First Aid Management of Orthopedic Injuries
Comprehensive Nursing Notes on Fractures, Dislocations, and Muscle Injuries
Table of Contents
Orthopedic Injuries Overview
Comprehensive overview of fractures, dislocations, and muscle injuries commonly encountered in emergency care
1. Introduction and Overview
Orthopedic injuries represent one of the most common presentations in emergency departments and primary care settings. As nursing professionals, understanding the immediate assessment and first aid management of fractures, dislocations, and muscle injuries is crucial for optimal patient outcomes and preventing secondary complications.
Clinical Significance
Prompt and appropriate first aid management can significantly reduce pain, prevent further tissue damage, and improve long-term functional outcomes. Nurses are often the first healthcare providers to assess and manage these injuries, making this knowledge essential for safe practice.
Learning Objectives
Knowledge Objectives:
- Understand pathophysiology of orthopedic injuries
- Classify different types of fractures and dislocations
- Recognize signs and symptoms of muscle injuries
- Identify potential complications
Skill Objectives:
- Perform systematic injury assessment
- Apply appropriate first aid interventions
- Implement immobilization techniques
- Provide patient education and support
2. Fractures: Pathophysiology and Classification
A fracture is defined as a break in the continuity of bone tissue, typically resulting from trauma that exceeds the bone’s ability to withstand mechanical stress. Understanding fracture patterns, healing processes, and complications is fundamental to providing effective nursing care.
Pathophysiology of Fractures
When excessive force is applied to bone, it may result in microscopic or macroscopic breaks. The healing process involves several overlapping phases: inflammation, soft callus formation, hard callus formation, and remodeling. This process typically takes 6-12 weeks for complete healing, depending on factors such as age, nutrition, blood supply, and the presence of infection.
Mnemonic: FRACTURE Assessment
F – Function (loss of normal function)
R – Rotation (abnormal positioning)
A – Angulation (bone deviation from normal alignment)
C – Crepitus (grating sensation)
T – Tenderness (localized pain)
U – Unnatural movement
R – Reduced length (shortening)
E – Edema (swelling)
Fracture Classifications
By Skin Integrity
-
Closed (Simple) Fracture:
Bone is broken but skin remains intact. Lower risk of infection but internal bleeding may occur.
-
Open (Compound) Fracture:
Bone breaks through the skin or wounds penetrate to the fracture site. High risk of infection and requires immediate surgical intervention.
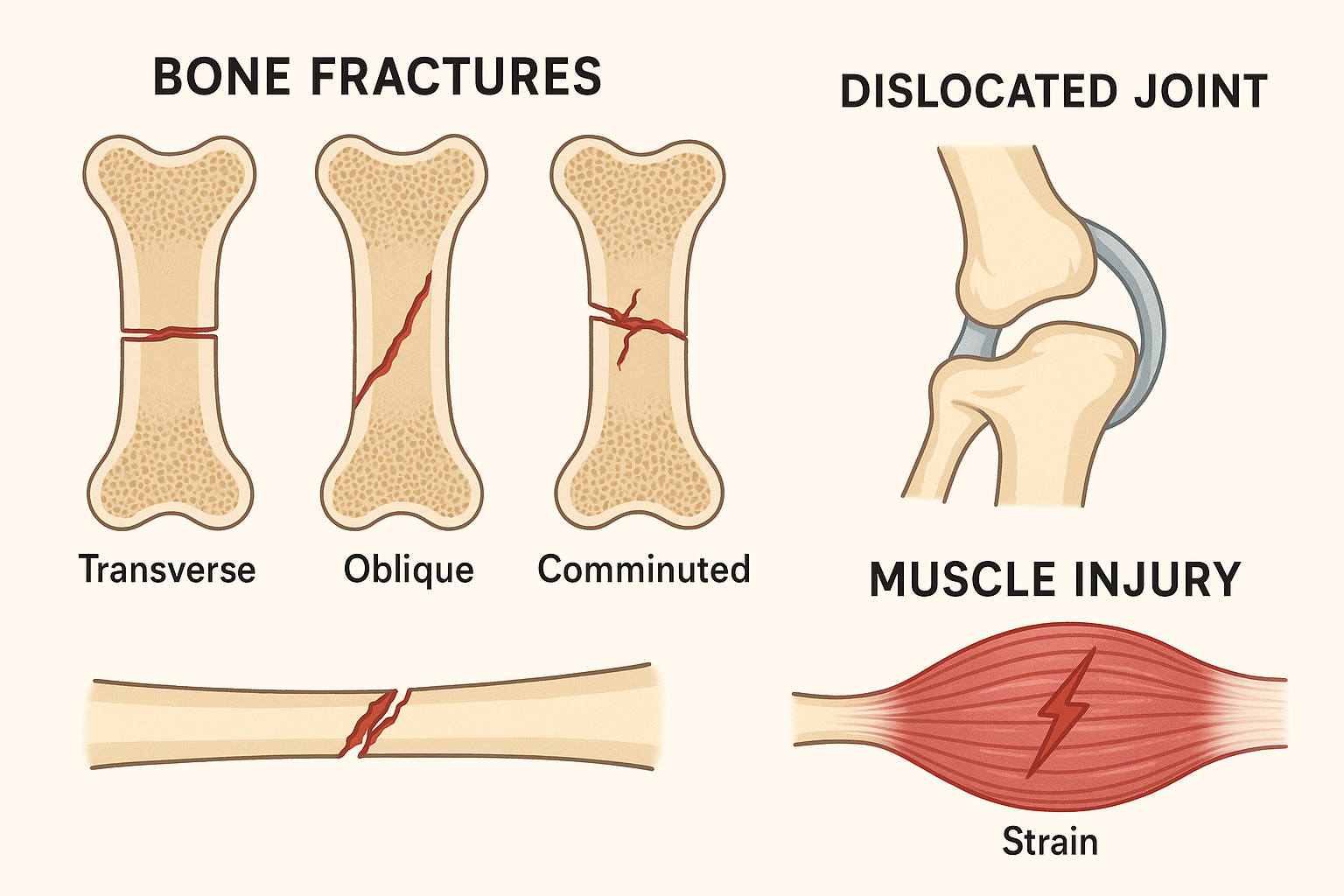
By Fracture Pattern
- Transverse: Horizontal break across the bone
- Oblique: Diagonal break across the bone
- Spiral: Twisting break around the bone shaft
- Comminuted: Bone shattered into multiple fragments
- Greenstick: Incomplete break (common in children)
- Compression: Bone crushed or collapsed
Critical Red Flags in Fractures
- Absent pulse distal to injury
- Severe pallor or cyanosis
- Complete loss of sensation
- Compartment syndrome signs
- Open fracture with contamination
- Neurovascular compromise
Common Fracture Sites and Special Considerations
| Fracture Site | Common Mechanism | Special Considerations |
|---|---|---|
| Femoral Neck | Fall on hip (elderly) | Risk of avascular necrosis, requires urgent surgery |
| Wrist (Colles’) | Fall on outstretched hand | Check for median nerve injury, “dinner fork” deformity |
| Ankle | Twisting injury | Assess stability, rule out syndesmosis injury |
| Ribs | Direct trauma | Watch for pneumothorax, pain management crucial |
3. Dislocations: Mechanisms and Types
A dislocation occurs when bones forming a joint are forced out of their normal anatomical position. This results in complete loss of joint function and often involves damage to surrounding ligaments, muscles, nerves, and blood vessels. Understanding the mechanism of injury helps predict associated complications and guide appropriate management.
Pathophysiology and Mechanisms
Dislocations typically result from high-energy trauma or forced movement beyond the joint’s normal range of motion. The injury disrupts the joint capsule and supporting structures, leading to immediate loss of function, severe pain, and potential neurovascular compromise. The position of the displaced bone often indicates the mechanism of injury and helps predict associated injuries.
Mnemonic: DISLOCATION Assessment – “Don’t Ignore Signs”
D – Deformity (obvious change in joint shape)
I – Immobility (inability to move joint)
S – Severe pain (often excruciating)
L – Loss of function
O – Obvious swelling
C – Circulation check (pulse, color, temperature)
A – Abnormal positioning
T – Tenderness on palpation
I – Instability of joint
O – Other associated injuries
N – Neurological assessment
Common Dislocations by Joint
Shoulder Dislocations (Most Common)
- Anterior (95%): Arm abducted and externally rotated, loss of rounded shoulder contour
- Posterior (4%): Often missed, arm held in internal rotation and adduction
- Inferior (1%): Rare, arm locked overhead
Key Complication: Axillary nerve injury (test deltoid function and sensation over lateral shoulder)
Finger/Thumb Dislocations
- PIP Joint: Most common, “swan neck” or “boutonnière” deformity possible
- MCP Joint: Thumb gamekeeper’s injury, UCL rupture
- DIP Joint: Usually simple, good prognosis
Key Consideration: Check for associated fractures, assess tendon function
Hip Dislocations
- Posterior (90%): Hip flexed, adducted, internally rotated
- Anterior (10%): Hip extended, abducted, externally rotated
Emergency: Requires reduction within 6 hours to prevent avascular necrosis of femoral head
Elbow Dislocations
- Posterior: Most common, often with coronoid or radial head fractures
- Anterior: Rare, high-energy trauma
Complications: Brachial artery injury, ulnar nerve palsy, compartment syndrome
Dislocation Emergencies – Immediate Action Required
- Hip dislocation: Reduce within 6 hours
- Knee dislocation: Check popliteal artery immediately
- Ankle dislocation: Urgent reduction to prevent skin necrosis
- Always check neurovascular status
- Document pre- and post-reduction exam
- Never attempt reduction without adequate analgesia
4. Muscle Injuries: Strains and Sprains
Muscle and soft tissue injuries encompass a wide range of conditions affecting muscles, tendons, and ligaments. Understanding the distinction between strains (muscle/tendon injuries) and sprains (ligament injuries) is crucial for appropriate assessment and management. These injuries range from minor overstretching to complete ruptures requiring surgical intervention.
Pathophysiology of Soft Tissue Injuries
Soft tissue injuries occur when forces exceed the tissue’s elastic limit, leading to fiber disruption and inflammatory response. The healing process involves three overlapping phases: inflammatory (0-72 hours), proliferative (3 days-6 weeks), and maturation/remodeling (6 weeks-6 months). Understanding these phases helps guide appropriate intervention timing and expectations for recovery.
Strain vs. Sprain Differentiation Flowchart
Force applied to musculoskeletal structure
Muscle or Tendon Injury
- • Pain with movement
- • Muscle weakness
- • Possible muscle spasm
Ligament Injury
- • Joint instability
- • Pain with weight bearing
- • Joint swelling
Classification by Severity
Grade I (Mild) Injuries
Strains:
- • Minimal fiber disruption (<5%)
- • Mild pain and tenderness
- • Full range of motion maintained
- • Normal strength
- • Return to activity: 2-10 days
Sprains:
- • Mild ligament stretching
- • Minimal swelling
- • Joint stability maintained
- • Weight bearing tolerated
- • Recovery: 1-3 weeks
Grade II (Moderate) Injuries
Strains:
- • Partial muscle fiber tears (5-50%)
- • Moderate pain and swelling
- • Decreased range of motion
- • Strength loss (25-50%)
- • Return to activity: 3-6 weeks
Sprains:
- • Partial ligament tear
- • Moderate swelling and bruising
- • Some joint instability
- • Painful weight bearing
- • Recovery: 3-8 weeks
Grade III (Severe) Injuries
Strains:
- • Complete muscle/tendon rupture
- • Severe pain followed by loss of pain
- • Complete loss of function
- • Palpable defect may be present
- • Often requires surgical repair
Sprains:
- • Complete ligament rupture
- • Significant swelling and bruising
- • Joint instability and abnormal motion
- • Unable to bear weight
- • May require surgical reconstruction
Mnemonic: MUSCLE Injury Assessment
M – Mechanism of injury
U – Unable to function normally
S – Swelling and deformity
C – Color changes (bruising)
L – Location of maximum tenderness
E – Examination of strength and range of motion
Common Muscle Injury Locations
| Location | Common Injury | Mechanism | Key Signs |
|---|---|---|---|
| Hamstring | Strain (Grade I-III) | Sudden acceleration, overstretching | Posterior thigh pain, weakness with knee flexion |
| Quadriceps | Contusion, strain | Direct blow, forceful contraction | Anterior thigh pain, difficulty with knee extension |
| Calf | Gastrocnemius strain | Sudden push-off movement | “Popping” sensation, unable to plantarflex |
| Ankle | Lateral ligament sprain | Inversion injury | Lateral ankle pain, swelling, instability |
| Shoulder | Rotator cuff strain | Overhead activities, repetitive motion | Shoulder pain, weakness with abduction |
5. Comprehensive Assessment Techniques
Systematic assessment of orthopedic injuries is crucial for identifying the extent of injury, associated complications, and determining appropriate interventions. A thorough assessment includes primary and secondary surveys, neurovascular evaluation, and ongoing monitoring. The assessment must be documented thoroughly and repeated regularly to identify changes in patient condition.
Assessment Principles
Always follow the primary survey (ABCDE) before focusing on specific injuries. Life-threatening conditions take precedence over limb-threatening conditions, which take precedence over simple fractures. Never assume a single injury – thoroughly assess for associated injuries.
Primary Survey: ABCDE Approach
A – Airway
- • Clear and patent
- • C-spine protection if trauma
- • Remove debris if present
B – Breathing
- • Rate and quality
- • Chest wall movement
- • Oxygen saturation
C – Circulation
- • Pulse rate and quality
- • Blood pressure
- • Signs of shock
D – Disability
- • Neurological status
- • Glasgow Coma Scale
- • Spinal assessment
E – Exposure
- • Full body examination
- • Log roll if needed
- • Prevent hypothermia
F – Full Set
- • Vital signs
- • Pain assessment
- • History taking
Secondary Survey: Focused Orthopedic Assessment
Systematic Orthopedic Examination Process
LOOK
- Deformity
- Swelling
- Bruising
- Open wounds
FEEL
- Tenderness
- Temperature
- Pulses
- Sensation
MOVE
- Active ROM
- Passive ROM
- Muscle strength
- Joint stability
SPECIAL
- X-rays
- Specific tests
- Measurements
- Documentation
Neurovascular Assessment: The “5 P’s”
Critical Mnemonic: The “5 P’s” of Neurovascular Assessment
PAIN
- Intensity (0-10)
- Quality
- Location
- Pain out of proportion
PALLOR
- Skin color
- Capillary refill
- Compare sides
- Temperature
PARESTHESIA
- Numbness
- Tingling
- Two-point discrimination
- Nerve distribution
PARALYSIS
- Motor function
- Muscle strength
- Active movement
- Reflexes
PULSELESSNESS
- Distal pulses
- Doppler if needed
- Compare sides
- Blood pressure
Critical Assessment Red Flags
Immediate Referral Required:
- Absent or diminished pulses
- Compartment syndrome signs
- Open fractures with contamination
- Complete neurological deficit
- Gross deformity with skin tenting
Close Monitoring Required:
- Progressive swelling
- Increasing pain despite treatment
- Change in neurological status
- Color changes in extremity
- Patient reporting unusual symptoms
Documentation Requirements
Initial Assessment Documentation:
- Time of injury and assessment
- Mechanism of injury
- Patient’s chief complaint
- Pain scale rating
- Neurovascular status (5 P’s)
- Deformity and visible injuries
- Range of motion assessment
Ongoing Assessment:
- Pain reassessment every 15-30 minutes
- Neurovascular checks every 15 minutes initially
- Response to interventions
- Changes in condition
- Patient education provided
- Family notification and involvement
- Discharge planning considerations
6. First Aid Management Protocols
Effective first aid management of orthopedic injuries focuses on immediate stabilization, pain control, prevention of further injury, and preparation for definitive treatment. The primary goals are to preserve life, prevent disability, and minimize complications. Understanding when to intervene and when to seek immediate medical attention is crucial for optimal outcomes.
Universal First Aid Mnemonic: “RICE PIES”
R – Rest (immobilize injured area)
I – Ice (apply cold therapy)
C – Compression (control swelling)
E – Elevation (reduce edema)
P – Pain management
I – Immobilization/stabilization
E – Evaluation (ongoing assessment)
S – Seek medical attention
Immediate First Aid Priorities
First Aid Decision Tree
Apply primary survey principles first
Hemorrhage, airway compromise, shock
- • Call 911 immediately
- • Control bleeding
- • Maintain airway
- • Treat for shock
- • Rapid transport
- • Assess neurovascular status
- • Immobilize injury
- • Apply ice and elevation
- • Provide pain relief
- • Arrange medical evaluation
Specific First Aid Protocols
Fracture Management Protocol
Immediate Actions:
- 1. Scene Safety: Ensure safe environment for you and patient
- 2. Primary Survey: ABCDE assessment, treat life threats first
- 3. Expose Injury: Remove clothing carefully, cut if necessary
- 4. Control Bleeding: Direct pressure if open fracture
- 5. Assess Circulation: Check pulse, color, temperature distal to injury
Stabilization Steps:
- 1. Immobilize: Splint above and below fracture site
- 2. Padding: Use soft materials to prevent pressure sores
- 3. Secure: Bandages snug but not tight enough to impair circulation
- 4. Recheck: Neurovascular status after immobilization
- 5. Document: Time, findings, interventions performed
- • Never attempt to reduce fractures in field setting
- • Immobilize in position found unless neurovascular compromise
- • Cover open wounds with sterile dressing before splinting
- • Monitor for signs of compartment syndrome
Dislocation Management Protocol
Assessment Priorities:
- Document neurovascular status immediately
- Photograph deformity if possible (with consent)
- Assess for associated fractures
- Note mechanism of injury
- Pain assessment (often severe initially)
Immediate Care:
- Apply ice wrapped in cloth (20 minutes on/off)
- Immobilize in position of comfort
- Administer pain medication per protocol
- Arrange immediate medical evaluation
- Monitor neurovascular status every 15 minutes
- • Suspected associated fracture
- • Neurovascular compromise
- • Multiple attempts by others
- • Inability to provide adequate analgesia
- • Inexperience with reduction technique
Muscle Injury Management Protocol
Grade I Injuries:
- • RICE protocol immediately
- • NSAIDs for pain/inflammation
- • Gentle range of motion
- • Return to activity as tolerated
- • Follow-up if no improvement
Grade II Injuries:
- • Strict RICE protocol
- • Immobilization 24-48 hours
- • Medical evaluation recommended
- • Physical therapy referral
- • Gradual return to activity
Grade III Injuries:
- • Immediate medical attention
- • Complete immobilization
- • Surgical evaluation needed
- • Pain management priority
- • Long-term rehab planning
Advanced First Aid Techniques
Splinting Principles
- Rule of Joints: Immobilize joint above and below fracture
- Rule of Bones: Immobilize bones above and below dislocated joint
- Padding: Use soft materials at bony prominences
- Positioning: Maintain anatomical alignment when possible
- Securing: Use triangular bandages, tape, or commercial splints
- Checking: Ensure splint doesn’t impair circulation
Cold Therapy Guidelines
- Application: 15-20 minutes every 1-2 hours
- Protection: Always use barrier (towel/cloth)
- Timing: Most effective within first 48 hours
- Benefits: Reduces swelling, pain, and muscle spasm
- Contraindications: Open wounds, impaired circulation
- Alternatives: Cold packs, frozen vegetables, ice water
First Aid Contraindications and Precautions
Never Attempt:
- Bone reduction without proper training
- Joint manipulation if fracture suspected
- Removal of impaled objects
- Moving patient with suspected spinal injury
- Giving oral medications if surgery possible
Use Caution With:
- Elderly patients (fragile skin, multiple comorbidities)
- Pediatric patients (growth plate considerations)
- Patients on anticoagulants (bleeding risk)
- Diabetic patients (healing impairment)
- Unconscious patients (inability to report symptoms)
7. Nursing Implementation and Care Plans
Nursing implementation for orthopedic injuries extends beyond immediate first aid to encompass comprehensive care planning, patient education, rehabilitation support, and prevention of complications. Nurses play a crucial role in coordinating care, advocating for patients, and ensuring continuity from emergency treatment through recovery and rehabilitation.
Nursing Process Applied to Orthopedic Injuries
Nursing Process Flowchart for Orthopedic Injuries
ASSESS
- Primary survey
- Focused assessment
- Neurovascular status
- Pain evaluation
- Psychosocial factors
DIAGNOSE
- Acute pain
- Impaired mobility
- Risk for infection
- Anxiety/fear
- Self-care deficit
PLAN
- Set goals
- Prioritize interventions
- Coordinate care
- Patient education
- Discharge planning
IMPLEMENT
- Pain management
- Immobilization
- Wound care
- Mobility assistance
- Teaching
EVALUATE
- Goal achievement
- Pain relief
- Complication prevention
- Patient satisfaction
- Plan revision
Priority Nursing Diagnoses
High Priority: Acute Pain Related to Tissue Injury
Goals:
- • Patient reports pain level ≤ 4/10 within 30 minutes of intervention
- • Patient demonstrates use of non-pharmacological pain management
- • Patient experiences minimal pain during necessary movement
Interventions:
- • Assess pain using standardized scale every 15-30 minutes
- • Administer analgesics per physician orders
- • Apply ice therapy as appropriate
- • Position for comfort and support injured area
- • Teach relaxation and distraction techniques
High Priority: Impaired Physical Mobility Related to Injury
Goals:
- • Patient maintains current range of motion in unaffected joints
- • Patient demonstrates safe use of assistive devices
- • Patient participates in prescribed activity level
Interventions:
- • Assess current mobility level and limitations
- • Maintain proper body alignment during immobilization
- • Encourage movement of unaffected extremities
- • Provide assistive devices and teach proper use
- • Collaborate with physical therapy for mobility plan
Medium Priority: Risk for Infection Related to Open Wounds
Goals:
- • Patient remains free from signs/symptoms of infection
- • Wound healing progresses without complications
- • Patient verbalizes understanding of infection prevention
Interventions:
- • Maintain sterile technique during wound care
- • Monitor for signs of infection (redness, warmth, drainage)
- • Administer antibiotics as prescribed
- • Teach patient wound care and hygiene measures
- • Document wound characteristics and healing progress
Specific Nursing Interventions
Pain Management Strategies
- Pharmacological:
- • Opioids for severe acute pain
- • NSAIDs for inflammation and moderate pain
- • Acetaminophen for mild to moderate pain
- • Topical analgesics for localized pain
- Non-pharmacological:
- • Cold therapy (first 48 hours)
- • Heat therapy (after acute phase)
- • TENS unit application
- • Massage therapy
- • Relaxation techniques
- • Distraction activities
Monitoring and Assessment
- Neurovascular Checks:
- • Every 15 minutes for first hour
- • Every 30 minutes for next 2 hours
- • Every hour thereafter
- • Document using standardized forms
- Complication Surveillance:
- • Compartment syndrome signs
- • Fat embolism symptoms
- • Deep vein thrombosis indicators
- • Infection development
- • Pressure ulcer formation
Patient Education Priorities
Immediate Care:
- • Signs of complications to report
- • Proper use of assistive devices
- • Medication administration and side effects
- • Activity restrictions and modifications
Recovery Phase:
- • Rehabilitation exercise programs
- • Gradual return to activities
- • Nutrition for healing
- • Follow-up appointment schedule
Prevention:
- • Home safety modifications
- • Fall prevention strategies
- • Bone health maintenance
- • Activity safety guidelines
Interdisciplinary Collaboration
Healthcare Team Members:
- Orthopedic Surgeon: Surgical decisions, treatment planning
- Physical Therapist: Mobility restoration, strength training
- Occupational Therapist: ADL adaptation, assistive devices
- Pharmacist: Medication management, drug interactions
- Dietitian: Nutritional support for healing
- Case Manager: Discharge planning, resource coordination
Nurse’s Coordination Role:
- • Communicate patient status to team members
- • Coordinate care schedules and interventions
- • Advocate for patient needs and preferences
- • Facilitate family meetings and discussions
- • Monitor progress toward team-established goals
- • Document interdisciplinary communications
- • Ensure continuity of care across settings
8. Complications and Red Flags
Recognition and early intervention for complications in orthopedic injuries can mean the difference between full recovery and permanent disability. Nurses must maintain high vigilance for both immediate and delayed complications, understanding their pathophysiology, risk factors, and appropriate interventions. Some complications require emergency intervention, while others require prompt medical evaluation and adjustment of the treatment plan.
Classification of Complications
Immediate Complications (0-24 hours)
- Hemorrhage: External bleeding or internal hematoma formation
- Compartment Syndrome: Increased pressure within fascial compartments
- Shock: Hypovolemic from blood loss or neurogenic
- Neurovascular Injury: Nerve damage or vascular compromise
- Fat Embolism: Release of fat globules into circulation
Delayed Complications (Days to Weeks)
- Infection: Superficial, deep, or osteomyelitis
- Malunion: Healing in incorrect position
- Non-union: Failure of bone healing
- Joint Stiffness: Loss of range of motion
- Thromboembolism: DVT or pulmonary embolism
Critical Complications Requiring Immediate Action
Compartment Syndrome – EMERGENCY
Pathophysiology:
Increased pressure within a closed fascial space compromises circulation, leading to tissue ischemia and potential necrosis. Most commonly affects forearm and lower leg compartments.
Risk Factors:
- • Fractures (especially tibia, forearm)
- • Crushing injuries
- • Prolonged compression
- • Reperfusion after ischemia
- • Tight casts or dressings
“5 P’s” Late Signs (Irreversible)
- Pain (severe, out of proportion)
- Pallor (pale, cool skin)
- Paresthesias (numbness, tingling)
- Paralysis (inability to move)
- Pulselessness (absent distal pulses)
Early Warning Signs:
- • Pain with passive muscle stretching
- • Tense, swollen compartment
- • Pain out of proportion to injury
- • Decreased sensation
IMMEDIATE SURGICAL DECOMPRESSION REQUIRED
Fat Embolism Syndrome
Clinical Presentation:
Classic Triad:
- • Respiratory: Dyspnea, tachypnea, hypoxemia
- • Neurological: Confusion, agitation, coma
- • Dermatological: Petechial rash (chest, axilla, neck)
Risk Factors:
- • Long bone fractures (especially femur)
- • Multiple fractures
- • Orthopedic surgery with reaming
- • Young age (15-30 years)
Nursing Assessment:
- Respiratory: Monitor oxygen saturation, respiratory rate, breath sounds
- Neurological: Level of consciousness, confusion, restlessness
- Vital Signs: Fever, tachycardia, hypotension
- Skin: Petechial rash examination
- Laboratory: ABGs, platelet count, hemoglobin
Early mobilization and proper fracture stabilization can prevent fat embolism syndrome.
Orthopedic Infections
Superficial Infection:
- • Redness around wound
- • Increased warmth
- • Purulent drainage
- • Local tenderness
- • Fever may be absent
Deep Infection:
- • Persistent deep pain
- • Systemic symptoms
- • Elevated WBC, ESR, CRP
- • Possible abscess formation
- • Delayed healing
Osteomyelitis:
- • Bone pain and tenderness
- • High fever, chills
- • Possible sinus tract
- • Bone destruction on X-ray
- • Chronic, recurrent course
Monitoring and Prevention Strategies
Prevention Strategies
- Compartment Syndrome:
- • Frequent neurovascular assessments
- • Proper splint/cast application
- • Elevation of injured extremity
- • Prompt treatment of swelling
- Infection:
- • Sterile technique for wound care
- • Appropriate antibiotic prophylaxis
- • Early mobilization when appropriate
- • Nutritional support for healing
- Thromboembolism:
- • Early mobilization
- • Sequential compression devices
- • Anticoagulation per protocol
- • Adequate hydration
Monitoring Protocols
- Frequency of Assessment:
- • High-risk patients: every 15 minutes initially
- • Stable patients: every 30-60 minutes
- • Post-operative: per protocol
- • Document all findings
- Key Parameters:
- • Pain level and characteristics
- • Neurovascular status
- • Wound appearance and drainage
- • Temperature and vital signs
- Documentation Requirements:
- • Time-stamped assessments
- • Objective measurements
- • Patient-reported symptoms
- • Interventions and responses
9. Documentation and Legal Considerations
Comprehensive documentation in orthopedic injury care serves multiple critical purposes: ensuring continuity of care, providing legal protection, facilitating quality improvement, and supporting billing and reimbursement. Nurses must understand both the clinical and legal implications of their documentation, maintaining accuracy, completeness, and timeliness in all records.
Essential Documentation Elements
Initial Assessment Documentation
- Patient Identification: Name, DOB, medical record number, time/date
- Mechanism of Injury: Detailed description of how injury occurred
- Chief Complaint: Patient’s description in their own words
- Pain Assessment: Location, quality, intensity (0-10 scale), aggravating/relieving factors
- Physical Examination: Inspection, palpation, range of motion, deformity
- Neurovascular Status: Complete 5 P’s assessment with specific findings
- Associated Injuries: Other trauma or medical conditions present
- Medications: Current medications, allergies, last tetanus shot
Ongoing Care Documentation
- Vital Signs: Complete set with trends and abnormalities noted
- Pain Reassessment: Response to interventions, new pain complaints
- Neurovascular Checks: Time-stamped assessments with comparison to baseline
- Interventions Performed: Medications given, treatments applied, patient responses
- Patient Education: Information provided, patient understanding demonstrated
- Communication: Physician notifications, family contacts, consultations
- Discharge Planning: Home care needs, follow-up appointments, resources
Documentation Mnemonic: “FACT”
F – Factual (objective, observable data)
A – Accurate (correct spelling, proper terminology)
C – Complete (all relevant information included)
T – Timely (documented promptly after occurrence)
Legal Considerations and Risk Management
High-Risk Documentation Areas
Common Liability Issues:
- • Failure to recognize compartment syndrome
- • Delayed identification of neurovascular compromise
- • Inadequate pain management documentation
- • Missing or incomplete neurovascular assessments
- • Failure to follow up on abnormal findings
- • Inadequate patient education documentation
Protective Documentation Practices:
- • Document exact time of assessments
- • Use specific, measurable terms
- • Record patient’s exact words for complaints
- • Document all attempts to contact physicians
- • Note patient compliance and non-compliance
- • Keep contemporaneous records
Documentation Errors to Avoid
Never Do:
- Use correction fluid or erasers
- Leave blank spaces in documentation
- Use vague terms like “normal” or “fine”
- Document care before providing it
- Use unapproved abbreviations
- Chart for others or allow others to chart for you
Always Do:
- Draw single line through errors, initial, and date
- Use complete sentences with proper grammar
- Be specific with measurements and descriptions
- Document contemporaneously when possible
- Use approved medical terminology
- Sign and date all entries
Quality Improvement Through Documentation
Using Documentation for Quality Metrics
Patient Safety Indicators:
- • Time to pain assessment
- • Frequency of neurovascular checks
- • Complication recognition time
- • Fall prevention measures
- • Infection control practices
Clinical Outcomes:
- • Length of stay
- • Readmission rates
- • Patient satisfaction scores
- • Functional outcomes
- • Complication rates
Process Measures:
- • Time to first assessment
- • Education completion rates
- • Discharge planning timeliness
- • Medication administration accuracy
- • Care plan adherence
Best Practices for Electronic Documentation
System Security:
- • Never share passwords or login credentials
- • Log out when leaving computer unattended
- • Use secure networks for remote access
- • Report system malfunctions immediately
- • Maintain confidentiality at all times
Efficiency Tips:
- • Use templates and flowsheets appropriately
- • Customize documentation to patient needs
- • Document in real-time when possible
- • Review entries for accuracy before finalizing
- • Stay current with system updates and training
10. Summary and Key Takeaways
The management of fractures, dislocations, and muscle injuries requires a systematic approach combining immediate first aid interventions, comprehensive nursing assessment, and ongoing monitoring for complications. Success in orthopedic injury care depends on early recognition, appropriate interventions, interdisciplinary collaboration, and thorough documentation. This knowledge forms the foundation for safe, effective nursing practice in emergency and orthopedic settings.
Essential Clinical Principles
Assessment Priorities:
- Always perform primary survey (ABCDE) first
