First Aid Management of Poisoning
Comprehensive Nursing Study Notes
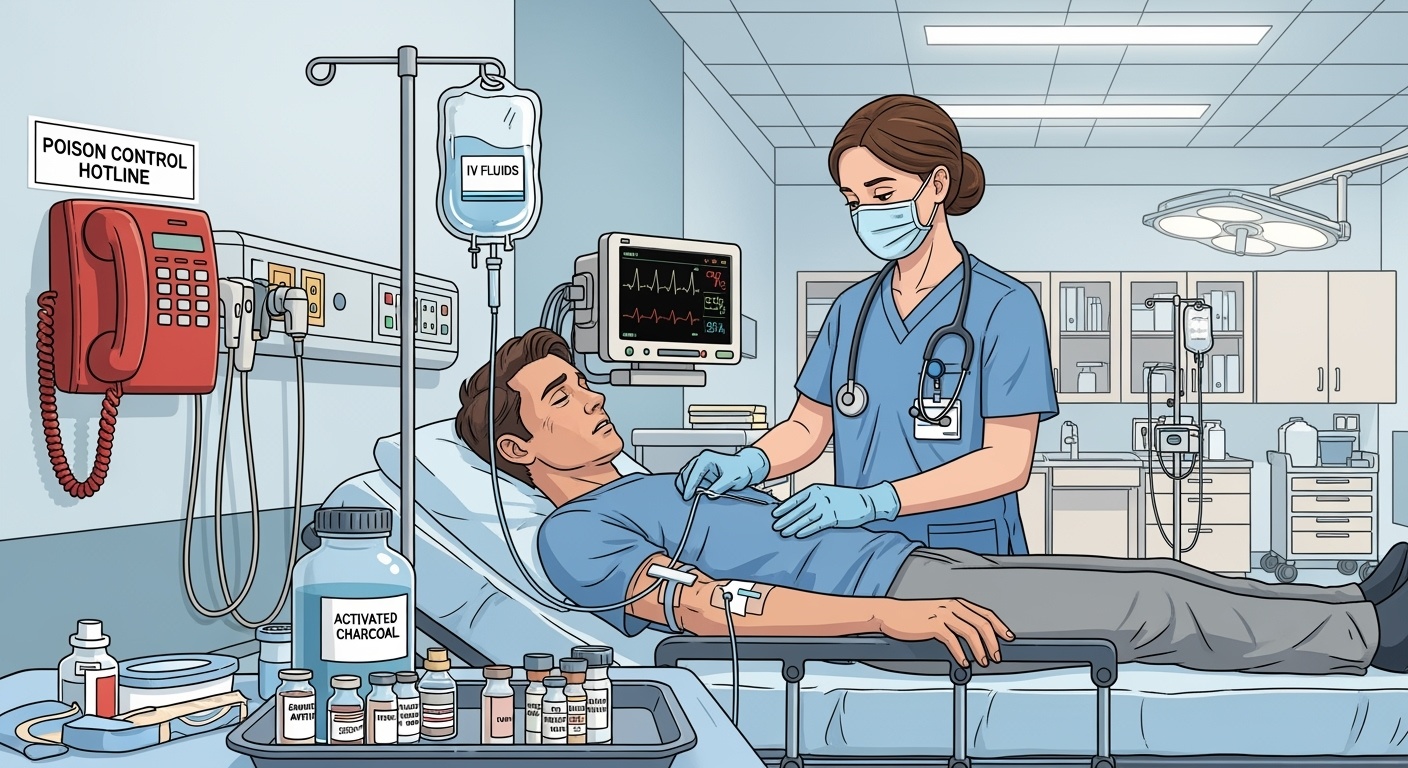
Table of Contents
1. Introduction to Poisoning
Definition and Scope
Poisoning refers to the harmful effects that result from exposure to toxic substances in quantities sufficient to cause cellular injury, organ dysfunction, or death. It represents a significant public health concern affecting millions worldwide annually, with particular vulnerability among children, elderly populations, and individuals with mental health conditions.
The World Health Organization estimates that approximately 193,000 people die annually from unintentional poisoning globally. In healthcare settings, nurses serve as frontline responders, making their knowledge of first aid management critical for optimal patient outcomes.
Memory Aid: POISONING
P – Protect yourself and others
O – Obtain history and vital signs
I – Identify the poison
S – Support airway, breathing, circulation
O – Order appropriate tests
N – Notify poison control center
I – Initiate decontamination if appropriate
N – Navigate antidote administration
G – Give supportive care and monitor
2. Classification of Poisons
By Route of Exposure
- Ingestion: Most common route (80-85% of cases)
- Inhalation: Gases, vapors, aerosols
- Dermal: Skin absorption
- Injection: Parenteral, bites, stings
- Ocular: Eye exposure
By Origin
- Pharmaceutical: Medications, overdoses
- Household: Cleaning products, cosmetics
- Industrial: Chemicals, solvents
- Agricultural: Pesticides, herbicides
- Biological: Plant, animal toxins
- Environmental: Heavy metals, pollutants
Clinical Pearl
The “Rule of 5s” for pediatric poisoning: Most pediatric ingestions involve substances found within 5 feet of the ground, occur within 5 minutes of inadequate supervision, and involve less than 5 mL or 5 grams of substance.
3. Pathophysiology of Poisoning
Toxicokinetics: The ADME Process
Absorption
Entry into systemic circulation
Distribution
Transport to target organs
Metabolism
Biotransformation processes
Elimination
Removal from the body
Understanding toxicokinetics helps nurses anticipate the timeline of toxic effects and guide appropriate interventions. Factors affecting these processes include age, organ function, genetic variations, and co-ingested substances.
Mechanisms of Toxicity
- Cellular Disruption: Direct membrane damage
- Enzyme Inhibition: Metabolic pathway interference
- Receptor Antagonism: Blocking normal signaling
- Oxidative Stress: Free radical damage
- Protein Denaturation: Structural alterations
Dose-Response Relationship
Paracelsus’s principle: “The dose makes the poison”
- Threshold Effect: Minimum dose for toxicity
- Linear Response: Proportional increase
- Saturation Kinetics: Maximum effect reached
- Individual Variation: Genetic and physiologic factors
4. Initial Assessment & Triage
Assessment Flowchart
Scene Safety
Protect self & others
Primary Survey
ABCDE assessment
History Taking
SAMPLE method
Physical Exam
Systematic approach
Poison Control
Expert consultation
History Taking: SAMPLE Method
S – Signs and Symptoms
A – Allergies and Antidotes used
M – Medications and Medical history
P – Past medical history, Pregnancy
L – Last meal, Last menstrual period
E – Events leading to exposure
Triage Categories
- Priority 1: Life-threatening presentations
- Priority 2: Potentially serious exposures
- Priority 3: Non-urgent exposures
- Information: Counseling and reassurance
Assessment Priorities
- 1. Ensure scene safety and personal protection
- 2. Stabilize airway, breathing, and circulation
- 3. Obtain accurate exposure history
- 4. Identify the poison and quantity if possible
- 5. Contact poison control center immediately
5. General Management Principles
The Four Pillars of Poison Management
Supportive Care
Maintain vital functions
Decontamination
Remove or neutralize poison
Antidote Therapy
Specific counteragents
Enhanced Elimination
Accelerate toxin removal
Critical Safety Warnings
- Never induce vomiting unless specifically directed by poison control
- Avoid neutralizing agents (milk, acids, bases) – they can cause thermal injury
- Do not give activated charcoal for corrosives, hydrocarbons, or alcohols
- Maintain universal precautions – some toxins are transmissible
- Consider co-ingestions – multiple substances may be involved
Nursing Priority Actions
Immediate Actions (0-5 minutes)
- • Ensure personal safety and PPE
- • Assess and support ABC
- • Obtain brief exposure history
- • Call Poison Control: 1-800-222-1222
- • Initiate cardiac monitoring
Secondary Actions (5-15 minutes)
- • Complete physical assessment
- • Obtain IV access
- • Collect specimens as indicated
- • Document thoroughly
- • Prepare for decontamination
6. Decontamination Methods
Ocular
Irrigation with normal saline
Dermal
Remove clothing, wash skin
Inhalation
Remove from source, oxygen
Ingestion
Activated charcoal if appropriate
Activated Charcoal Administration
Indications
- • Most organic compounds
- • Within 1-2 hours of ingestion
- • Conscious patient with intact gag reflex
- • Significant ingestion quantity
- • No contraindications present
Contraindications
- • Altered mental status
- • Corrosive ingestions
- • Hydrocarbon ingestions
- • Alcohols, metals, electrolytes
- • GI obstruction or perforation
Dosing Guidelines
Adults: 25-50 grams in 100-200 mL water
Children: 1-2 grams/kg (maximum 25 grams)
Administration: Mix to slurry consistency, administer via large-bore NG tube if necessary
Decontamination Decision: CHARCOAL
C – Conscious and cooperative patient
H – Hours since ingestion (<2 hours optimal)
A – Adsorbable substance (organic compounds)
R – Reasonable amount ingested
C – Contraindications absent
O – Oral route safe and accessible
A – Anticipated benefit outweighs risks
L – Life-threatening exposure potential
7. Specific Antidotes and Treatments
Common Antidote Pairs
Antidote Administration Principles
- Time-sensitive: Earlier administration generally more effective
- Risk-benefit analysis: Some antidotes have significant side effects
- Dose calculations: Most are weight-based, verify calculations
- Monitoring requirements: Continuous assessment during and after administration
- Repeat dosing: Many require multiple doses or continuous infusion
High-Alert Antidotes
- Flumazenil: Risk of seizures in chronic benzos users
- Naloxone: May precipitate withdrawal, short half-life
- Physostigmine: Contraindicated in tricyclic overdose
- Calcium: Tissue necrosis if extravasated
Nursing Considerations
- Verify antidote appropriateness with poison control
- Check expiration dates and proper storage
- Monitor for allergic reactions during administration
- Document response and any adverse effects
- Prepare for potential repeat doses
8. Supportive Care Management
ABCDE Approach to Supportive Care
Airway
Position, suction, intubation if needed
Breathing
Oxygen, ventilation support
Circulation
IV access, fluid resuscitation
Disability
Neurologic assessment, glucose
Exposure
Temperature control, full exam
Cardiovascular Support
- Hypotension: IV fluids, vasopressors if needed
- Arrhythmias: Antiarrhythmic agents, electrical therapy
- Monitoring: Continuous ECG, frequent vital signs
- Access: Large-bore IV, central line if indicated
Sodium bicarbonate for tricyclic antidepressant overdose with wide QRS (>100ms)
Neurological Support
- Altered mental status: Glucose, thiamine, naloxone
- Seizures: Benzodiazepines first-line
- Agitation: Environmental controls, chemical restraints
- Monitoring: Glasgow Coma Scale, pupil response
Coma cocktail: Glucose, thiamine, naloxone (consider flumazenil with caution)
Supportive Care Mnemonic: SUPPORT
S – Stabilize vital signs
U – Urine output monitoring
P – Prevent complications
P – Pain management
O – Oxygen and ventilation
R – Renal function protection
T – Temperature regulation
9. Nursing Interventions and Care Plans
Priority Nursing Diagnoses
Immediate Priority
- • Ineffective airway clearance
- • Impaired gas exchange
- • Decreased cardiac output
- • Risk for injury
- • Altered mental status
Secondary Priority
- • Anxiety related to emergency
- • Knowledge deficit
- • Risk for aspiration
- • Fluid volume imbalance
- • Family coping issues
Comprehensive Nursing Assessment
Respiratory
- • Respiratory rate and pattern
- • Oxygen saturation
- • Breath sounds
- • Use of accessory muscles
- • Cyanosis or color changes
Cardiovascular
- • Heart rate and rhythm
- • Blood pressure
- • Capillary refill
- • Peripheral pulses
- • Skin temperature
Neurological
- • Level of consciousness
- • Pupil size and reaction
- • Motor responses
- • Speech patterns
- • Seizure activity
Documentation Essentials
- Time and circumstances of exposure
- Substance involved (bring container if available)
- Estimated quantity and route
- Time of symptom onset
- Pre-hospital interventions
- Serial vital signs and assessments
- Interventions and patient responses
- Poison control consultations
Red Flag Symptoms
- Altered mental status or unconsciousness
- Respiratory distress or apnea
- Cardiac arrhythmias or instability
- Seizure activity
- Severe hyperthermia or hypothermia
- Signs of shock or circulatory compromise
- Corrosive injuries to mucous membranes
Patient and Family Education
Prevention Strategies
- • Proper medication storage and labeling
- • Childproofing homes and securing toxins
- • Reading labels and following directions
- • Avoiding mixing household chemicals
- • Installing carbon monoxide detectors
- • Safe disposal of medications
Emergency Response
- • Poison Control Center: 1-800-222-1222
- • When to call 911 vs. poison control
- • What information to have ready
- • First aid measures to take/avoid
- • Follow-up care instructions
- • Warning signs requiring immediate return
10. Legal and Ethical Considerations
Legal Framework for Poisoning Cases
Mandatory Reporting
- Child abuse/neglect: Suspicious circumstances in pediatric cases
- Elder abuse: Potential neglect or intentional harm
- Workplace exposures: OSHA requirements
- Public health threats: Contamination or epidemic potential
- Criminal activity: Suspected intentional poisoning
Documentation Requirements
- Chain of custody: For potential legal specimens
- Witness statements: Accurate recording of events
- Photographic evidence: Injuries or scene documentation
- Consent processes: Treatment authorization
- Discharge planning: Safety assessments
Ethical Dilemmas in Poisoning Cases
Intentional Self-Harm
Balance patient autonomy with duty to preserve life. Psychiatric evaluation often required before discharge.
Pediatric Cases
Child’s best interest vs. parental rights. Consider child protective services involvement when appropriate.
Confidentiality vs. Safety
When to break confidentiality to protect patient or others from ongoing harm.
Consent Considerations
- Altered mental status: May require emergency treatment without consent
- Minor patients: Parental consent required except in emergencies
- Psychiatric holds: Understanding involuntary commitment procedures
- Refusal of treatment: Capacity assessment and documentation
- Surrogate decision-makers: Identifying appropriate representatives
11. Prevention Strategies and Public Health
Home Safety Assessment
Kitchen Safety
- • Lock cabinets with cleaning supplies
- • Use original containers only
- • Install cabinet latches
- • Keep appliances unplugged
Bathroom Safety
- • Medicine cabinet locks
- • Proper medication disposal
- • Cosmetic and toiletry storage
- • Ventilation for cleaning products
General Home
- • Carbon monoxide detectors
- • Proper storage of automotive products
- • Paint and solvent safety
- • Garden chemical security
Community Education Programs
- School presentations: Age-appropriate poison prevention
- Parent education: Childproofing and emergency response
- Senior programs: Medication safety and management
- Workplace training: Chemical safety and emergency procedures
- Healthcare provider education: Recognition and management updates
High-Risk Populations
- Children <6 years: Exploratory behavior, accessibility issues
- Elderly patients: Polypharmacy, cognitive changes
- Mental health patients: Intentional overdose risk
- Substance users: Adulterants and unknown compositions
- Occupational workers: Chemical and industrial exposures
Prevention Mnemonic: SAFE HOME
S – Secure all medications and chemicals
A – Always use original containers
F – Follow label directions exactly
E – Educate all household members
H – Have poison control number accessible
O – Out of reach and sight storage
M – Monitor expiration dates
E – Emergency plan established
12. Case Studies and Clinical Scenarios
Case Study 1: Pediatric Acetaminophen Overdose
Scenario
3-year-old male presents 2 hours after ingesting approximately 15 children’s acetaminophen tablets (80mg each). Child found with empty bottle, is awake and alert, no symptoms currently.
Immediate Nursing Actions
- • Assess airway, breathing, circulation
- • Calculate ingested dose: 15 × 80mg = 1200mg
- • Weight-based toxicity: 1200mg ÷ 15kg = 80mg/kg
- • Contact poison control immediately
- • Prepare for activated charcoal if indicated
Treatment Plan
- • Activated charcoal within 2 hours if >150mg/kg
- • 4-hour acetaminophen level
- • Plot on Rumack-Matthew nomogram
- • NAC therapy if indicated
- • Monitor liver function tests
- • Consider child protective services
Learning Point: Toxic dose >150mg/kg in children, >7.5g in adults. Early intervention crucial for hepatotoxicity prevention.
Case Study 2: Adult Tricyclic Antidepressant Overdose
Scenario
45-year-old female with depression, found unconscious 1 hour after taking “a handful” of amitriptyline tablets. Initial vitals: BP 80/40, HR 120, wide-complex tachycardia on ECG.
Critical Presentations
- • Altered mental status
- • Cardiovascular toxicity (wide QRS)
- • Anticholinergic effects
- • Potential for rapid deterioration
Management Priorities
- • Airway protection (intubation likely)
- • Sodium bicarbonate for QRS >100ms
- • Activated charcoal if airway protected
- • Avoid physostigmine (contraindicated)
- • Continuous cardiac monitoring
- • Psychiatric consultation for disposition
Critical Point: Sodium bicarbonate is first-line therapy for TCA-induced wide QRS complexes. Target serum pH 7.45-7.55.
Case Study 3: Carbon Monoxide Poisoning
Scenario
Family of 4 presents with headaches, nausea, and confusion after generator use during power outage. CO level 25% on arterial blood gas. Youngest child (age 2) most symptomatic.
Clinical Presentation
- • “Flu-like” symptoms initially
- • Headache, dizziness, nausea
- • Confusion, altered mental status
- • Cherry-red skin (late finding)
Treatment Protocol
- • 100% oxygen via non-rebreather mask
- • Consider hyperbaric oxygen therapy
- • Neurological assessments
- • Treat all family members
- • Home safety evaluation
- • Follow-up for delayed neurological effects
Prevention Focus: Education about CO detector installation, proper ventilation, and generator safety crucial for preventing future exposures.
Key Takeaways for Nursing Practice
Clinical Excellence
- • Systematic assessment using ABCDE approach
- • Early poison control center consultation
- • Evidence-based decontamination decisions
- • Appropriate antidote administration
- • Comprehensive supportive care
Professional Responsibilities
- • Accurate documentation and reporting
- • Patient and family education
- • Legal and ethical considerations
- • Prevention advocacy
- • Continuing education and competency
Essential Resources
Emergency Contacts
- Poison Control Center: 1-800-222-1222
- Emergency Services: 911
- AAPCC Online: www.aapcc.org
- CDC Poisoning Prevention: www.cdc.gov/poisoning
Professional References
- Goldfrank’s Toxicologic Emergencies
- Poisindex System (Micromedex)
- AACT Position Statements
- Emergency Nursing Core Curriculum

