Specialized Medication Administration Routes
Master the Art of Eye, Ear, Bladder, Vaginal, and Rectal Medication Administration for Safe and Effective Patient Care
Understanding Specialized Administration Routes
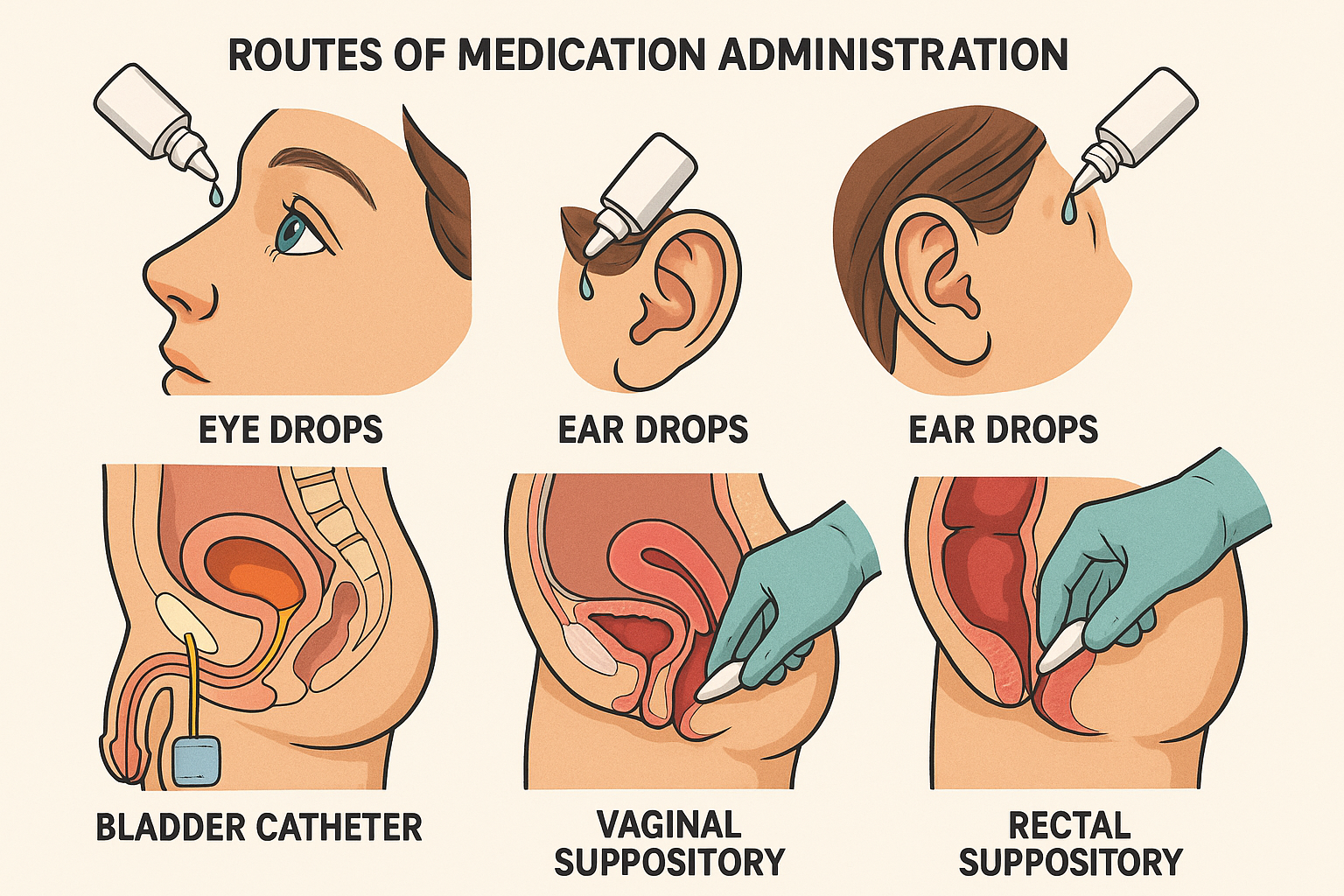
Welcome to the comprehensive guide on specialized-routes of medication administration! As nursing professionals, mastering these techniques is crucial for providing optimal patient care across diverse clinical scenarios. This guide covers five critical administration pathways that every competent nurse must understand.
Ophthalmic Route
Direct application to the eye for localized treatment of ocular conditions and infections.
Otic Route
Ear canal administration for treating infections, inflammation, and cerumen impaction.
Intravesical Route
Direct bladder instillation for urological conditions and localized cancer treatment.
Vaginal Route
Intravaginal medication delivery for gynecological conditions and hormone replacement.
Rectal Route
Per rectum administration when oral route is compromised or for localized treatment.
Safety First
Evidence-based practices ensuring patient safety and therapeutic effectiveness.
Fundamental Principles of Specialized-Routes Administration
Sterile Technique
Maintain asepsis to prevent healthcare-associated infections
Patient Positioning
Optimal positioning enhances medication absorption and patient comfort
Timing Considerations
Understand absorption rates and therapeutic windows for maximum efficacy
Contraindication Awareness
Identify absolute and relative contraindications before administration
Patient Assessment
Comprehensive evaluation before, during, and after medication administration
Documentation Standards
Accurate recording of administration details and patient responses
Ophthalmic Medication Administration
Understanding the Ophthalmic Route
The ophthalmic route delivers medications directly to ocular structures, providing localized therapeutic effects while minimizing systemic absorption. This specialized-routes approach is essential for treating conditions such as glaucoma, conjunctivitis, corneal ulcers, and post-surgical inflammation.
Common Formulations
- Drops (Solutions): Most common, rapid onset
- Ointments: Longer contact time, sustained release
- Gels: Improved retention, reduced frequency
- Inserts: Extended-release systems
Anatomy Review
Key Structures
Anterior Segment
- • Cornea
- • Anterior chamber
- • Iris
- • Lens
Supporting Structures
- • Conjunctiva
- • Lacrimal system
- • Eyelids
- • Sclera
Step-by-Step Eye Drop Administration
Preparation
- • Verify patient identity
- • Check medication orders
- • Gather sterile supplies
- • Perform hand hygiene
Positioning
- • Patient supine or seated
- • Head tilted backward
- • Affected eye accessible
- • Ensure comfort
Cleansing
- • Clean from inner to outer canthus
- • Use sterile saline or water
- • Remove discharge/debris
- • Pat dry gently
Drop Installation
- • Shake medication if required
- • Pull down lower eyelid
- • Create conjunctival sac
- • Hold dropper 1-2cm above eye
Administration
- • Release prescribed number of drops
- • Aim for conjunctival sac
- • Avoid touching eye with dropper
- • Release eyelid gently
Post-Administration
- • Patient closes eyes gently
- • Apply nasolacrimal occlusion
- • Wipe excess medication
- • Monitor for reactions
Memory Aid: DROPS Method
Critical Safety Points
Infection Prevention
- • Never touch dropper tip to eye or eyelashes
- • Use separate bottles for each eye if bilateral infection
- • Discard single-use containers immediately after use
- • Check expiration dates and storage requirements
Systemic Absorption
- • Apply nasolacrimal occlusion for 1-2 minutes
- • Wait 5 minutes between different eye medications
- • Monitor for systemic side effects
- • Educate patients about proper technique
Otic Medication Administration
Understanding the Otic Route
The otic route delivers medications directly to the external auditory canal and middle ear, providing targeted treatment for conditions such as otitis externa, otitis media, cerumen impaction, and fungal infections. This specialized-routes approach ensures maximum therapeutic concentration at the site of infection while minimizing systemic exposure.
Common Indications
- Otitis Externa: Bacterial or fungal outer ear infections
- Otitis Media: Middle ear inflammation with intact tympanic membrane
- Cerumen Removal: Softening and dissolution of earwax
- Pain Management: Analgesic drops for ear discomfort
Ear Anatomy Essentials
Anatomical Considerations
Age-Specific Administration Techniques
| Age Group | Pinna Direction | Positioning | Special Considerations |
|---|---|---|---|
| Infants (0-12 months) | Down and back | Lateral with affected ear up | Gentle restraint may be needed; parent assistance helpful |
| Toddlers (1-3 years) | Down and back | Seated on parent’s lap or lateral | Distraction techniques; ensure safety restraint |
| Children (3+ years) | Up and back | Seated or lateral position | Age-appropriate explanation; cooperation usually good |
| Adults | Up and back | Seated or lateral position | Full explanation of procedure; self-administration teaching |
Otic Drop Administration Protocol
Assessment
- • Check for cerumen impaction
- • Inspect tympanic membrane
- • Note discharge or inflammation
- • Assess pain level
Preparation
- • Warm medication to body temperature
- • Verify correct medication and dose
- • Position patient appropriately
- • Gather clean supplies
Instillation
- • Straighten ear canal appropriately
- • Insert dropper 1cm into canal
- • Instill prescribed number of drops
- • Avoid touching canal with dropper
Follow-Up
- • Patient remains on side 5-10 minutes
- • Massage tragus gently if indicated
- • Insert cotton plug if ordered
- • Monitor for adverse reactions
Memory Aid: HEAR Method
Intravesical (Bladder) Medication Administration
Understanding Intravesical Therapy
Intravesical medication administration involves direct instillation of therapeutic agents into the bladder through a urinary catheter. This specialized-routes approach provides high local drug concentrations while minimizing systemic absorption, making it ideal for treating bladder conditions, preventing recurrent urinary tract infections, and delivering chemotherapy for bladder cancer.
Clinical Applications
- Bladder Cancer: BCG therapy, chemotherapeutic agents
- Interstitial Cystitis: Dimethyl sulfoxide (DMSO), heparin
- Recurrent UTIs: Antibiotic instillation
- Bladder Irrigation: Continuous or intermittent irrigation
Critical Safety Alert
Intravesical administration requires specialized training and should only be performed by qualified healthcare professionals. Always verify bladder emptying before instillation and monitor for signs of bladder perforation or systemic absorption.
Equipment and Supplies
Required Materials
Sterile Supplies
- • Urinary catheter (usually Foley)
- • Sterile gloves
- • Antiseptic solution
- • Sterile drapes
- • Catheter insertion kit
Administration
- • Prescribed medication
- • Large syringes (50-60mL)
- • Clamps or plugs
- • Drainage bag
- • pH strips (if indicated)
Timing Considerations
- BCG therapy: Weekly for 6 weeks, then maintenance schedule
- Chemotherapy: Varies by protocol, typically weekly or monthly
- DMSO: Every 2 weeks for 4-6 treatments initially
- Retention time: Usually 1-2 hours, varies by medication
Intravesical Administration Protocol
Pre-Procedure
- • Obtain informed consent
- • Verify patient identity and allergies
- • Check medication order and expiration
- • Assess for contraindications
- • Ensure bladder is empty
- • Position patient supine
- • Perform thorough hand hygiene
Instillation Phase
- • Insert catheter using sterile technique
- • Verify catheter placement
- • Drain residual urine completely
- • Clamp catheter drainage port
- • Instill medication slowly (gravity or gentle pressure)
- • Clamp catheter after instillation
- • Position patient as ordered
Post-Procedure
- • Monitor patient during retention period
- • Assess for discomfort or adverse reactions
- • Unclamp after prescribed retention time
- • Monitor drainage characteristics
- • Remove catheter if single-dose treatment
- • Document procedure and patient response
- • Provide post-procedure instructions
Contraindications
-
Active UTI: Increased risk of systemic infection and reduced efficacy
-
Gross Hematuria: May indicate bladder trauma or malignancy
-
Bladder Trauma: Risk of perforation and medication extravasation
-
Immunosuppression: Relative contraindication for BCG therapy
Potential Complications
-
BCG Sepsis: Rare but life-threatening; monitor for fever, chills
-
Chemical Cystitis: Inflammation from medication irritation
-
Bladder Perforation: Rare; requires immediate surgical intervention
-
Allergic Reactions: Monitor for signs of hypersensitivity
Vaginal and Rectal Medication Administration
Vaginal Route Administration
Clinical Applications
- Vaginal Infections: Antifungals, antibiotics for bacterial vaginosis
- Hormone Replacement: Estrogen creams and rings
- Contraception: Spermicidal agents, vaginal rings
- Cervical Ripening: Prostaglandins for labor induction
- Vaginal Atrophy: Moisturizers and lubricants
Dosage Forms
Solid Forms
- • Suppositories
- • Tablets
- • Capsules
- • Ovules
Semi-solid/Liquid
- • Creams
- • Gels
- • Foams
- • Solutions
Vaginal Administration Steps
-
1
Explain procedure and obtain consent; ensure privacy
-
2
Position patient in lithotomy or Sims position
-
3
Perform hand hygiene and don clean gloves
-
4
Inspect external genitalia for abnormalities
-
5
Separate labia and locate vaginal opening
-
6
Insert medication using applicator or finger
-
7
Push medication high into posterior fornix
-
8
Remove applicator gently and dispose properly
-
9
Provide perineal pad to prevent staining
Rectal Route Administration
When to Use Rectal Route
- Nausea/Vomiting: When oral route is not feasible
- NPO Status: Pre/post-operative patients
- Unconscious Patients: Alternative to IV when unavailable
- Constipation: Laxatives and stool softeners
- Localized Treatment: Hemorrhoids, anal fissures
- Pediatric Use: When oral cooperation is difficult
Rectal Route Contraindications
- • Recent rectal surgery or trauma
- • Severe diarrhea or fecal impaction
- • Rectal bleeding or inflammatory bowel disease
- • Neutropenia (infection risk)
Rectal Suppository Technique
- 1. Position patient in left lateral or Sims position
- 2. Apply water-soluble lubricant to suppository
- 3. Don clean gloves and separate buttocks
- 4. Insert suppository pointed end first
- 5. Push beyond internal anal sphincter (2-4 inches)
- 6. Hold buttocks together briefly
- 7. Instruct patient to retain for 15-30 minutes
- 8. Document administration and patient response
Absorption Characteristics
Memory Aid: PLACE Method (Both Routes)
Specialized-Routes Comparison and Selection Guide
| Route | Onset Time | Absorption | Advantages | Disadvantages | Patient Factors |
|---|---|---|---|---|---|
| Ophthalmic | 5-15 minutes | Primarily local | High local concentration, minimal systemic effects | Requires cooperation, temporary vision blur | Eye anatomy, tear production, blink reflex |
| Otic | 10-20 minutes | Local with minimal systemic | Direct delivery to infection site, good penetration | Cerumen may block access, patient positioning required | Age (canal anatomy), cerumen impaction, TM integrity |
| Intravesical | 30-60 minutes | Local with variable systemic | High bladder concentration, good for cancer therapy | Invasive procedure, infection risk, specialized training | Bladder capacity, UTI status, immune function |
| Vaginal | 15-30 minutes | Local and systemic | Good absorption, sustained release, patient can self-administer | Privacy concerns, leakage, hormonal fluctuations affect pH | Menstrual cycle, vaginal infections, anatomy variations |
| Rectal | 15-30 minutes | Good systemic absorption | Alternative when oral not possible, bypasses some first-pass | Patient discomfort, variable retention, social stigma | Rectal tone, stool presence, inflammatory conditions |
Patient Education Essentials
- • Proper technique demonstration
- • Storage requirements and expiration dates
- • Expected therapeutic effects and timeline
- • Recognition of adverse reactions
- • When to contact healthcare provider
Documentation Requirements
- • Medication name, dose, route, time
- • Patient positioning and cooperation
- • Immediate patient response
- • Any adverse reactions or complications
- • Patient education provided
Quality Improvement
- • Regular competency validation
- • Patient satisfaction feedback
- • Infection rate monitoring
- • Medication error prevention
- • Evidence-based practice updates
Global Best Practices in Specialized-Routes Administration
Scandinavian Model (Norway, Sweden, Denmark)
-
Specialized Certification: Mandatory certification for intravesical therapy administration with annual competency validation
-
Two-Nurse Verification: Required double-check system for high-risk medications like chemotherapy instillations
-
Digital Documentation: Real-time electronic systems with barcode verification reduce medication errors by 40%
Japanese Healthcare System
-
Technology Integration: Smart pumps for intravesical instillations with automated pressure monitoring
-
Outcome Tracking: National database tracking infection rates and treatment outcomes for quality improvement
-
Simulation Training: Mandatory high-fidelity simulation training before clinical practice
Australian Nursing Standards
-
Cultural Competency: Specialized training for Indigenous populations with consideration for traditional healing practices
-
Community Integration: Home healthcare nurses trained in specialized-routes administration for rural/remote populations
-
Sustainability Focus: Environmentally conscious disposal protocols for medical waste from specialized administration routes
Canadian Quality Initiatives
-
Multilingual Resources: Patient education materials available in French, English, and Indigenous languages
-
Cold Chain Management: Rigorous temperature monitoring for temperature-sensitive medications during transport
-
Interprofessional Collaboration: Structured communication protocols between nurses, pharmacists, and physicians
