Complete Guide to Medical Equipment
Syringes, Needles, Cannulas & Infusion Sets for Nursing Students
Table of Contents
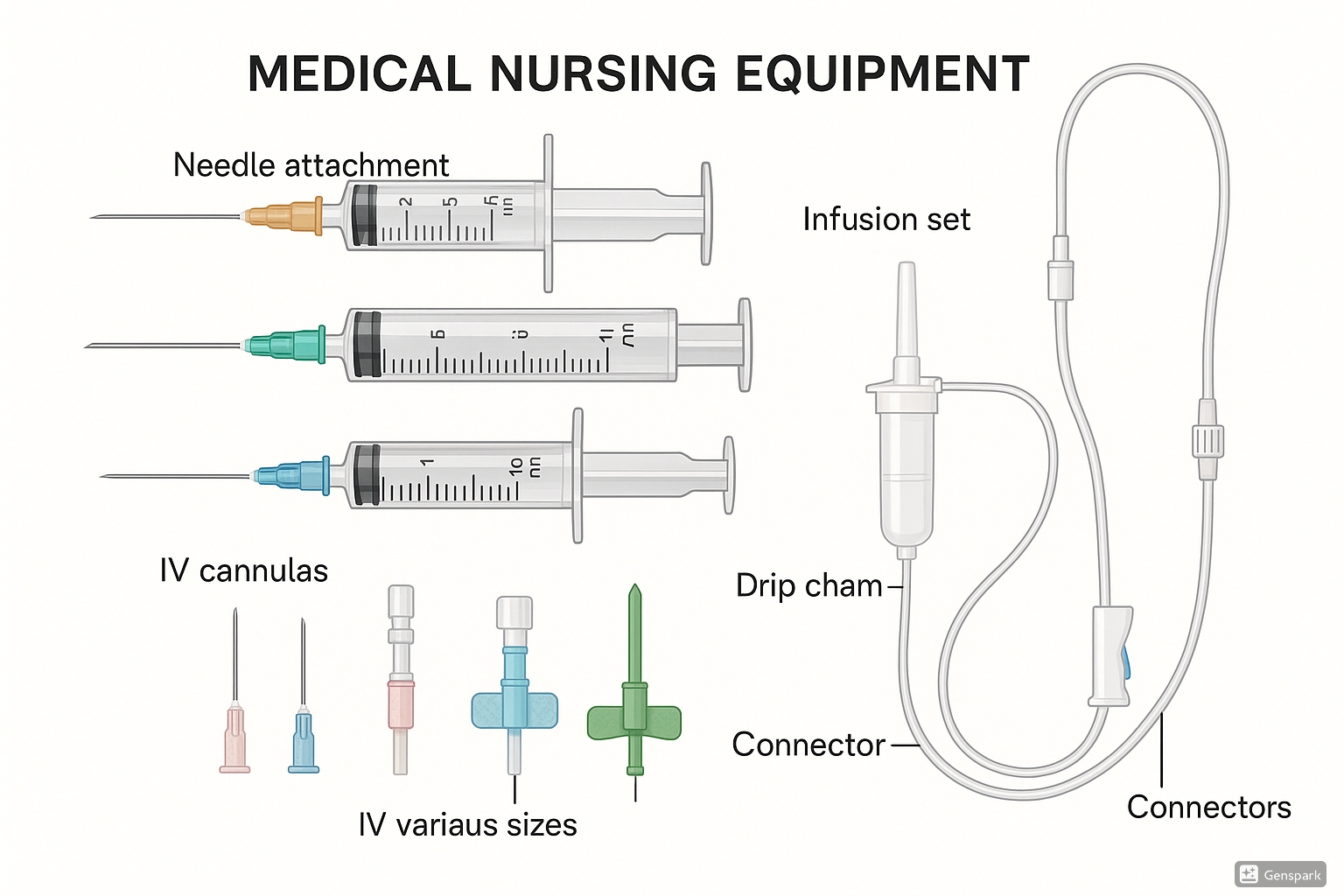
Comprehensive overview of essential medical equipment used in nursing practice
Introduction to Medical Equipment
Why Master Medical Equipment?
Understanding medical equipment is fundamental to safe, effective nursing practice. Every piece of medical equipment serves a specific purpose in patient care, from delivering medications to maintaining fluid balance. This comprehensive guide will transform you from a novice to a confident practitioner in handling essential medical equipment.
In modern healthcare, nurses interact with various types of medical equipment daily. The proper selection, handling, and application of syringes, needles, cannulas, and infusion sets directly impact patient outcomes and safety. This guide provides evidence-based knowledge to help nursing students master these essential tools.
Medical equipment mastery involves understanding not just the physical components, but also the clinical reasoning behind equipment selection. Each piece of medical equipment has specific indications, contraindications, and optimal usage scenarios that every nursing professional must comprehend.
Patient Safety
Proper medical equipment usage prevents complications and ensures optimal patient outcomes.
Professional Excellence
Mastering medical equipment enhances clinical competence and professional confidence.
Evidence-Based Practice
Understanding equipment principles supports evidence-based clinical decisions.
Syringes: Essential Medical Equipment
Memory Aid: SYRINGE Components
- S – Shaft (barrel)
- Y – Yielding plunger
- R – Rubber stopper
- I – Injection tip
- N – Needle hub connection
- G – Graduated markings
- E – End cap (safety)
Anatomy of Medical Equipment: Syringe Components
Primary Components
Barrel (Shaft)
The cylindrical chamber that holds the medication. Made from clear plastic or glass to allow visualization of contents and air bubbles.
Plunger
The movable component that creates pressure to draw up or expel medication. Features a rubber stopper for airtight seal.
Tip
The connection point for needles, available in Luer-Lok or slip-tip designs for secure needle attachment.
Safety Features
Safety Cap
Protects the sterile tip before use and prevents contamination during storage and transport.
Graduated Scale
Precise volume measurements marked in milliliters (mL) and sometimes units for accurate dosing.
Finger Grips
Textured areas on the barrel for secure handling and improved control during medication administration.
Types of Medical Equipment: Syringe Classification
| Syringe Type | Volume Range | Primary Use | Key Features |
|---|---|---|---|
| Insulin Syringes | 0.3-1.0 mL | Diabetes management | Ultra-fine needles, unit markings |
| Tuberculin Syringes | 1.0 mL | Intradermal injections | Precise measurements, fine graduations |
| Standard Syringes | 3-10 mL | General injections | Versatile, Luer-Lok compatibility |
| Large Volume Syringes | 20-60 mL | Irrigation, feeding | Catheter tip, high volume capacity |
| Safety Syringes | 1-10 mL | All applications | Retractable needles, safety shields |
Critical Safety Considerations
- • Never recap needles using the two-handed technique
- • Always check syringe integrity before use
- • Verify medication compatibility with syringe materials
- • Dispose of medical equipment in appropriate sharps containers
- • Use single-use syringes only once to prevent cross-contamination
Needles: Precision Medical Equipment
Memory Aid: NEEDLE Selection Criteria
- N – Need (clinical indication)
- E – Evaluation of patient factors
- E – Examination of medication viscosity
- D – Determination of injection site
- L – Length consideration
- E – External gauge selection
Understanding Medical Equipment: Needle Specifications
Gauge System
The gauge system measures needle diameter inversely – larger gauge numbers indicate smaller needle diameters. This counterintuitive system is crucial for medical equipment selection.
18-19 Gauge: Large diameter, blood donation, rapid fluid administration
20-22 Gauge: Medium diameter, intramuscular injections, general use
23-25 Gauge: Small diameter, subcutaneous injections, pediatrics
26-30 Gauge: Very fine, insulin injections, intradermal use
Length Specifications
Needle length determines injection depth and is critical for reaching the intended tissue layer. Proper length selection ensures effective medication delivery.
⅜ inch (10mm): Intradermal injections, tuberculin testing
½ – ⅝ inch (13-16mm): Subcutaneous injections, insulin, heparin
1 – 1½ inch (25-38mm): Intramuscular injections, standard adults
2 – 3 inch (50-76mm): Deep intramuscular, specialized procedures
Clinical Selection of Medical Equipment: Needle Guide
| Injection Type | Recommended Gauge | Typical Length | Color Code | Clinical Notes |
|---|---|---|---|---|
| Intradermal | 26-27G | ⅜ – ½ inch | Gray/Clear | Tuberculin testing, allergy testing |
| Subcutaneous | 25-27G | ⅝ inch | Orange | Insulin, heparin, vaccines |
| Intramuscular (Adult) | 21-23G | 1-1½ inch | Green/Blue | Vaccines, antibiotics |
| Intramuscular (Pediatric) | 22-25G | ⅝-1 inch | Blue | Age-appropriate sizing |
| Intravenous | 18-22G | 1-1½ inch | Pink/Blue | Blood draws, IV access |
Advanced Needle Technology in Medical Equipment
Safety-Engineered Needles
- • Retractable needles that withdraw into the syringe
- • Safety shields that cover the needle after use
- • Blunt-tip needles for medication preparation
- • Self-sheathing mechanisms for automatic protection
Specialized Needle Designs
- • Butterfly needles for difficult venous access
- • Huber needles for port access
- • Filter needles for medication preparation
- • Pen needles for insulin delivery systems
Cannulas: Critical Medical Equipment for Vascular Access
Memory Aid: CANNULA Components
- C – Catheter (flexible tube)
- A – Access needle (stylet)
- N – Needle guard/safety
- N – Needle hub
- U – Universal connector
- L – Luer connector
- A – Adhesive wings
Anatomy of Medical Equipment: Cannula Structure
Catheter
The flexible, biocompatible tube that remains in the vein after insertion. Made from materials like polyurethane or silicone for patient comfort.
- • Radiopaque stripe for X-ray visibility
- • Smooth surface to minimize thrombosis
- • Color-coded for gauge identification
Stylet/Needle
The sharp metal needle that facilitates initial venipuncture and is removed after catheter placement.
- • Beveled tip for smooth insertion
- • Safety mechanism prevents needlestick
- • Precise length for optimal insertion
Hub & Wings
Connection point for IV tubing with stabilization wings for secure patient attachment.
- • Luer-compatible connections
- • Flexible wings for comfort
- • Clear hub for blood flashback visibility
Types and Sizes of Medical Equipment: Cannula Classification
| Gauge | Color | External Diameter | Flow Rate | Clinical Use | Patient Population |
|---|---|---|---|---|---|
| 14G | Orange | 2.1mm | 270 mL/min | Trauma, surgery, blood transfusion | Adult emergency |
| 16G | Gray | 1.7mm | 180 mL/min | Surgery, rapid fluid replacement | Adult |
| 18G | Green | 1.3mm | 90 mL/min | Blood transfusion, general surgery | Adult |
| 20G | Pink | 1.0mm | 54 mL/min | Routine IV therapy, medications | Adult, elderly |
| 22G | Blue | 0.8mm | 31 mL/min | Routine medications, pediatrics | Elderly, pediatric |
| 24G | Yellow | 0.7mm | 20 mL/min | Fragile veins, neonates | Neonatal, fragile veins |
Selection Criteria for Medical Equipment
-
Patient Factors: Age, vein condition, mobility, treatment duration
-
Treatment Requirements: Medication viscosity, infusion rate, compatibility
-
Duration: Short-term vs. long-term access needs
-
Clinical Urgency: Emergency vs. routine procedures
Insertion Best Practices
-
Sterile Technique: Hand hygiene, gloves, aseptic preparation
-
Vein Assessment: Palpation, visualization, optimal site selection
-
Insertion Angle: 15-30 degrees for optimal success rate
-
Confirmation: Blood flashback, easy flushing, patient comfort
Infusion Sets: Essential Medical Equipment for Fluid Delivery
Memory Aid: INFUSION Set Components
- I – IV bag connector spike
- N – Non-vented drip chamber
- F – Flow control clamp
- U – Uniform tubing
- S – Secondary ports
- I – Injection sites
- O – Output connector
- N – Needle-free connectors
Components of Medical Equipment: Infusion Set Assembly
Spike
Sterile connector that pierces IV bag septum for fluid access
Drip Chamber
Transparent chamber for visualizing and counting drip rate
Flow Clamp
Adjustable mechanism to control infusion rate
Connector
Luer-compatible connection for cannula attachment
Types of Medical Equipment: Infusion Set Varieties
Macrodrip Sets
Drop Factor: 10, 15, or 20 drops/mL
Applications: Rapid fluid replacement, blood transfusions
Advantages: Fast flow rates, large volume delivery
Typical Use: Adult patients requiring high-volume infusions
Clinical Tip: Ideal for emergency situations requiring rapid fluid resuscitation
Microdrip Sets
Drop Factor: 60 drops/mL
Applications: Precise medication delivery, pediatrics
Advantages: Accurate small volume control
Typical Use: Pediatric patients, elderly, critical medications
Clinical Tip: Essential for medications requiring precise dosing control
Filtered Sets
- • 0.2 micron filters for particulate removal
- • Essential for chemotherapy administration
- • Prevents air embolism
- • Required for certain high-risk medications
Y-Type Sets
- • Dual spike configuration
- • Allows blood component mixing
- • Built-in filters
- • Specialized for transfusion therapy
Pump-Compatible Sets
- • Specific tubing diameter
- • Anti-free-flow protection
- • Pressure-rated construction
- • Designed for infusion pumps
Medical Equipment Calculation: Flow Rate Formula
Basic Formula
Flow Rate = (Volume × Drop Factor) ÷ (Time in minutes)
Expressed as drops per minute (gtts/min)
Practical Example
Given:
- • 1000 mL Normal Saline
- • Infuse over 8 hours
- • 15 gtts/mL drip set
Calculation:
(1000 × 15) ÷ 480 min = 31 gtts/min
Safety Protocols for Medical Equipment
Memory Aid: SAFETY Protocol
- S – Sterile technique maintenance
- A – Aseptic handling procedures
- F – Five rights verification
- E – Equipment integrity check
- T – Time-based monitoring
- Y – Yearly competency validation
Critical Safety Measures
-
Hand Hygiene: Before and after handling all medical equipment
-
Visual Inspection: Check medical equipment integrity before use
-
Expiration Dates: Verify all medical equipment within date limits
-
Proper Disposal: Use appropriate containers for contaminated medical equipment
Quality Assurance
-
Two-Person Verification: High-risk medications and procedures
-
Documentation: Record medical equipment usage and patient response
-
Incident Reporting: Report medical equipment failures or complications
-
Continuing Education: Stay updated on medical equipment innovations
Infection Prevention with Medical Equipment
Before Use
- • Perform hand hygiene
- • Check medical equipment packaging
- • Verify sterility indicators
- • Inspect for damage
- • Gather all necessary supplies
During Use
- • Maintain sterile field
- • Use aseptic technique
- • Avoid contamination
- • Monitor for complications
- • Document procedure
After Use
- • Dispose medical equipment safely
- • Clean work area
- • Remove gloves properly
- • Perform hand hygiene
- • Complete documentation
Clinical Applications of Medical Equipment
Emergency Medicine Applications
Trauma Resuscitation
Medical Equipment: 14-16G cannulas, large-bore infusion sets
Rationale: Rapid volume replacement requires high-flow capability
Medication Administration
Medical Equipment: Safety syringes, various needle gauges
Rationale: Emergency medications require precise, rapid delivery
Pediatric Considerations
Size Specifications
Medical Equipment: 22-24G cannulas, microdrip sets
Rationale: Smaller vessels require specialized medical equipment
Safety Features
Medical Equipment: Safety-engineered devices, shorter needles
Rationale: Enhanced safety for active pediatric patients
Specialty Medical Equipment Applications
Oncology Care
- • Central line compatible medical equipment
- • Filtered infusion sets for chemotherapy
- • Safety needles for hazardous drugs
- • Specialized disposal protocols
Critical Care
- • Multiple lumen access medical equipment
- • Pressure-monitoring compatible sets
- • High-flow medical equipment for resuscitation
- • Continuous infusion systems
Surgical Services
- • Sterile, single-use medical equipment
- • Rapid infusion capabilities
- • Blood-compatible medical equipment
- • Anesthesia-compatible systems
Medical Equipment Selection Framework
Clinical Assessment
- • Patient age and weight
- • Vascular access quality
- • Treatment duration
- • Medication characteristics
- • Emergency vs. routine care
Medical Equipment Factors
- • Flow rate requirements
- • Compatibility considerations
- • Safety features needed
- • Cost-effectiveness
- • Availability and accessibility
Global Best Practices in Medical Equipment Usage
United States – CDC Guidelines
Safe Injection Practices: The CDC emphasizes single-use medical equipment protocols to prevent healthcare-associated infections.
- • One needle, one syringe, one patient policy
- • Proper medical equipment disposal protocols
- • Staff education on medical equipment safety
- • Regular auditing of medical equipment practices
Canada – Health Canada Standards
Quality Assurance: Comprehensive medical equipment validation and monitoring systems ensure optimal patient outcomes.
- • Rigorous medical equipment testing protocols
- • Standardized nursing competency validation
- • Integration of medical equipment safety in education
- • Provincial medical equipment quality initiatives
European Union – EMA Regulations
Standardized Medical Equipment: EU-wide standards ensure consistent medical equipment quality and safety across member nations.
- • Harmonized medical equipment specifications
- • Cross-border medical equipment recognition
- • Unified training standards for medical equipment
- • Centralized medical equipment surveillance
Singapore – Advanced Practices
Technology Integration: Leading adoption of smart medical equipment and digital monitoring systems in healthcare.
- • RFID-enabled medical equipment tracking
- • Automated medical equipment inventory systems
- • AI-assisted medical equipment selection
- • Real-time medical equipment usage analytics
Innovative Medical Equipment Practices Worldwide
Smart Medical Equipment
- • RFID tracking systems
- • Bluetooth-enabled monitoring
- • Automated expiration alerts
- • Usage pattern analytics
Sustainability Initiatives
- • Eco-friendly medical equipment materials
- • Reduced packaging waste
- • Recycling programs
- • Carbon footprint reduction
Training Excellence
- • Virtual reality medical equipment training
- • Competency-based assessments
- • Peer learning networks
- • Continuous improvement culture
Key Takeaways for Medical Equipment Mastery
Essential Points to Remember
- • Medical equipment selection directly impacts patient safety and treatment outcomes
- • Understanding the relationship between gauge, length, and flow rate optimizes medical equipment usage
- • Proper handling and disposal of medical equipment prevents healthcare-associated infections
- • Continuous education on medical equipment innovations enhances professional competence
- • Global best practices provide frameworks for excellence in medical equipment utilization
Mastering medical equipment – including syringes, needles, cannulas, and infusion sets – is fundamental to safe, effective nursing practice. This comprehensive guide provides the foundation for confident, competent use of essential medical equipment in various clinical settings.
Remember that proficiency with medical equipment comes through practice, continuing education, and commitment to patient safety. Stay updated on innovations in medical equipment technology and maintain the highest standards of clinical practice.
