps nurses make informed decisions about timing, monitoring, and patient education. Each purpose requires different considerations regarding pharmacokinetics and expected outcomes.
Preventive (Prophylactic)
Administered to prevent disease or complications before they occur.
Therapeutic (Curative)
Designed to treat existing conditions and restore health.
Palliative (Symptomatic)
Provides relief from symptoms without curing the underlying condition.
Diagnostic
Used to help diagnose medical conditions through testing or imaging.
Replacement
Replaces substances that the body cannot produce adequately.
Supportive
Maintains body functions during illness or treatment.
Safe Medication Practices
Patient Safety Priority
Safe medication administration requires understanding of pharmacokinetics, careful adherence to protocols, and continuous vigilance. Every step must prioritize patient safety and therapeutic effectiveness.
The 5 Rights of Medication Administration
Right Patient
Verify identity using two identifiers
Right Drug
Check medication name and strength
Right Dose
Calculate and verify dosage accuracy
Right Route
Confirm appropriate administration method
Right Time
Administer at scheduled intervals
Extended Rights (5 + 5)
Right Documentation
Complete accurate medication records
Right Reason
Understand indication for medication
Right Response
Monitor for therapeutic effects
Right to Refuse
Respect patient autonomy
Right Education
Provide patient teaching
Memory Aid: The 5 Rights
PDDRT – Never Forget These Rights:
Patient (verify identity)
Drug (check medication)
Dose (calculate accurately)
Route (confirm method)
Time (administer correctly)
Routes of Administration
The route of administration significantly affects pharmacokinetics parameters including absorption rate, bioavailability, and onset of action. Understanding these differences is crucial for optimal therapeutic outcomes.
Enteral Routes
Oral (PO)
Most common, convenient, but variable absorption
Sublingual (SL)
Under tongue; rapid absorption, bypasses liver
Buccal
Against cheek; sustained release, local effect
Rectal (PR)
Alternative when oral route unavailable
Parenteral Routes
Intravenous (IV)
Direct into bloodstream; immediate effect
Intramuscular (IM)
Into muscle tissue; faster than oral
Subcutaneous (SC)
Under skin; slower absorption, sustained effect
Intradermal (ID)
Into skin; mainly for testing
| Route | Onset Time | Bioavailability | Duration | Nursing Considerations |
|---|---|---|---|---|
| Intravenous | Immediate | 100% | Short | Requires sterile technique, monitor for infiltration |
| Intramuscular | 10-30 minutes | Variable | Moderate | Choose appropriate site, rotate injection sites |
| Subcutaneous | 30-60 minutes | Variable | Long | Rotate sites, assess for lipodystrophy |
| Oral | 30-60 minutes | Variable | Variable | Consider food interactions, swallowing ability |
| Sublingual | 1-3 minutes | High | Short | Avoid eating/drinking, hold under tongue |
Global Best Practices in Medication Administration
Healthcare systems worldwide have developed innovative approaches to medication safety, incorporating advanced understanding of pharmacokinetics and technology to improve patient outcomes.
Canada: Safer Healthcare Now!
High-Alert Medication Protocol: National standardization of high-risk drug handling with mandatory double-checks and specialized training.
Pharmacokinetic Monitoring: Integration of therapeutic drug monitoring with electronic health records for personalized dosing.
Key Innovation: Real-time clinical decision support systems that alert nurses to potential adverse effects based on patient-specific pharmacokinetics.
Netherlands: Medication Safety Program
Integrated Pharmacy Services: Clinical pharmacists embedded in nursing units to provide real-time consultation on complex medication regimens.
Smart Pump Technology: IV pumps with built-in safety limits and automatic dosing adjustments based on patient weight and renal function.
Key Innovation: Automated medication reconciliation systems that track changes in patient condition and adjust dosing recommendations.
Japan: Precision Medicine Initiative
Pharmacogenomics Integration: Genetic testing to predict individual patient responses to medications, optimizing both efficacy and safety.
Robotic Dispensing Systems: Automated medication preparation with barcode verification and real-time inventory management.
Key Innovation: AI-powered prediction models that anticipate adverse drug reactions based on patient demographics and medication history.
United Kingdom: NHS Safety Framework
National Reporting System: Comprehensive medication error reporting with analysis and feedback to improve system-wide safety.
Competency-Based Training: Structured nursing education programs with mandatory certification for medication administration.
Key Innovation: Mobile applications that provide instant access to drug information, interaction checkers, and dosing calculators.
Universal Best Practices
Technology Integration
- Electronic medication administration records (eMAR)
- Barcode scanning for drug verification
- Clinical decision support systems
- Automated dispensing systems
Education and Training
- Simulation-based learning programs
- Continuing education requirements
- Interprofessional collaboration training
- Patient safety culture development
Mastering Medication Administration
Safe and effective medication administration requires comprehensive understanding of drug properties, pharmacokinetics, and patient-centered care principles. By integrating theoretical knowledge with practical skills and adopting global best practices, nurses can ensure optimal therapeutic outcomes while maintaining the highest standards of patient safety.
Routes of Drug Administration & Storage
Comprehensive Nursing Guide for Safe Medication Management
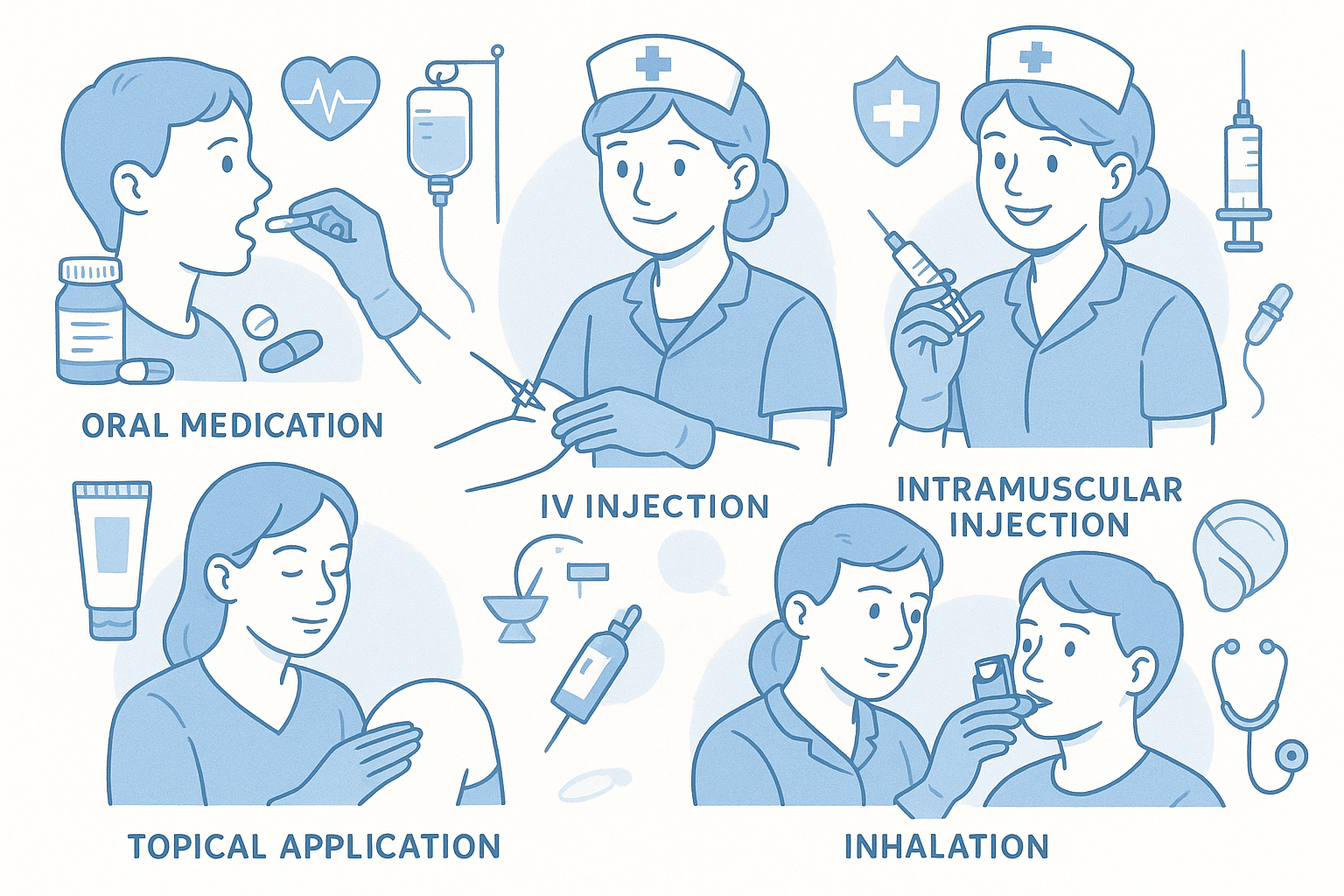
Table of Contents
Part I: Routes of Administration
Part II: Storage & Nursing Responsibilities
Introduction & Learning Objectives
Safe medication administration is one of the most critical responsibilities in nursing practice. Understanding the various routes of drug administration, proper storage techniques, and maintenance protocols is essential for delivering safe, effective patient care and preventing medication errors.
Learning Objectives
- Identify and describe the major routes of drug administration
- Understand the advantages, disadvantages, and nursing considerations for each route
- Demonstrate knowledge of proper drug storage and maintenance principles
- Recognize nursing responsibilities in medication management
- Apply safety protocols to prevent medication errors
- Implement evidence-based practices in clinical settings
Memory Aid: The “5 Rights Plus” of Medication Administration
Classic 5 Rights:
- Right Patient
- Right Drug
- Right Dose
- Right Route
- Right Time
Additional Rights:
- Right Documentation
- Right Assessment
- Reason/Indication
- Response/Evaluation
- Refusal Rights
Oral Route (PO – Per Os)
Advantages
- • Most convenient and cost-effective
- • Non-invasive and patient-friendly
- • Self-administration possible
- • Generally safer with lower risk of infection
- • Can be reversed if necessary (gastric lavage)
- • Various formulations available
Disadvantages
- • Slower onset of action
- • First-pass metabolism reduces bioavailability
- • Cannot use with unconscious patients
- • Affected by food, gastric pH, and GI motility
- • Risk of aspiration in dysphagia patients
- • Drug interactions with food and other medications
Oral Administration Process Flow
Critical Nursing Considerations for Oral Route
Assessment Points:
- • Gag reflex and swallowing ability
- • Level of consciousness and cooperation
- • Presence of nausea or vomiting
- • NPO status or dietary restrictions
- • Current GI function and conditions
Safety Measures:
- • Never crush enteric-coated or extended-release
- • Use appropriate crushing devices when needed
- • Ensure adequate fluid intake (unless restricted)
- • Monitor for signs of aspiration
- • Check for drug-food interactions
Mnemonic: “SWALLOW” for Oral Medication Safety
S – Swallowing ability assessed
W – Water or appropriate fluid ready
A – Aspiration risk evaluated
L – Level of consciousness confirmed
L – Look for contraindications
O – Observe patient during administration
W – Watch for immediate adverse reactions
Parenteral Routes
Intravenous (IV)
Advantages:
- • Rapid onset (immediate)
- • 100% bioavailability
- • Precise dosing control
- • Large volume capability
Risks:
- • Infection and phlebitis
- • Extravasation injury
- • Air embolism
- • Incompatibility reactions
Intramuscular (IM)
Advantages:
- • Faster than oral route
- • Good for depot injections
- • Larger volumes than subQ
- • Avoids GI tract
Considerations:
- • Proper site selection critical
- • Risk of nerve injury
- • Patient discomfort
- • Requires adequate muscle mass
Subcutaneous (SubQ)
Advantages:
- • Sustained drug release
- • Self-administration possible
- • Less painful than IM
- • Good for small volumes
Limitations:
- • Limited to small volumes (≤2mL)
- • Slower absorption
- • Risk of lipodystrophy
- • Affected by circulation
Injection Sites Reference Guide
| Route | Primary Sites | Max Volume | Needle Size | Key Landmarks |
|---|---|---|---|---|
| IM | Ventrogluteal, Deltoid, Vastus Lateralis | 3mL (deltoid: 1mL) | 22-25G, 1-1.5″ | ASIS, greater trochanter, iliac crest |
| SubQ | Abdomen, Upper arm, Thigh | 2mL | 25-27G, ⅜-⅝” | 2″ from umbilicus, fatty tissue |
| ID | Forearm, Upper back | 0.1mL | 26-27G, ⅜-½” | Avoid hair, scars, tattoos |
Mnemonic: “INJECT” for Parenteral Safety
I – Identify patient and verify order
N – New needle for each injection
J – Judge appropriate site and position
E – Examine site for contraindications
C – Clean with antiseptic and allow to dry
T – Track injection sites and rotate appropriately
Topical & Transdermal Routes
Topical Applications
Forms:
- • Creams and ointments
- • Gels and lotions
- • Powders and sprays
- • Eye/ear drops
- • Suppositories
Applications:
- • Local anti-inflammatory effects
- • Antimicrobial treatment
- • Pain relief (analgesics)
- • Wound care products
Transdermal Systems
Advantages:
- • Consistent drug levels
- • Improved compliance
- • Avoids first-pass metabolism
- • Reduced dosing frequency
- • Non-invasive application
Common Examples:
- • Nicotine patches
- • Fentanyl patches
- • Nitroglycerine patches
- • Hormone replacement patches
Special Nursing Considerations
Topical Administration:
- • Always wear gloves to prevent self-exposure
- • Clean application site before use
- • Apply thin, even layer unless specified otherwise
- • Avoid contaminating medication container
- • Monitor for local skin reactions
- • Document application site and patient response
Transdermal Patches:
- • Remove old patch before applying new one
- • Rotate application sites to prevent irritation
- • Apply to clean, dry, hairless skin
- • Press firmly for 10-15 seconds
- • Fold used patches in half before disposal
- • Check adherence during patient rounds
Respiratory Routes
Metered-Dose Inhalers (MDI)
- • Pressurized delivery system
- • Requires coordination
- • Often used with spacer
- • Prime before first use
- • Shake well before each use
Dry Powder Inhalers (DPI)
- • Breath-activated system
- • No coordination required
- • Requires adequate inspiratory flow
- • Keep dry and sealed
- • Don’t exhale into device
Nebulizers
- • Converts liquid to mist
- • Suitable for all ages
- • No coordination needed
- • Takes 10-15 minutes
- • Requires power source
MDI Administration Technique
Patient Education Priorities
Teaching Points:
- • Demonstrate proper technique repeatedly
- • Emphasize importance of technique on drug delivery
- • Provide written instructions and diagrams
- • Schedule return demonstrations
- • Discuss cleaning and maintenance
Common Errors to Address:
- • Inhaling too quickly (MDI)
- • Poor timing of actuation
- • Not shaking before use
- • Inadequate breath-holding
- • Poor device maintenance
Specialized Routes of Administration
Intrathecal
- • Direct CNS delivery
- • Chemotherapy, anesthetics
- • Strict aseptic technique
- • Monitor for complications
Epidural
- • Pain management
- • Anesthesia for surgery
- • Continuous infusion possible
- • Monitor respiratory status
Intraosseous
- • Emergency access
- • When IV access impossible
- • Rapid absorption
- • Temporary use only
Intra-articular
- • Direct joint injection
- • Corticosteroids
- • Hyaluronic acid
- • Sterile technique essential
High-Alert Considerations for Specialized Routes
Before Administration:
- • Verify specialized competency certification
- • Confirm appropriate indication and contraindications
- • Ensure emergency equipment availability
- • Obtain informed consent when required
- • Verify medication compatibility with route
During & After:
- • Maintain strict aseptic technique
- • Monitor vital signs continuously
- • Watch for immediate complications
- • Document procedure details thoroughly
- • Provide post-procedure patient education
Drug Storage Principles
Temperature Requirements
Room Temperature:
20-25°C (68-77°F)
Refrigerated:
2-8°C (36-46°F)
Frozen:
-25 to -10°C (-13 to 14°F)
Controlled Room Temperature:
15-30°C (59-86°F)
Light & Environmental Protection
- • Store in original containers when possible
- • Protect from direct sunlight
- • Use amber or opaque containers for light-sensitive drugs
- • Maintain appropriate humidity levels
- • Avoid storage near heat sources
- • Ensure adequate ventilation
Security Requirements
- • Controlled substances in locked storage
- • Limited access with proper authorization
- • Separate high-alert medications
- • Inventory tracking systems
- • Regular audits and counts
- • Proper disposal protocols
| Storage Category | Examples | Special Requirements | Monitoring Frequency |
|---|---|---|---|
| Refrigerated Medications | Insulin, vaccines, some antibiotics | Continuous temperature monitoring, backup power | Every 4 hours |
| Controlled Substances | Opioids, benzodiazepines | Double-locked cabinet, witness counts | Every shift change |
| High-Alert Medications | Chemotherapy, concentrated electrolytes | Separate storage, warning labels | Daily inventory |
| Light-Sensitive | Nitroprusside, some vitamins | Amber containers, dark storage areas | Weekly inspection |
Mnemonic: “STABLE” for Drug Storage
S – Security measures in place
T – Temperature control maintained
A – Access limited to authorized personnel
B – Barriers against light and moisture
L – Labels clear and legible
E – Expiration dates regularly checked
Maintenance & Stability
Factors Affecting Drug Stability
-
Temperature: Heat accelerates degradation; freezing can denature proteins
-
Light: UV radiation can break chemical bonds and cause photodegradation
-
Moisture: Can cause hydrolysis reactions and microbial growth
-
Air/Oxygen: Oxidation can alter drug structure and potency
-
pH: Extreme acidity or alkalinity can cause chemical breakdown
Signs of Drug Deterioration
Visual Changes:
- • Color changes or discoloration
- • Precipitation or crystallization
- • Cracking, chipping, or swelling
- • Separation of emulsions
Physical Changes:
- • Unusual odors
- • Texture changes
- • Gas formation or bubbling
- • Hardening or softening
Medication Stability Assessment Process
Check appearance, integrity, expiration dates
Temperature, humidity, light exposure logs
Record findings, report concerns to pharmacy
Remove compromised medications, investigate causes
Maintenance Best Practices for Nurses
Daily Responsibilities:
- • Check refrigerator and freezer temperatures
- • Inspect medication storage areas
- • Rotate stock using FIFO (First In, First Out)
- • Clean and organize storage areas
- • Document temperature logs and inspections
Weekly Tasks:
- • Comprehensive expiration date review
- • Deep cleaning of storage equipment
- • Review and update inventory counts
- • Check emergency backup systems
- • Communicate issues to pharmacy staff
Nursing Responsibilities in Medication Management
Assessment
- • Patient history and allergies
- • Current medications review
- • Physical assessment
- • Laboratory values
- • Functional status
Safety
- • Verify patient identity
- • Check allergies and contraindications
- • Ensure proper route selection
- • Monitor for adverse reactions
- • Implement fall precautions
Education
- • Medication purpose and effects
- • Proper administration technique
- • Side effects to report
- • Storage instructions
- • Compliance strategies
Monitoring
- • Therapeutic response
- • Adverse reactions
- • Vital signs changes
- • Laboratory trends
- • Patient compliance
High-Risk Medication Management
High-Alert Medications:
- • Anticoagulants (heparin, warfarin)
- • Insulin and hypoglycemics
- • Chemotherapy agents
- • Concentrated electrolytes
- • Neuromuscular blocking agents
- • IV sedation medications
Special Precautions:
- • Double verification required
- • Independent calculations
- • Standardized concentrations
- • Smart pump programming
- • Enhanced monitoring protocols
- • Immediate availability of antidotes
Documentation Requirements:
- • Time and route of administration
- • Patient response and vital signs
- • Any adverse reactions observed
- • Co-signature when required
- • Patient education provided
- • Waste witnessed and documented
Mnemonic: “NURSING” for Comprehensive Medication Management
N – Name verification (patient and medication)
U – Understand indication and contraindications
R – Route, rate, and timing verification
S – Safety checks and allergy confirmation
I – Identify potential interactions
N – Note patient response and effectiveness
G – Give thorough patient education
Safety Protocols & Documentation
Error Prevention Strategies
- • Use barcode scanning technology when available
- • Implement “Do Not Disturb” policies during medication preparation
- • Standardize medication administration times
- • Create visual cues for high-alert medications
- • Establish clear communication protocols
- • Regular competency assessments for staff
- • Maintain current drug reference resources
Documentation Standards
- • Document immediately after administration
- • Use only approved abbreviations
- • Include patient response and vital signs
- • Note any deviations from standard protocol
- • Record patient education provided
- • Document refusals and reasons
- • Sign and date all entries appropriately
Medication Error Response Protocol
Immediate Actions
Assess patient condition, vital signs
Report immediately, obtain orders
Administer antidote if indicated
Follow-up Actions
Complete incident reports, chronology
Report through proper channels
Continuous monitoring, family notification
Essential Documentation Elements
Before Administration:
- • Patient assessment findings
- • Vital signs and allergies confirmed
- • Medication verification completed
- • Patient education provided
- • Consent obtained when required
During Administration:
- • Exact time of administration
- • Route and site used
- • Dosage and concentration
- • Patient tolerance and cooperation
- • Any difficulties encountered
After Administration:
- • Patient response and effectiveness
- • Any adverse reactions noted
- • Post-administration assessments
- • Follow-up interventions
- • Communication with healthcare team
Clinical Implementation in Nursing Practice
Practical Application Scenarios
Understanding how to implement medication administration knowledge in real clinical situations is crucial for safe nursing practice. Here are key scenarios nurses commonly encounter:
Emergency Situations
Code Blue Medications:
- • IV epinephrine for cardiac arrest
- • Atropine for bradycardia
- • Amiodarone for arrhythmias
- • Rapid IV access establishment
Anaphylaxis Response:
- • IM epinephrine (EpiPen)
- • IV corticosteroids
- • H1 and H2 antihistamines
- • Continuous monitoring protocols
Routine Care Implementation
Medication Reconciliation:
- • Admission medication history
- • Transfer between units
- • Discharge planning and education
- • Home medication management
Patient Education Programs:
- • Diabetic medication teaching
- • Inhaler technique demonstrations
- • Anticoagulation monitoring
- • Pain management strategies
Interdisciplinary Collaboration
Pharmacist Partnership:
- • Medication review and optimization
- • Drug interaction screening
- • Dosing recommendations
- • Patient education support
- • Adverse reaction monitoring
Physician Collaboration:
- • Medication orders clarification
- • Patient response reporting
- • Side effect communication
- • Treatment plan modifications
- • Emergency medication requests
Patient/Family Engagement:
- • Medication adherence counseling
- • Side effect recognition training
- • Proper storage instruction
- • Refill scheduling assistance
- • Cultural considerations
Best Practice Implementation Strategies
Technology Integration:
- • Electronic health records optimization
- • Barcode medication administration
- • Smart pump programming
- • Clinical decision support systems
- • Mobile medication reference apps
Quality Improvement:
- • Medication error analysis
- • Process improvement initiatives
- • Staff education programs
- • Patient safety rounds
- • Evidence-based practice updates
Shift Medication Management Workflow
Review MAR, patient status, pending orders
Calculate doses, prepare syringes, check expiration dates
Administer medications, assess responses, provide education
Complete charts, communicate changes, prepare report
Transfer medication information to next shift
Summary & Key Takeaways
Safe medication administration requires comprehensive knowledge of routes, storage principles, and nursing responsibilities. Success depends on systematic approaches, continuous learning, and adherence to evidence-based practices.
Essential Competencies Achieved
- ✓ Mastery of major administration routes
- ✓ Understanding of pharmacokinetic principles
- ✓ Implementation of safety protocols
- ✓ Proper storage and maintenance practices
- ✓ Patient assessment and education skills
- ✓ Documentation and communication excellence
- ✓ Error prevention and response capabilities
Continuing Education Priorities
- • Stay current with new medication approvals
- • Participate in medication safety initiatives
- • Attend pharmacology update seminars
- • Practice emergency response protocols
- • Engage in interdisciplinary learning
- • Pursue specialized certification programs
- • Contribute to quality improvement projects
Final Mnemonic: “EXCELLENCE” in Medication Administration
E – Evidence-based practice implementation
X – eXamine patient thoroughly before administration
C – Confirm all rights of medication administration
E – Educate patient and family comprehensively
L – Look for adverse reactions and interactions
L – Learn continuously and stay updated
E – Ensure proper storage and handling
N – Never compromise on safety protocols
C – Communicate effectively with healthcare team
E – Evaluate outcomes and document thoroughly
Remember: Patient Safety is Paramount
Every medication administration is an opportunity to improve patient outcomes and demonstrate nursing excellence. When in doubt, seek clarification, verify information, and prioritize patient safety above all else.
“Safe medication administration is not just a skill—it’s a professional commitment to patient welfare.”
Routes of Drug Administration & Storage
Complete Nursing Guide with Clinical Applications
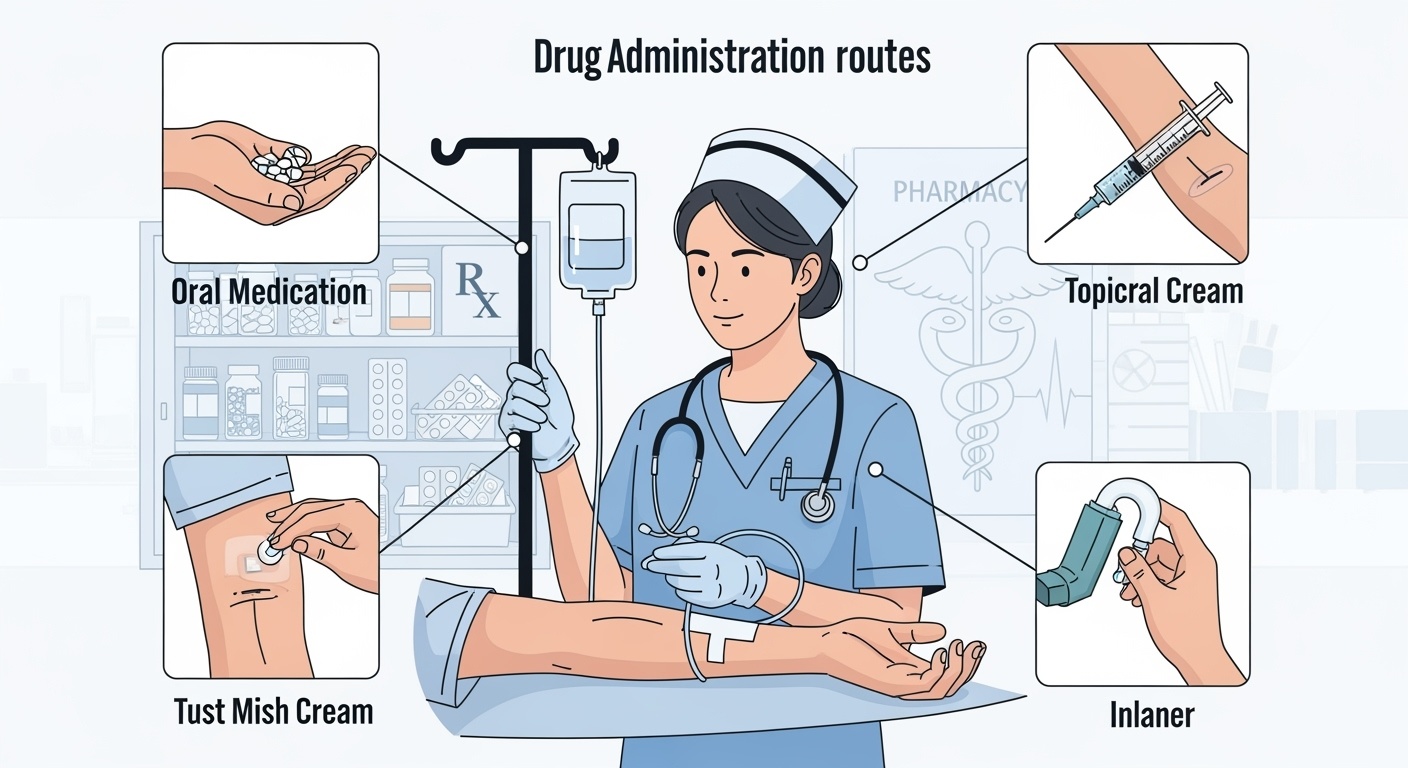
Table of Contents
1. Introduction to Drug Administration
Drug administration is a fundamental nursing skill that requires comprehensive knowledge of pharmacokinetics, patient safety protocols, and clinical decision-making. Understanding the various routes of drug administration is crucial for optimizing therapeutic outcomes while minimizing adverse effects.
Memory Aid: The 5 R’s of Drug Administration
- Right Patient – Verify identity using two identifiers
- Right Drug – Check medication name and form
- Right Dose – Calculate and verify dosage
- Right Route – Confirm administration method
- Right Time – Administer at prescribed intervals
Pharmacokinetics
The study of drug absorption, distribution, metabolism, and excretion (ADME) which determines the route selection.
Patient Safety
Priority consideration in all drug administration decisions, including allergy assessment and contraindication evaluation.
Clinical Judgment
Critical thinking skills required to assess patient condition and select appropriate administration routes.
2. Enteral Routes of Administration
Enteral routes involve drug administration through the gastrointestinal tract. These routes are generally safer, more convenient, and cost-effective compared to parenteral routes.
Oral Route (PO)
Advantages:
- Safe and convenient
- Cost-effective
- High patient compliance
- Self-administration possible
Disadvantages:
- First-pass metabolism
- Variable absorption
- Not suitable for unconscious patients
- Drug-food interactions
Sublingual/Buccal Route
Key Features:
- Rapid absorption
- Bypasses first-pass metabolism
- Rich blood supply
- Direct systemic circulation
Examples:
- Nitroglycerin tablets
- Buprenorphine films
- Ondansetron ODT
Enteral Feeding Routes
Nasogastric (NG)
Short-term use, nose to stomach placement
Percutaneous Endoscopic Gastrostomy (PEG)
Long-term feeding, direct stomach access
Jejunostomy
Post-pyloric feeding, bypasses stomach
Memory Aid: ORAL Assessment
- Order verification and patient identification
- Readiness to swallow assessment
- Allergies and contraindications check
- Location and positioning optimization
3. Parenteral Routes of Administration
Parenteral routes bypass the gastrointestinal tract, providing direct access to systemic circulation. These routes offer precise control over drug delivery but require sterile technique and specialized training.
Intravenous (IV)
- • Immediate effect
- • 100% bioavailability
- • Continuous infusion possible
- • High risk of complications
Intramuscular (IM)
- • Depot effect possible
- • Larger volumes tolerated
- • Painful injection
- • Risk of nerve damage
Subcutaneous (SC)
- • Self-administration feasible
- • Sustained absorption
- • Limited volume capacity
- • Lower absorption rate
Intradermal (ID)
- • Diagnostic testing
- • Allergy testing
- • Very small volumes
- • Localized response
IV Administration Flowchart
Injection Site Selection Guide
Intramuscular Sites:
- Deltoid: Small volumes (<1mL), vaccines
- Vastus Lateralis: Large volumes, pediatric preferred
- Ventrogluteal: Adults, Z-track technique
Subcutaneous Sites:
- Abdomen: Insulin administration preferred
- Upper Arms: Rotate sites regularly
- Thighs: Self-administration accessible
Memory Aid: STERILE Technique
- Sanitize hands thoroughly
- Take proper precautions
- Ensure sterile supplies
- Reach without contamination
- Inject using proper technique
- Label and document
- Evaluate patient response
4. Topical and Specialized Routes
Topical and specialized routes provide targeted drug delivery with minimal systemic effects. These routes are particularly valuable for local treatment and specialized therapeutic applications.
Topical
- Forms: Creams, ointments, gels, patches
- Benefits: Local action, minimal systemic effects
- Examples: Hydrocortisone cream, nicotine patches
Inhalation
- Devices: MDI, DPI, nebulizers
- Benefits: Direct lung delivery, rapid onset
- Examples: Albuterol, budesonide
Ophthalmic
- Forms: Drops, ointments, inserts
- Benefits: Local eye treatment
- Examples: Artificial tears, antibiotic drops
Neurological Routes
Intrathecal/Epidural:
- Direct CNS drug delivery
- Bypasses blood-brain barrier
- Used for anesthesia, pain management
- Requires specialized training
Cardiovascular Routes
Intra-arterial/Intra-cardiac:
- Emergency situations only
- Direct cardiac drug delivery
- High-risk procedures
- Physician administration required
Proper MDI Technique Steps
5. Drug Storage and Maintenance
Proper drug storage and maintenance are critical for maintaining medication efficacy, preventing contamination, and ensuring patient safety. Environmental factors significantly impact drug stability and therapeutic effectiveness.
Temperature Control
- Room Temperature: 20-25°C (68-77°F)
- Refrigerated: 2-8°C (36-46°F)
- Frozen: -25 to -10°C (-13 to 14°F)
- Controlled: 15-30°C (59-86°F)
Humidity Control
- Standard: <60% relative humidity
- Desiccants: Silica gel packets
- Monitoring: Hygrometers required
- Effects: Clumping, degradation prevention
Light Protection
- UV Protection: Amber containers
- Storage: Dark, cool places
- Photosensitive: Special handling required
- Examples: Furosemide, nitroglycerin
Controlled Substance Storage Requirements
Security Measures:
- Double-locked storage systems
- Limited access authorization
- Automated dispensing systems (ADS)
- 24/7 surveillance monitoring
- Regular inventory audits
Documentation Requirements:
- Perpetual inventory records
- DEA registration compliance
- Waste disposal documentation
- Transfer and receipt logs
- Discrepancy reporting protocols
Healthcare Facility Storage Areas
Central Pharmacy
Bulk storage, compounding
Unit Stock
Floor stock, emergency medications
Patient-Specific
Individualized medication storage
Emergency Cart
Code blue, rapid response
Memory Aid: FIFO Rotation System
- First medications received
- In storage should be the
- First medications
- Out for patient use
This system prevents medication expiration and ensures optimal drug potency.
6. Nursing Responsibilities in Drug Administration
Nurses play a pivotal role in medication administration, serving as the final checkpoint in the medication delivery process. This responsibility encompasses assessment, administration, monitoring, and patient education.
Pre-Administration Assessment
Patient Assessment:
- Verify patient identity using two identifiers
- Review medication allergies and intolerances
- Assess current vital signs and clinical status
- Evaluate laboratory values and diagnostic results
- Review concurrent medications for interactions
Order Verification:
- Confirm prescription completeness and legibility
- Verify dosage calculations and conversions
- Check route appropriateness for patient condition
- Confirm timing and frequency requirements
- Question unclear or inappropriate orders
During Administration
- Sterile Technique: Maintain asepsis for parenteral routes
- Patient Positioning: Optimize for safety and absorption
- Continuous Monitoring: Observe for immediate reactions
- Patient Communication: Explain procedure and expectations
- Documentation: Record immediately after administration
Post-Administration Monitoring
- Therapeutic Response: Assess efficacy indicators
- Adverse Reactions: Monitor for side effects
- Vital Sign Changes: Track hemodynamic responses
- Patient Comfort: Address pain or discomfort
- Follow-up Care: Plan continued monitoring
Legal and Ethical Responsibilities
Legal Obligations:
- Practice within nursing scope
- Follow institutional policies
- Maintain accurate documentation
- Report medication errors
- Protect patient confidentiality
Ethical Principles:
- Patient autonomy respect
- Beneficence and non-maleficence
- Justice in care delivery
- Informed consent facilitation
- Cultural sensitivity maintenance
Professional Standards:
- Continuing education requirements
- Competency maintenance
- Quality improvement participation
- Evidence-based practice
- Collegial collaboration
Patient and Family Education Components
Medication Information:
- • Drug name, purpose, and expected effects
- • Dosage schedule and administration techniques
- • Common side effects and when to report
- • Drug interactions and precautions
- • Storage requirements and expiration dates
Safety Education:
- • Importance of adherence to prescribed regimen
- • Recognition of adverse reactions
- • When to contact healthcare providers
- • Proper disposal of unused medications
- • Follow-up appointment scheduling
Memory Aid: LEARN Patient Education
- Listen to patient concerns and questions
- Explain medication purpose and effects
- Acknowledge patient understanding
- Reinforce key safety information
- Negotiate realistic adherence strategies
7. Safety Considerations and Error Prevention
Medication safety is paramount in nursing practice. Understanding common error types, prevention strategies, and emergency response protocols is essential for safe patient care.
High-Alert Medications (ISMP List)
Anticoagulants:
- Heparin (all forms)
- Warfarin
- Direct oral anticoagulants
- Thrombolytics
Insulin Products:
- Rapid-acting insulins
- Long-acting insulins
- Concentrated formulations
- IV insulin infusions
Other High-Risk:
- Narcotics and opioids
- Chemotherapy agents
- Neuromuscular blockers
- Concentrated electrolytes
System-Based Prevention
- Computerized Order Entry: Reduces transcription errors
- Barcode Scanning: Ensures correct medication matching
- Automated Dispensing: Controls access and tracking
- Clinical Decision Support: Alerts for interactions
- Standardized Protocols: Consistent practices
Individual Prevention
- Double-Check Procedures: Independent verification
- Read-Back Protocols: Verbal order confirmation
- Distraction Management: Minimize interruptions
- Fatigue Recognition: Know personal limitations
- Continuing Education: Stay current with practices
Look-Alike Sound-Alike (LASA) Medications
Common Examples:
- • Celebrex vs. Celexa
- • Hydroxyzine vs. Hydralazine
- • Clonidine vs. Clonazepam
- • Prednisone vs. Prednisolone
Prevention Strategies:
- • Tall Man lettering
- • Separate storage locations
- • Color-coded labels
- • Computer alerts
Verification Steps:
- • Read labels carefully
- • Check generic names
- • Verify indication
- • Confirm with pharmacist
Medication Error Response Protocol
Memory Aid: SAFE Medication Practice
- Stop and think before administering
- Ask questions when uncertain
- Follow established protocols consistently
- Evaluate patient response continuously
8. Clinical Applications and Case Studies
Understanding practical applications of drug administration principles through real-world scenarios enhances clinical decision-making skills and promotes safe practice patterns.
Case Study 1: Emergency Medication Administration
Scenario:
A 65-year-old patient presents with acute chest pain. The physician orders nitroglycerin 0.4 mg sublingual every 5 minutes × 3 doses for chest pain relief.
Nursing Considerations:
- Assess blood pressure before each dose
- Monitor for hypotension (hold if SBP <90)
- Instruct patient not to swallow tablet
- Document pain level and response
Route Selection Rationale:
- Sublingual chosen because:
- • Rapid absorption (1-3 minutes)
- • Bypasses first-pass metabolism
- • Emergency situation requires quick action
- • Patient conscious and able to cooperate
Monitoring:
- • Vital signs every 5 minutes
- • Pain scale assessment
- • Signs of improvement or deterioration
Case Study 2: Pediatric Medication Administration
Scenario:
A 3-year-old child (15 kg) requires acetaminophen for fever reduction. The order is for 15 mg/kg PO every 6 hours PRN fever >38.5°C.
Calculations:
- 15 mg/kg × 15 kg = 225 mg per dose
- Available: 160 mg/5 mL suspension
- 225 mg ÷ 160 mg × 5 mL = 7.03 mL
Pediatric Considerations:
- • Use oral syringe for accurate measurement
- • Position child upright to prevent aspiration
- • Administer slowly in small amounts
- • Consider palatability and flavoring
- • Involve parents in administration when appropriate
Safety Checks:
- • Double-check weight-based calculations
- • Verify concentration of liquid medication
- • Confirm maximum daily dose not exceeded
Case Study 3: Geriatric Patient with Multiple Routes
Scenario:
An 82-year-old patient with dysphagia requires multiple medications: PPI for GERD, antibiotic for UTI, and pain management post-surgery.
Route Modifications:
- PPI: Crushing not recommended – use IV formulation
- Antibiotic: Switch to IV equivalent
- Pain medication: Transdermal patch or IV options
Geriatric Considerations:
- • Age-related pharmacokinetic changes
- • Increased sensitivity to medications
- • Higher risk of adverse reactions
- • Polypharmacy concerns
- • Cognitive assessment for compliance
Monitoring Priorities:
- • Renal function for dose adjustments
- • Drug accumulation signs
- • Falls risk assessment
Special Population Considerations
Neonates/Infants
- • Immature organ systems
- • Weight-based dosing
- • Limited IV access
Pediatric
- • Developmental considerations
- • Parent involvement
- • Age-appropriate forms
Pregnancy
- • Teratogenic risk assessment
- • Physiologic changes
- • Fetal considerations
Geriatric
- • Decreased clearance
- • Polypharmacy issues
- • Cognitive factors
Key Takeaways for Nursing Practice
Essential Principles:
- • Patient safety is the paramount concern in all medication administration
- • Route selection significantly impacts drug efficacy and patient outcomes
- • Proper storage and handling maintain medication integrity
- • Nursing responsibilities extend beyond administration to education and monitoring
- • Error prevention requires systematic approaches and vigilant practice
Professional Development:
- • Continuous learning enhances medication administration competency
- • Evidence-based practice guides optimal drug delivery methods
- • Interdisciplinary collaboration improves patient outcomes
- • Quality improvement initiatives advance medication safety
- • Professional accountability drives excellence in nursing practice
