Medication Terminologies & Abbreviations
Decoding Prescriptions with Developmental Considerations in Nursing
Table of Contents
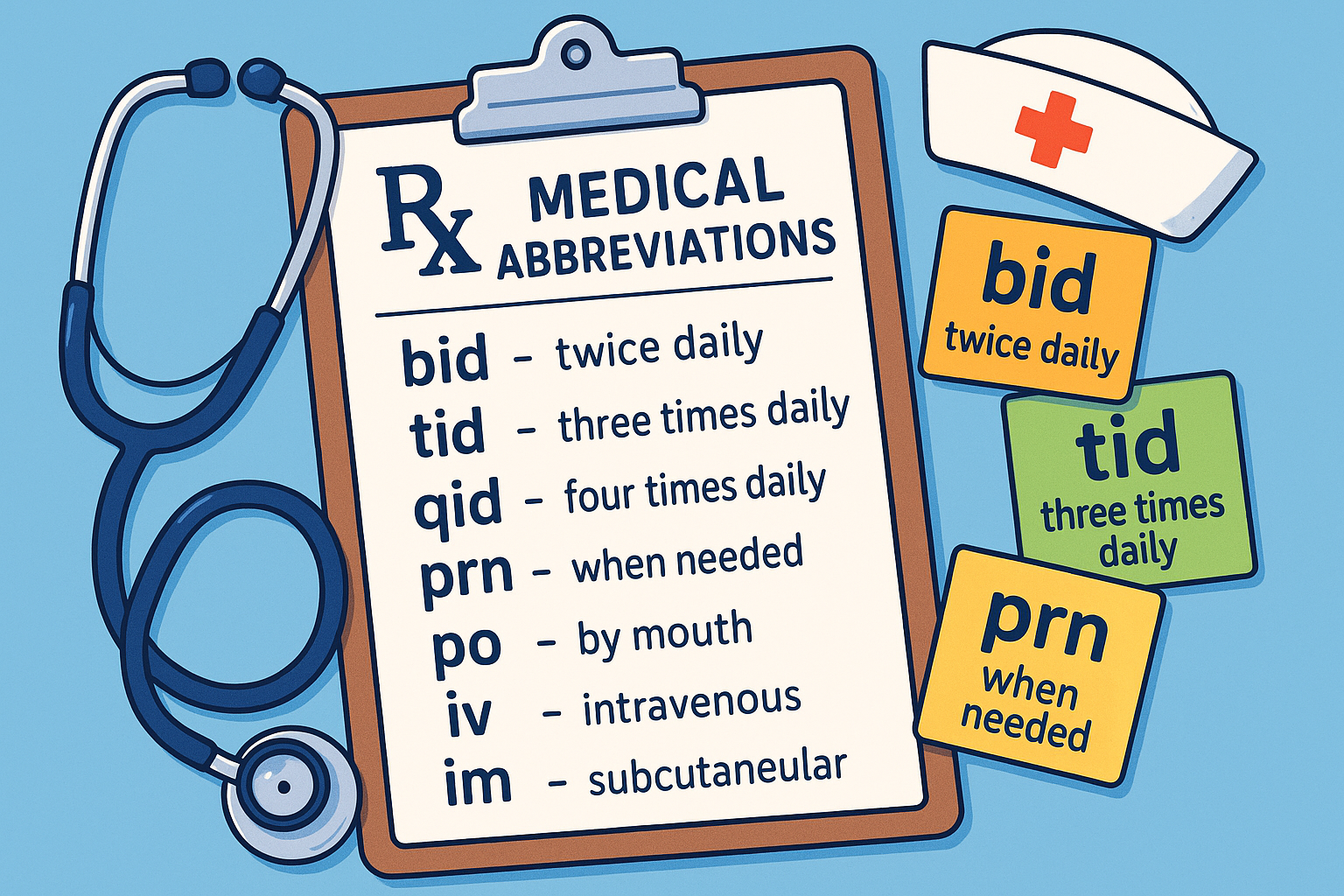
Common prescription abbreviations and terminologies used in healthcare
Introduction to Medication Safety in Nursing Practice
Why Understanding Abbreviations Matters
Medication errors are among the leading causes of preventable patient harm in healthcare settings. Understanding prescription abbreviations and medication terminologies is crucial for safe nursing practice and patient care delivery.
As nursing professionals, we serve as the final checkpoint in the medication administration process. Our ability to accurately interpret prescription abbreviations, understand medication terminologies, and apply developmental considerations can literally mean the difference between life and death for our patients.
Medication Errors
Cause over 7,000 deaths annually in the US
Prevention Rate
95% of medication errors are preventable
Nursing Role
Final safety checkpoint in medication delivery
Learning Objectives
- Master common prescription abbreviations and their meanings
- Understand developmental considerations across age groups
- Apply safety principles to prevent medication errors
- Utilize memory techniques for complex medical terminologies
Common Prescription Abbreviations
Understanding prescription abbreviations is fundamental to safe medication administration. These standardized abbreviations help healthcare professionals communicate medication orders efficiently while maintaining accuracy and safety.
| Abbreviation | Meaning | Context | Safety Notes |
|---|---|---|---|
| Rx | Prescription/Treatment | Universal symbol for prescription | Always verify with licensed prescriber |
| Sig | Directions for use | Patient instructions section | Ensure patient understanding |
| Disp | Dispense | Quantity to provide | Verify correct quantity |
| NKA | No Known Allergies | Allergy status documentation | Always double-check allergies |
| NKDA | No Known Drug Allergies | Specific to medication allergies | Monitor for new reactions |
High-Alert Abbreviations to Avoid
The Institute for Safe Medication Practices (ISMP) has identified dangerous abbreviations that should never be used due to high error potential.
Never Use: U or u
Can be mistaken for 0, 4, or cc
Use: “units” instead
Never Use: IU
Can be mistaken for IV or 10
Use: “international units”
Never Use: QD, QOD
Mistaken for each other
Use: “daily” or “every other day”
Never Use: MS, MSO4
Can be confused for magnesium
Use: “morphine sulfate”
Frequency & Timing Abbreviations
Proper timing of medication administration is critical for therapeutic effectiveness and patient safety. Understanding frequency abbreviations ensures medications are given at optimal intervals for maximum benefit.
Common Frequency Terms
Administered every 12 hours (8 AM, 8 PM typical)
Every 8 hours (8 AM, 4 PM, 12 AM typical)
Every 6 hours (6 AM, 12 PM, 6 PM, 12 AM)
Given based on patient need and assessment
Specific Timing Indicators
Usually 30 minutes before eating
Usually 30 minutes to 1 hour after eating
Hour of sleep – typically 9-10 PM
Urgent administration – within 15 minutes
Timing Considerations for Different Age Groups
Pediatric Patients
- • Coordinate with feeding schedules
- • Consider sleep patterns
- • Account for school hours
Adult Patients
- • Work around meal times
- • Consider work schedules
- • Respect sleep cycles
Geriatric Patients
- • Early morning medications
- • Avoid late evening doses
- • Consider cognitive patterns
Routes of Administration Abbreviations
The route of medication administration significantly affects drug absorption, onset time, and therapeutic effect. Understanding route abbreviations is essential for safe and effective medication delivery across all patient populations.
Enteral Routes
Most common oral administration route
Contraindicated if NPO or dysphagia
Under the tongue for rapid absorption
Do not swallow, drink, or eat immediately
Via feeding tube to stomach
Verify tube placement before administration
Parenteral Routes
Direct access to bloodstream – fastest onset
Highest bioavailability, immediate effect
Into muscle tissue for sustained release
Good absorption, moderate onset time
Into fatty tissue under skin
Slower absorption, longer duration
Topical & Specialized Routes
OU, OD, OS
Both eyes, right eye, left eye
AU, AD, AS
Both ears, right ear, left ear
TOP
Topically to skin
INH
Inhalation route
Route Selection Based on Patient Factors
Consider Patient Age:
- • Infants: Often IV, IM, or rectal routes
- • Children: PO when possible, avoid IM when feasible
- • Adults: All routes available based on condition
- • Elderly: Consider swallowing difficulties, skin integrity
Consider Clinical Factors:
- • Consciousness level and ability to swallow
- • Severity and urgency of condition
- • Drug properties and formulation
- • Patient preferences and comfort
Dosage & Measurement Terminologies
Accurate dosage calculations and understanding measurement units are critical nursing skills. Proper interpretation of dosage abbreviations prevents medication errors and ensures therapeutic effectiveness across all patient age groups.
Weight-Based Units
Volume-Based Units
Concentration Units
Critical Dosage Calculation Formulas
Basic Dose Calculation
Dose = (Desired × Volume) ÷ Available
Use when converting between different concentrations
Weight-Based Dosing
Dose = Weight (kg) × mg/kg
Essential for pediatric and many adult medications
IV Flow Rate
mL/hr = Total Volume ÷ Time (hours)
For continuous IV medication infusions
Unit Conversion
1 g = 1000 mg = 1,000,000 mcg
Master these conversions to prevent errors
High-Risk Calculation Scenarios
Pediatric Considerations:
- • Always verify weight in kilograms
- • Double-check decimal placement
- • Use pediatric-specific references
- • Consider body surface area calculations
- • Have second nurse verify high-risk drugs
Geriatric Considerations:
- • Account for decreased organ function
- • Consider polypharmacy interactions
- • Start with lower doses when appropriate
- • Monitor for cumulative effects
- • Adjust for renal/hepatic impairment
Developmental Considerations in Medication Management
Understanding how age and development affect medication metabolism, absorption, and response is crucial for safe nursing practice. Each developmental stage presents unique challenges and considerations for medication administration.
Physiological Changes Across the Lifespan
| System | Infants | Children | Adults | Elderly |
|---|---|---|---|---|
| Absorption | Higher gastric pH, slower gastric emptying | Approaching adult values | Baseline normal function | Decreased acid production, delayed emptying |
| Distribution | Higher body water, lower protein | Transitioning to adult ratios | Standard water/protein ratios | Decreased water, altered protein binding |
| Metabolism | Immature liver enzymes | Rapid metabolism | Full enzyme activity | Decreased enzyme activity |
| Elimination | Immature kidney function | Adult-like function | Optimal renal function | Decreased glomerular filtration |
Pharmacokinetic Considerations
Absorption Factors
- • Gastric pH variations affect drug stability
- • Gastric emptying time influences onset
- • Surface area differences impact absorption rate
- • First-pass metabolism varies by age
Distribution Patterns
- • Body composition affects drug distribution
- • Protein binding capacity varies
- • Blood-brain barrier permeability changes
- • Tissue binding affects drug availability
Pharmacodynamic Considerations
Receptor Sensitivity
- • Age-related receptor density changes
- • Altered drug-receptor interactions
- • Modified cellular response patterns
- • Varied therapeutic windows
Side Effect Profiles
- • Age-specific adverse reactions
- • Increased sensitivity to certain drugs
- • Different manifestation patterns
- • Varied tolerance levels
Age-Appropriate Dosing Strategies
Neonates (0-28 days)
- • Weight-based dosing essential
- • Frequent monitoring required
- • Extended dosing intervals
- • Organ immaturity considerations
Infants (1-12 months)
- • Rapid growth adjustments
- • Developing enzyme systems
- • BSA calculations important
- • Frequent dose reassessment
Children (1-12 years)
- • Higher mg/kg requirements
- • Faster metabolism rates
- • Age-appropriate formulations
- • Growth-based adjustments
Adolescents (13-18 years)
- • Approaching adult dosing
- • Hormonal influences
- • Compliance considerations
- • Transition planning
Pediatric Medication Management
Pediatric medication administration requires specialized knowledge and careful attention to developmental physiology. Understanding how children differ from adults in drug processing and response is essential for safe practice and optimal therapeutic outcomes.
Pediatric Dosing Calculations
Weight-Based Dosing
Dose = Weight (kg) × mg/kg/day
- • Most common pediatric dosing method
- • Requires accurate current weight
- • May need to divide total daily dose
- • Always verify maximum adult dose
Body Surface Area (BSA)
BSA = √[(Height cm × Weight kg) ÷ 3600]
- • More accurate for chemotherapy drugs
- • Accounts for metabolic activity
- • Used for high-risk medications
- • Requires height and weight
Age-Specific Administration Techniques
Infants (0-12 months)
- Use oral syringes for liquid medications
- Administer slowly to prevent choking
- Hold infant upright or semi-upright
- Use taste masking when possible
Toddlers (1-3 years)
- Offer choices when appropriate
- Use positive reinforcement
- Have parent assist if possible
- Be firm but gentle if resistance
School Age (4-12 years)
- Explain procedure in simple terms
- Encourage self-administration when safe
- Use age-appropriate rewards
- Teach about medication purpose
Pediatric High-Alert Situations
Critical Safety Checks:
- • Verify weight in kilograms (not pounds)
- • Double-check decimal point placement
- • Confirm age-appropriate medication
- • Verify maximum safe dose limits
- • Check for pediatric contraindications
- • Ensure appropriate concentration
Common Error Sources:
- • Calculation errors with small doses
- • Using adult formulations
- • Incorrect weight documentation
- • Misreading micrograms vs milligrams
- • Inappropriate route selection
- • Inadequate monitoring frequency
Family-Centered Care in Medication Management
Parent Education:
- • Medication purpose and expected effects
- • Proper administration techniques
- • Side effects to monitor
- • When to contact healthcare provider
Home Safety:
- • Proper storage requirements
- • Child-resistant packaging
- • Disposal of unused medications
- • Emergency contact information
Compliance Strategies:
- • Age-appropriate explanations
- • Reward systems for cooperation
- • Medication schedules and reminders
- • Involving child in age-appropriate ways
Geriatric Medication Considerations
Older adults present unique challenges in medication management due to age-related physiological changes, multiple comorbidities, and polypharmacy. Understanding geriatric-specific considerations for medication abbreviations and administration is crucial for preventing adverse events and optimizing therapeutic outcomes.
Age-Related Physiological Changes
Cardiovascular Changes
- • Decreased cardiac output affects drug distribution
- • Reduced blood flow to organs slows metabolism
- • Increased sensitivity to cardiovascular drugs
- • Higher risk of orthostatic hypotension
Renal Function Decline
- • Decreased glomerular filtration rate
- • Reduced drug clearance and elimination
- • Risk of drug accumulation and toxicity
- • Need for dose adjustments in many drugs
Polypharmacy and Drug Interactions
Common Polypharmacy Issues
- • Average of 5+ medications per elderly patient
- • Increased risk of drug-drug interactions
- • Cumulative side effects and adverse reactions
- • Medication cascade effects
- • Compliance challenges with complex regimens
High-Risk Drug Combinations
- • Warfarin + NSAIDs (bleeding risk)
- • ACE inhibitors + Potassium supplements
- • Digoxin + Diuretics (toxicity risk)
- • Sedatives + Hypnotics (fall risk)
- • Multiple anticholinergic medications
Beers Criteria and Inappropriate Medications
| Drug Class | Examples | Concerns in Elderly | Nursing Implications |
|---|---|---|---|
| Anticholinergics | Diphenhydramine, Atropine | Cognitive impairment, confusion | Monitor mental status closely |
| Benzodiazepines | Lorazepam, Diazepam | Fall risk, cognitive decline | Implement fall precautions |
| NSAIDs | Ibuprofen, Naproxen | GI bleeding, kidney damage | Monitor for GI symptoms |
| Muscle Relaxants | Cyclobenzaprine | Sedation, anticholinergic effects | Assess for alternative therapies |
Geriatric-Friendly Medication Practices
Assessment Priorities:
- • Comprehensive medication review
- • Cognitive and physical function assessment
- • Fall risk evaluation
- • Swallowing ability assessment
- • Vision and hearing capabilities
Administration Strategies:
- • “Start low, go slow” principle
- • Simplify medication regimens
- • Use larger print labels
- • Consider alternative formulations
- • Implement pill organizers
Monitoring Focus:
- • Increased frequency of assessments
- • Watch for subtle side effects
- • Monitor functional status changes
- • Regular medication reconciliation
- • Family and caregiver involvement
Medication Error Prevention Strategies
Medication errors are a significant patient safety concern, but they are largely preventable through systematic approaches and understanding of common error patterns. Mastering error prevention strategies is essential for safe nursing practice across all patient populations.
The Five Rights of Medication Administration
Right Patient
- • Two patient identifiers
- • Verbal confirmation
- • Wristband verification
Right Drug
- • Check drug name
- • Verify spelling
- • Confirm formulation
Right Dose
- • Double-check calculations
- • Verify units
- • Age-appropriate dosing
Right Route
- • Verify administration path
- • Check contraindications
- • Assess patient ability
Right Time
- • Check frequency
- • Verify timing
- • Consider interactions
Additional Safety Rights
Right Documentation
- • Accurate medication record
- • Timely documentation
- • Complete information
Right Reason
- • Understand indication
- • Verify appropriateness
- • Question if unclear
Right Response
- • Monitor for effectiveness
- • Watch for adverse effects
- • Follow up appropriately
Right Education
- • Patient understanding
- • Clear instructions
- • Safety information
Common Sources of Medication Errors
System-Related Factors:
- • Look-alike, sound-alike medications (LASA)
- • Poor handwriting or unclear orders
- • Inadequate lighting or workspace
- • Interruptions during medication preparation
- • Complex medication regimens
- • Inadequate staffing or time pressure
Human Factors:
- • Calculation errors and decimal misplacement
- • Failure to verify patient identity
- • Knowledge deficits about medications
- • Fatigue and stress affecting performance
- • Communication failures between staff
- • Overconfidence leading to shortcuts
Evidence-Based Error Prevention Strategies
Technology Solutions:
- • Computerized Provider Order Entry (CPOE)
- • Barcode medication administration
- • Smart infusion pumps
- • Clinical decision support systems
- • Automated dispensing systems
Process Improvements:
- • Standardized medication protocols
- • Double-check systems for high-risk drugs
- • Medication reconciliation processes
- • Structured communication methods
- • Regular medication safety training
Cultural Changes:
- • Just culture approach to errors
- • Encourage reporting and learning
- • Team-based safety initiatives
- • Patient and family involvement
- • Continuous quality improvement
Memory Aids & Mnemonics for Medication Safety
Memorizing complex medication abbreviations and safety protocols can be challenging. These carefully crafted mnemonics and memory aids will help you retain critical information and apply it consistently in clinical practice, ultimately improving patient safety outcomes.
Essential Safety Mnemonics
RIGHTS: Medication Safety
Right Patient
Identify Drug
Get Right Dose
Healthy Route
Time Correctly
Safety Documentation
Remember the fundamental rights every time you administer medication
DOSE: Calculation Safety
Double-check calculations
Order appropriateness
Safety limits verified
Evaluate patient factors
Critical steps for safe dose calculations
SAFE: High-Alert Medications
Second nurse verification
Accurate calculation check
Frequent monitoring required
Extra documentation needed
Special precautions for high-risk medications like insulin, heparin, chemotherapy
KIDS: Pediatric Safety
Kilograms for weight
Infusion rate carefully
Developmental considerations
Safety dose limits
Essential reminders for pediatric medication administration
Abbreviation Memory Techniques
Frequency Helpers
BID = “Buy It Daily” (twice)
Every 12 hours
TID = “Take It Daily” (three times)
Every 8 hours
QID = “Quite In Demand” (four times)
Every 6 hours
Route Reminders
PO = “Put in Oral cavity”
By mouth
IV = “Into Vein”
Intravenous
IM = “Into Muscle”
Intramuscular
Timing with Meals
AC = “Always Come early”
Before meals
PC = “Please Come after”
After meals
HS = “Hit the Sack”
At bedtime
Visual Memory Aids
Dangerous Abbreviations Visual
U IU QD MS
Picture these with a big red X
Visualize these abbreviations with warning signs to remember they’re dangerous
Eye & Ear Memory Aid
OU OD OS
AU AD AS
Use the body part visual to remember which abbreviations go with eyes vs ears
Memory Enhancement Strategies
Active Learning:
- • Create your own abbreviation mnemonics
- • Practice with flashcards daily
- • Teach abbreviations to study partners
- • Use spaced repetition techniques
Visual Techniques:
- • Draw pictures to represent abbreviations
- • Use color coding for different categories
- • Create mind maps connecting related terms
- • Post key abbreviations in clinical areas
Practical Application:
- • Practice reading real prescriptions
- • Quiz yourself during clinical rotations
- • Join study groups focused on pharmacology
- • Use apps and online resources regularly
Practical Applications in Clinical Settings
Translating theoretical knowledge of medication abbreviations into safe clinical practice requires understanding real-world scenarios and developing systematic approaches to medication administration. These practical applications demonstrate how to apply safety principles across diverse clinical environments.
Case Study Applications
Case Study 1: Pediatric Emergency
6-year-old, 22 kg child with fever in emergency department
Order: Acetaminophen 15 mg/kg PO q6h PRN fever
Step 1: Calculate dose: 22 kg × 15 mg/kg = 330 mg
Step 2: Verify maximum dose: 330 mg < 650 mg (adult max) ✓
Step 3: Select appropriate formulation: liquid suspension
Step 4: Patient education: explain to parent and child
Result: Safe, effective fever management
Case Study 2: Elderly Patient with Polypharmacy
82-year-old with heart failure, diabetes, and arthritis
Furosemide 40mg PO BID, Metformin 500mg PO BID with meals, Ibuprofen 200mg PO TID PRN pain
Issue Identified: NSAIDs contraindicated with heart failure
Action: Contact prescriber about pain management alternatives
Education: Discuss timing of medications with meals
Monitoring: Daily weights, blood glucose, kidney function
Result: Safer medication regimen with reduced interactions
Clinical Environment Applications
Emergency Department
- • Rapid medication preparation under pressure
- • STAT orders requiring immediate attention
- • Weight-based dosing for pediatric patients
- • High-alert medications like epinephrine
- • Clear communication during resuscitation
Key Focus: Speed with accuracy, double-checking critical calculations
Intensive Care Unit
- • Complex IV drip calculations and titrations
- • Multiple concurrent medication infusions
- • Frequent dosage adjustments based on response
- • Precise timing for critical medications
- • Compatibility considerations for IV lines
Key Focus: Precision dosing, continuous monitoring, complex calculations
Medical-Surgical Floor
- • Routine medication administration schedules
- • Patient education and discharge planning
- • Managing PRN medications effectively
- • Coordinating timing with meals and activities
- • Documentation and medication reconciliation
Key Focus: Patient education, routine safety checks, comprehensive care
Medication Administration Checklist for Clinical Practice
Pre-Administration:
- Review medication order for completeness
- Verify patient allergies and contraindications
- Check drug interactions with current medications
- Calculate and verify dosage appropriateness
- Assess patient’s ability to receive medication
- Gather necessary equipment and supplies
During Administration:
- Verify patient identity with two identifiers
- Explain medication purpose and effects to patient
- Administer via correct route and technique
- Stay with patient during administration
- Monitor for immediate adverse reactions
- Document administration immediately
Transitioning from Student to Professional Practice
Building Confidence:
- • Start with routine medications in familiar settings
- • Gradually take on more complex medication regimens
- • Ask questions when uncertain about abbreviations
- • Observe experienced nurses in challenging situations
- • Practice calculations regularly to maintain proficiency
Professional Development:
- • Join medication safety committees when possible
- • Attend continuing education on pharmacology
- • Stay updated on new medication abbreviations
- • Participate in quality improvement initiatives
- • Share knowledge with newer students and staff
Global Best Practices in Medication Safety
Learning from international healthcare systems and their approaches to medication safety can enhance our understanding and improve patient outcomes. These global best practices demonstrate innovative solutions to common medication safety challenges that can be adapted to various healthcare settings.
International Medication Safety Initiatives
United Kingdom: NHS Medication Safety
Electronic Prescribing Systems
Nationwide implementation of electronic prescribing to reduce handwriting errors and improve medication reconciliation.
Medication Safety Officers
Dedicated roles in each trust focused on medication error prevention and safety culture development.
Patient Safety Alerts
Rapid communication system for sharing medication safety learnings across the entire NHS network.
Australia: National Medication Safety Program
Medication Reconciliation Standards
Standardized processes for medication history taking and reconciliation at all transition points.
High-Risk Medication Lists
Nationally agreed upon lists of high-risk medications requiring special handling protocols.
Consumer Medication Safety
Programs focused on patient education and involvement in medication safety processes.
