Unlock Flawless Skin & Mucous Membrane Application in Indian Nursing!
Master the Art of Topical Medication Administration with Expert Techniques and Safety Protocols
Table of Contents
Professional Topical Medication Administration Techniques
Introduction to Topical Administration
What Makes Topical Administration Special?
Topical administration represents a cornerstone of modern nursing practice, offering direct drug delivery to specific body areas while minimizing systemic exposure. This localized approach enhances therapeutic effectiveness while reducing potential side effects, making it an essential skill for every nursing professional in India.
Key Advantages
- Direct targeted action
- Reduced systemic side effects
- Patient-friendly application
- Cost-effective treatment
Clinical Applications
- Dermatological conditions
- Pain management
- Infection control
- Wound care
Critical Success Factors
Effective topical administration depends on proper technique, appropriate medication selection, correct site preparation, and thorough patient education. Each step requires careful attention to detail and adherence to evidence-based protocols to ensure optimal therapeutic outcomes and patient safety.
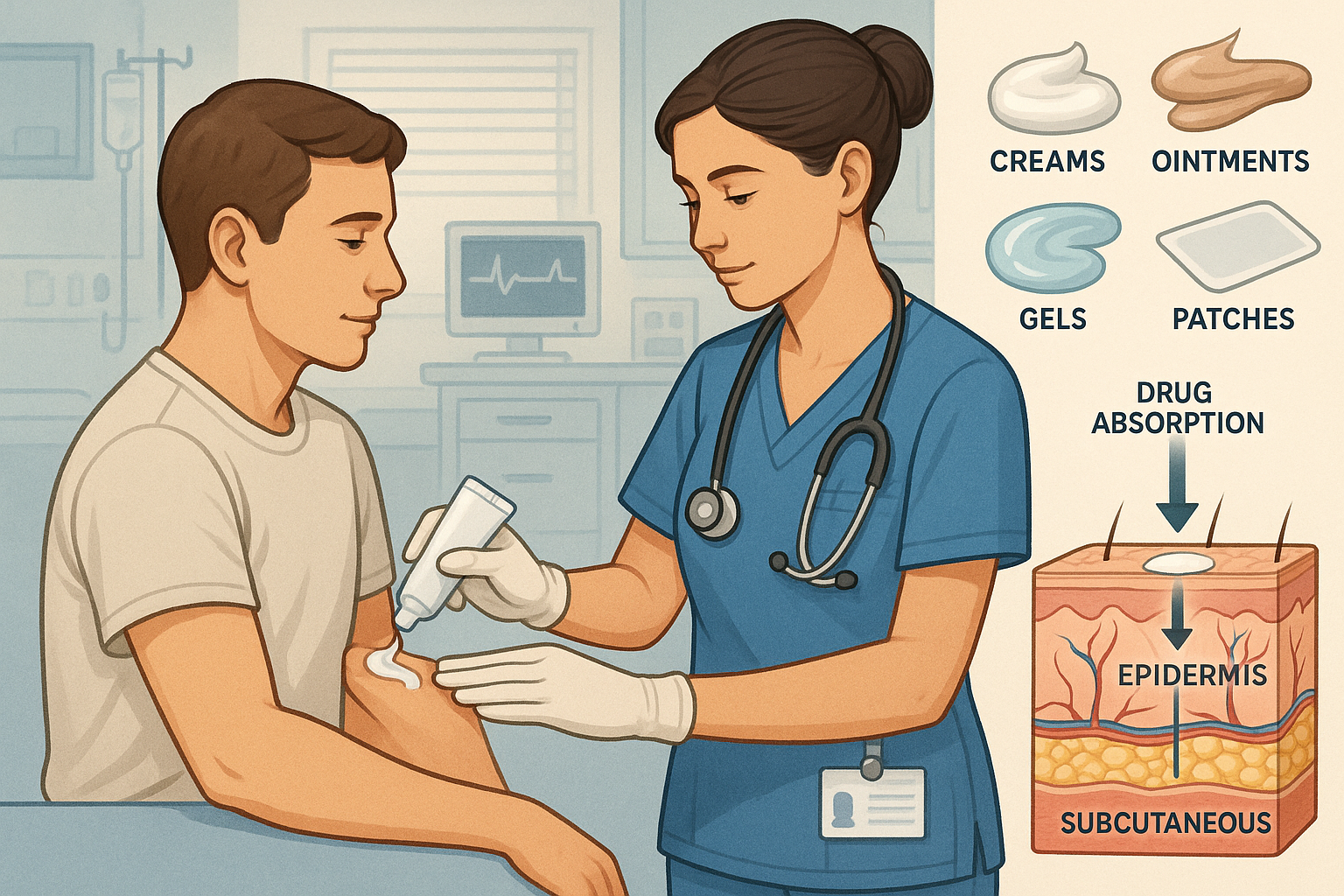
Understanding Skin & Mucous Membrane Anatomy
Skin Structure Layers
Epidermis (Outer Layer)
Primary barrier; controls medication penetration
Dermis (Middle Layer)
Contains blood vessels; main absorption site
Hypodermis (Deep Layer)
Fat storage; systemic circulation entry
Mucous Membrane Characteristics
- Highly vascularized tissue
- Rapid drug absorption
- Sensitive to irritation
- Requires gentle handling
| Site | Absorption Rate | Characteristics |
|---|---|---|
| Forearm | 1.0 (baseline) | Standard reference site |
| Face | 13.0 | High absorption, delicate |
| Scalp | 3.5 | Hair follicle penetration |
| Palm | 0.8 | Thick stratum corneum |
| Genital Area | 42.0 | Highest absorption rate |
Memory Aid: “SAFE”
Skin integrity assessment
Absorption rate consideration
Factor in patient comfort
Evaluate for allergic reactions
Clinical Correlation
Understanding anatomical variations in drug absorption is crucial for safe topical administration. Areas with thinner stratum corneum or higher vascularity require modified dosing and increased monitoring. This knowledge helps nurses optimize therapeutic outcomes while preventing adverse reactions through appropriate site selection and application techniques.
Types of Topical Medications
Liquid Formulations
Solutions
Clear, homogeneous mixtures
Example: Calamine lotion
Suspensions
Particles dispersed in liquid
Example: Zinc oxide shake lotion
Semi-solid Forms
Ointments
Greasy, occlusive base
Best for dry, scaling conditions
Creams
Oil-in-water emulsion
Cosmetically acceptable
Gels
Clear, non-greasy
Rapid absorption
Specialized Systems
Transdermal Patches
Controlled drug release
Example: Nicotine, pain patches
Sprays & Aerosols
Easy application
Ideal for large areas
Specialized Mucous Membrane Applications
Ophthalmic Preparations
- Eye drops: aqueous solutions
- Eye ointments: longer contact time
- Gel formulations: sustained release
Otic Applications
- Ear drops: infection treatment
- Irrigation solutions: wax removal
- Powder insufflations: dry conditions
Nasal Preparations
- Sprays: systemic absorption
- Drops: localized treatment
- Inhalers: respiratory conditions
Vaginal & Rectal
- Suppositories: solid dosage forms
- Creams: local treatment
- Tablets: vaginal infections
Formulation Selection Mnemonic: “COPS”
Condition of the skin (dry vs. moist)
Occlusive properties needed
Patient preference and compliance
Site of application requirements
Mastering Application Techniques
Universal Pre-Application Protocol
Hand hygiene and PPE donning
Patient identification verification
Medication rights confirmation
Site assessment and preparation
Patient education and consent
Equipment and supply preparation
Topical Skin Application
Gentle Spreading Technique
- • Apply small amount to clean fingertip
- • Use gentle circular motions
- • Work from center outward
- • Avoid excessive rubbing
Dosage Guidelines
- • Fingertip unit measurement
- • Thin, even layer application
- • Cover entire affected area
- • Extend slightly beyond margins
Ophthalmic Administration
Step-by-Step Process
- Position patient supine or seated
- Gently pull lower eyelid downward
- Instill drops into conjunctival sac
- Avoid touching eye with dropper
- Apply gentle pressure to lacrimal sac
- Instruct patient to close eyes gently
Otic Administration
Adult Technique
- • Pull pinna up and back
- • Direct drops toward ear canal wall
- • Gentle massage of tragus
- • Maintain position for 2-3 minutes
Pediatric Considerations
- • Pull pinna down and back
- • Use restraint if necessary
- • Warmer drops for comfort
- • Parent involvement encouraged
Administration Memory Aid: “CLEAN”
Clean the application site
Load appropriate amount
Evenly distribute medication
Assess patient response
Note administration details
Transdermal Patch Application Excellence
Site Selection
- • Clean, dry, intact skin
- • Minimal hair coverage
- • Avoid bony prominences
- • Rotate application sites
Application Process
- • Remove backing carefully
- • Apply with firm pressure
- • Hold for 30 seconds
- • Check adherence edges
Monitoring Points
- • Date and time application
- • Document site location
- • Assess for skin irritation
- • Monitor therapeutic effect
Critical Safety Reminders
Never Compromise On:
- • Aseptic technique maintenance
- • Patient comfort and dignity
- • Proper dosage measurement
- • Complete documentation
Always Monitor For:
- • Allergic reactions
- • Local skin irritation
- • Therapeutic effectiveness
- • Systemic absorption effects
Strategic Administration Sites Selection
Site Selection Principles
Assess Integrity
Evaluate skin condition, barriers, and healing status
Rotate Locations
Prevent sensitization and tissue damage
Consider Patient
Age, mobility, and comfort preferences
| Application Site | Absorption Rate | Best For | Special Considerations | Avoid If |
|---|---|---|---|---|
|
Forearm (Flexor)
|
Moderate | Patches, routine creams | Good accessibility, patient comfort | Broken skin, rash |
|
Upper Arm
|
Moderate-High | Hormone patches, vaccines | Less visible, good adherence | Excessive hair, scars |
|
Chest
|
High | Cardiac medications, pain patches | Large surface area, good circulation | Breast tissue, excessive hair |
|
Behind Ear
|
Very High | Motion sickness patches | Thin skin, good absorption | Ear infections, hearing aids |
|
Thigh
|
Moderate | Large patches, creams | Large surface area, privacy | Tight clothing, excessive movement |
Ocular Administration Sites
Lower Conjunctival Sac
- • Primary site for eye drops
- • Natural medication reservoir
- • Minimizes systemic absorption
- • Reduces corneal irritation
Inner Canthus Considerations
- • Lacrimal puncta location
- • Digital pressure application
- • Prevents systemic drainage
- • Enhances local effectiveness
Nasal Cavity Zones
Anterior Nares
- • Easy access for drops
- • Good for local treatment
- • Patient self-administration
- • Minimal systemic absorption
Middle Meatus
- • Optimal spray targeting
- • Rich vascular supply
- • Systemic medication delivery
- • Hormone administration site
Site Selection Mnemonic: “RAPIR”
Rotate sites regularly
Assess skin integrity
Patient comfort priority
Infection risk evaluation
Respect patient preferences
Clinical Wisdom for Indian Practice
In tropical climates like India, consider increased perspiration affecting patch adherence and medication stability. Higher ambient temperatures may accelerate drug release from transdermal systems, requiring enhanced monitoring for therapeutic and adverse effects. Cultural preferences for covering certain body areas should guide respectful site selection while maintaining clinical effectiveness.
Regular site rotation becomes even more critical in hot, humid conditions to prevent skin maceration and fungal overgrowth. Documentation of administration sites should include environmental factors that might influence drug absorption and patient response.
Safety Protocols & Risk Management
Critical Safety Framework
Safe topical administration requires systematic risk assessment, adherence to evidence-based protocols, and continuous patient monitoring. Every step of the administration process must prioritize patient safety while maximizing therapeutic outcomes through careful attention to detail and professional competence.
Safety Hierarchy of Controls
Engineering Controls
Proper ventilation, lighting, ergonomic setup
Administrative Controls
Policies, training, competency validation
Personal Protection
Gloves, gowns, eye protection
High-Risk Scenarios
Patient-Related Risks
- • Compromised skin integrity
- • Multiple drug allergies
- • Immunocompromised status
- • Pediatric or geriatric patients
- • Pregnancy or lactation
Medication-Related Risks
- • High-potency corticosteroids
- • Cytotoxic agents
- • Sensitizing compounds
- • Concentration variations
- • Expired or damaged products
Personal Protective Equipment
Standard Precautions
Nitrile gloves, hand hygiene, avoid contamination
Enhanced Protection
Gowns for messy applications, eye protection for sprays
Specialized Requirements
Chemotherapy drugs: double gloves, impervious gown
Verification Protocols
Five Rights Plus
- ✓ Right patient identification
- ✓ Right medication verification
- ✓ Right dose calculation
- ✓ Right route confirmation
- ✓ Right time scheduling
- ✓ Right documentation
- ✓ Right to refuse
Double-Check Requirements
- • High-alert medications
- • Pediatric calculations
- • First-time administrations
- • Complex preparations
Safety Mnemonic: “SCARED”
Skin assessment before application
Check allergies and contraindications
Aseptic technique maintenance
Right dose and concentration
Evaluate patient response
Document thoroughly
Adverse Reaction Management Protocol
Recognition
- • Local irritation signs
- • Contact dermatitis
- • Allergic responses
- • Systemic symptoms
- • Worsening condition
Immediate Action
- • Discontinue medication
- • Gentle site cleansing
- • Vital sign assessment
- • Physician notification
- • Emergency protocols
Documentation
- • Reaction description
- • Timeline of events
- • Interventions provided
- • Patient response
- • Follow-up plans
Infection Prevention Strategies
Hand Hygiene Excellence
20-second wash or alcohol-based sanitizer before and after each patient contact
Medication Integrity
Single-use containers, proper storage, contamination prevention
Equipment Sterilization
Clean applicators, sterile technique for open wounds
Quality Assurance Measures
Regular Audits
Technique observation, competency assessment, outcome evaluation
Continuous Education
Regular training updates, new technique integration, evidence-based practice
Outcome Monitoring
Patient satisfaction, adverse events tracking, improvement initiatives
Cultural Competency in Safety
In diverse Indian healthcare settings, safety protocols must accommodate cultural preferences and religious practices. Respect patient modesty requirements during topical administration, especially when treating areas typically covered by traditional clothing. Language barriers may affect safety communication – utilize translators or visual aids to ensure proper understanding of administration instructions and adverse reaction recognition.
Consider cultural attitudes toward pain expression and medication acceptance when monitoring patient responses. Some patients may underreport discomfort or side effects due to cultural norms, requiring enhanced observational skills and gentle encouragement for honest communication about treatment effects.
Essential Equipment & Supply Management
Comprehensive Supply Checklist
Proper equipment selection and management are fundamental to safe and effective topical administration. Every nursing unit should maintain standardized supplies, ensure proper storage conditions, and implement systematic inventory management to support consistent, high-quality patient care delivery.
Application Tools
Primary Applicators
- • Cotton-tipped swabs
- • Tongue depressors
- • Gauze squares (2×2, 4×4)
- • Disposable spatulas
Specialized Tools
- • Medicine droppers
- • Irrigation syringes
- • Measuring spoons
- • Application brushes
Protective Equipment
Standard Protection
- • Nitrile examination gloves
- • Disposable aprons/gowns
- • Face shields (for sprays)
- • Hair covers (when needed)
Enhanced Protection
- • Double-layer gloves
- • Impervious sleeves
- • Respiratory protection
- • Closed-system devices
Storage Solutions
Environmental Control
- • Refrigerated storage units
- • Controlled room temperature
- • Humidity monitoring
- • Light-resistant containers
Organization Systems
- • Labeled medication carts
- • Secure storage cabinets
- • First-in-first-out rotation
- • Emergency supply kits
| Equipment Category | Specific Items | Primary Use | Special Requirements | Replacement Frequency |
|---|---|---|---|---|
|
Ophthalmic
|
Sterile droppers, eye cups, irrigation bottles | Eye medication delivery | Sterile, single-use preferred | After each patient |
|
Otic
|
Ear droppers, bulb syringes, otoscope | Ear canal medication | Warm to body temperature | Daily cleaning required |
|
Respiratory
|
Nebulizers, inhalers, spacer devices | Respiratory medication delivery | Regular calibration needed | Per manufacturer guidelines |
|
Dermal
|
Applicator sticks, measuring devices, scissors | Skin surface application | Non-contaminating materials | Single use or sterilized |
|
Environmental
|
Thermometers, hygrometers, timers | Condition monitoring | Regular calibration essential | Annual or per protocol |
Maintenance Protocols
Daily Checks
- • Equipment functionality testing
- • Cleanliness verification
- • Supply level assessment
- • Expiration date monitoring
Weekly Reviews
- • Inventory rotation procedures
- • Storage condition validation
- • Equipment calibration checks
- • Waste disposal protocols
Sustainable Practices
Waste Reduction
- • Accurate usage calculations
- • Reusable equipment preference
- • Bulk purchasing strategies
- • Energy-efficient storage
Cost Optimization
- • Generic equivalent utilization
- • Volume-based negotiations
- • Preventive maintenance programs
- • Staff training investments
Equipment Management Mnemonic: “SECURE”
Standardized supply protocols
Environmental control systems
Cleanliness maintenance standards
Utilization tracking methods
Regular inspection schedules
Emergency backup supplies
Technology Integration Opportunities
Modern healthcare facilities increasingly utilize technology to enhance topical administration efficiency and safety. Automated dispensing systems reduce medication errors, while electronic tracking systems monitor expiration dates and usage patterns. Smart storage solutions maintain optimal environmental conditions and alert staff to temperature excursions or inventory shortages.
Consider implementing barcode scanning for medication verification, mobile documentation systems for bedside charting, and integrated communication platforms for rapid consultation with pharmacy and medical staff. These technological advances support evidence-based practice while reducing administrative burden on nursing staff.
International Best Practices in Topical Administration
Excellence Through Global Learning
Healthcare systems worldwide have developed innovative approaches to topical medication administration that can enhance nursing practice in India. By adopting proven international standards while respecting local culture and resource constraints, Indian nurses can deliver world-class care that meets global benchmarks for safety, efficacy, and patient satisfaction.
Nordic Model Excellence
Evidence-Based Protocols
Scandinavian countries implement rigorous, research-driven protocols for topical administration. Every procedure is backed by current scientific evidence, with regular protocol updates based on emerging research findings. This systematic approach ensures consistent, high-quality care delivery across all healthcare facilities.
Patient-Centered Care
Nordic healthcare emphasizes shared decision-making and patient education. Patients receive comprehensive information about their topical medications, including expected outcomes, potential side effects, and self-administration techniques. This approach improves adherence and empowers patients as active partners in their care.
Canadian Safety Standards
Accreditation Excellence
Canadian healthcare facilities maintain strict accreditation standards for medication administration. Regular audits, competency assessments, and quality improvement initiatives ensure that nursing staff demonstrate consistent proficiency in topical administration techniques.
Cultural Competency Integration
Canadian nursing practice recognizes diverse cultural backgrounds and adapts care delivery accordingly. This includes respecting religious requirements, language preferences, and traditional healing practices while maintaining evidence-based medical standards.
Japanese Precision Medicine
Meticulous Documentation
Japanese healthcare systems maintain extraordinarily detailed documentation for all medication administrations. This includes precise timing, exact dosages, patient positioning, and immediate responses. Such thorough records enable pattern recognition and continuous quality improvement.
Technology Integration
Japanese hospitals extensively utilize technology to enhance safety and efficiency. Robotic dispensing systems, electronic monitoring devices, and AI-assisted decision support tools reduce errors while providing real-time guidance to nursing staff during medication administration.
Global Excellence Mnemonic: “WORLD”
Worldwide evidence integration
Organizational learning culture
Respect for cultural diversity
Leadership in innovation
Dedication to continuous improvement
Implementation Roadmap for Indian Healthcare
Phase 1: Foundation
- • Standardize basic protocols
- • Establish training programs
- • Implement safety measures
- • Begin data collection
- • Create quality metrics
Phase 2: Enhancement
- • Integrate technology solutions
- • Develop cultural adaptations
- • Expand specialized training
- • Implement outcome tracking
- • Foster innovation culture
Phase 3: Excellence
- • Achieve international standards
- • Share best practices globally
- • Lead research initiatives
- • Mentor other healthcare systems
- • Maintain continuous improvement
Australian Innovation Model
Clinical Practice Improvement
Australian nursing councils emphasize continuous professional development with mandatory annual competency assessments for topical administration. Nurses must demonstrate proficiency in new techniques and technologies to maintain their practice credentials.
Patient Advocacy Excellence
Strong patient advocacy programs ensure that nurses actively represent patient interests during medication decisions. This includes advocating for appropriate formulation choices, application schedules, and comfort measures during treatment.
Dutch Collaborative Care
Interprofessional Teams
Dutch healthcare utilizes integrated teams where nurses, pharmacists, and physicians collaborate closely on topical medication decisions. Regular team meetings ensure optimal treatment selection and monitoring protocols for each patient.
Community Integration
Seamless transitions between hospital and community care ensure continuous topical medication management. Community nurses receive the same training standards and have access to hospital-based consultation for complex cases.
Adapting Global Excellence for Indian Healthcare
Cultural Adaptations
- Incorporate traditional healing wisdom where evidence-based
- Respect religious and cultural practices during treatment
- Develop multilingual patient education materials
- Train staff in cultural competency and sensitivity
Resource Optimization
- Cost-effective technology solutions for resource-limited settings
- Scalable training programs for large nursing populations
- Leverage mobile technology for rural healthcare delivery
- Public-private partnerships for sustainable improvement
“By thoughtfully integrating global best practices with Indian healthcare values and constraints, nursing professionals can achieve excellence that serves patients effectively while honoring cultural traditions and working within available resources.”
Mastering Topical Administration Excellence
Through comprehensive understanding of anatomical principles, evidence-based techniques, and patient-centered care approaches, nursing professionals in India can deliver exceptional topical medication administration that meets international standards while serving diverse patient populations with cultural sensitivity and clinical expertise.
Excellence Achieved
Through systematic learning and practice
Patient Care Enhanced
With safe, effective medication delivery
Global Standards Met
While honoring local culture and values
Continue Your Professional Journey
Master these techniques, practice with precision, and become the skilled nursing professional that patients trust and colleagues respect. Your dedication to topical administration excellence contributes to better health outcomes for the communities you serve.
