First Aid Management of Bites
Comprehensive Nursing Study Notes
Osmosis-Style Medical Education • Evidence-Based Practice
Comprehensive first aid management approaches for various types of bites
Table of Contents
Introduction to Bite Management
Bite injuries represent a significant portion of emergency presentations, requiring immediate and appropriate first aid management. As nursing professionals, understanding the pathophysiology, clinical presentation, and evidence-based interventions for various bite types is crucial for optimal patient outcomes.
Epidemiology
- Annual incidence: 4.5 million dog bites in the US
- Snake bites: 7,000-8,000 venomous bites annually
- Human bites: 250,000 cases requiring medical attention
- Infection rates: 3-18% depending on bite type
Critical Considerations
- Time-sensitive interventions save lives
- Infection prevention is paramount
- Documentation affects legal outcomes
- Patient education prevents recurrence
Classification of Bite Injuries
| Bite Type | Primary Concerns | Infection Risk | Mortality Risk |
|---|---|---|---|
| Venomous Snake | Systemic envenomation, coagulopathy | Moderate (5-10%) | High (0.06%) |
| Dog/Cat | Deep puncture wounds, crush injury | Moderate (5-25%) | Low (<0.01%) |
| Human | Polymicrobial infection, viral transmission | High (10-50%) | Low |
| Insect/Spider | Allergic reactions, local necrosis | Low (1-5%) | Variable |
General First Aid Principles
SAFE-BITE Mnemonic
S – Scene safety and self-protection
A – Assess airway, breathing, circulation
F – First aid measures (pressure, elevation)
E – Emergency services activation
B – Bite identification and documentation
I – Immobilization of affected area
T – Tetanus prophylaxis consideration
E – Emergency department transport
Universal First Aid Steps
Ensure personal protection
ABCs (Airway, Breathing, Circulation)
Control bleeding, cleanse if appropriate
Prevent movement, reduce spread
Emergency services or hospital
DO’s
- ✓ Maintain calm, reassuring demeanor
- ✓ Use universal precautions (gloves, barriers)
- ✓ Document time, circumstances, and interventions
- ✓ Monitor vital signs and consciousness level
- ✓ Apply direct pressure for bleeding control
- ✓ Elevate extremity above heart level if possible
- ✓ Immobilize affected limb with splinting
- ✓ Remove jewelry before swelling occurs
DON’Ts
- ✗ Never apply tourniquets unless life-threatening hemorrhage
- ✗ Avoid ice application directly to bite wounds
- ✗ Don’t use suction devices or cut-and-suck methods
- ✗ Never give alcohol or stimulants to the patient
- ✗ Avoid excessive movement of bitten extremity
- ✗ Don’t attempt to capture or kill the animal
- ✗ Never leave patient unattended if systemic symptoms
- ✗ Avoid delaying professional medical care
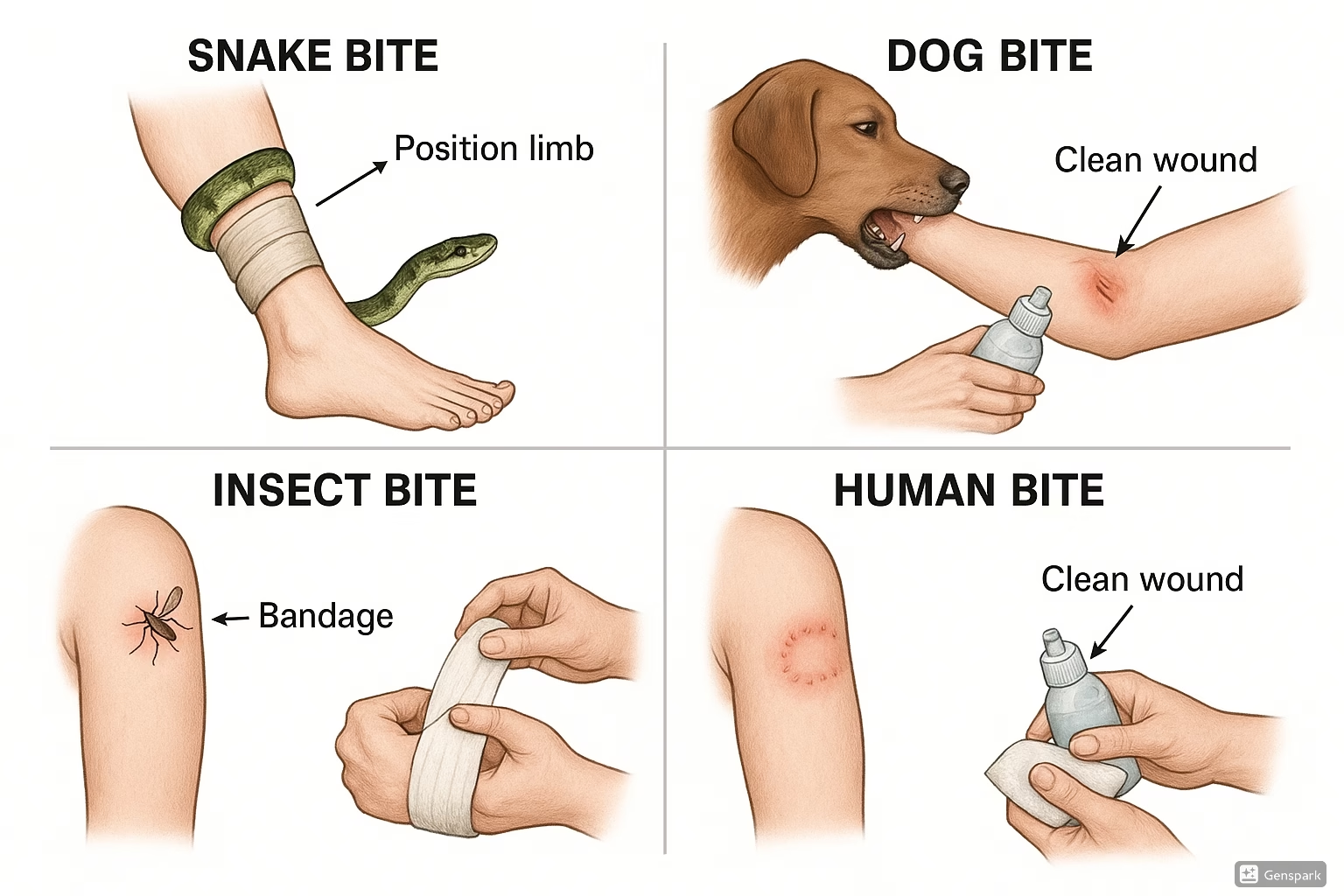
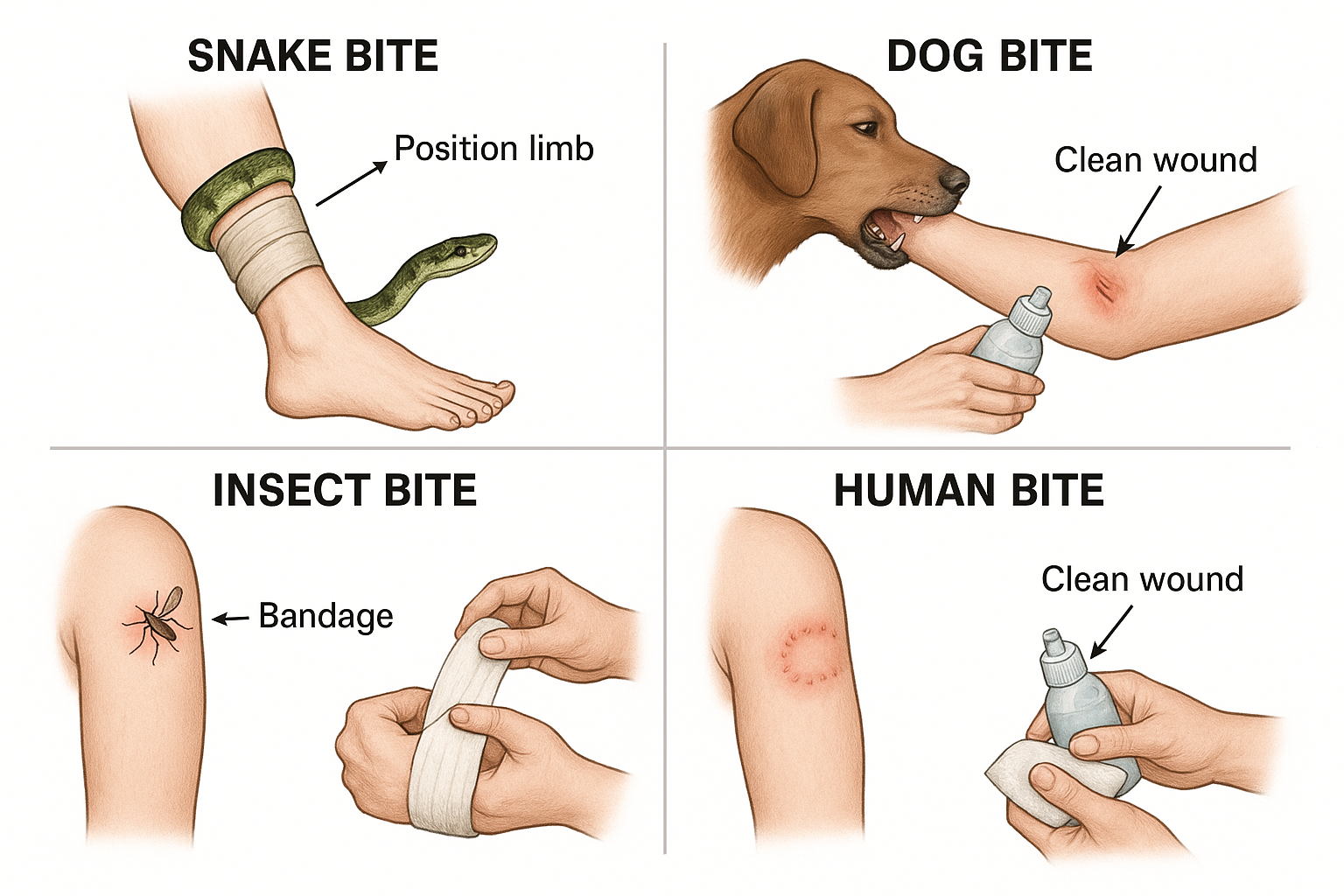
Snake Bite Management
Snake bite envenomation represents a true medical emergency requiring immediate, systematic intervention. The severity of envenomation varies significantly based on species, venom load, patient factors, and time to treatment.
SNAKE-BITE Assessment Mnemonic
S – Species identification (if possible)
N – Neurological symptoms assessment
A – Area of bite location and fang marks
K – Keep patient calm and still
E – Evaluate systemic symptoms
B – Blood coagulation monitoring
I – Immobilize affected extremity
T – Time documentation crucial
E – Emergency transport immediately
Venomous vs. Non-Venomous Recognition
| Characteristic | Venomous Species | Non-Venomous Species |
|---|---|---|
| Bite Pattern | Two distinct puncture wounds (fangs) | Multiple small puncture marks |
| Local Symptoms | Immediate severe pain, swelling, discoloration | Minimal pain, limited swelling |
| Systemic Signs | Nausea, weakness, altered consciousness | Usually absent |
| Progression | Rapid worsening within 30-60 minutes | Stable or improving |
Immediate First Aid Protocol
Time-Critical Steps (First 15 Minutes)
Minutes 0-5:
- • Move patient away from snake
- • Keep patient calm and lying down
- • Remove constricting items immediately
- • Mark swelling progression with pen
- • Call emergency services (911)
Minutes 5-15:
- • Apply loose constricting band above bite
- • Immobilize extremity with splint
- • Position limb at heart level
- • Monitor vital signs continuously
- • Document all interventions and timing
Signs of Severe Envenomation
Cardiovascular
- • Hypotension
- • Tachycardia
- • Shock symptoms
- • Arrhythmias
Neurological
- • Altered consciousness
- • Ptosis (drooping eyelids)
- • Difficulty swallowing
- • Respiratory paralysis
Hematological
- • Bleeding from bite site
- • Spontaneous bleeding
- • Prolonged clotting
- • Hemolysis signs
Nursing Implementation for Snake Bites
Assessment Priority: Establish baseline measurements within first 5 minutes including vital signs, pain scale, swelling circumference, and neurological status.
Documentation: Record exact time of bite, first aid measures applied, progression of symptoms, and all vital sign measurements with timestamps.
Patient Education: Explain the importance of immobilization, reassure about treatment availability, and prepare family for potential hospital admission.
Preparation for Transport: Ensure IV access if trained, prepare emergency medications, and maintain continuous monitoring during transport.
Animal Bite Management
Animal bites, particularly from dogs and cats, present unique challenges due to their crush-puncture injury pattern and high risk of bacterial contamination. Understanding species-specific considerations is essential for optimal wound management.
Dog Bite Characteristics
- Mechanism: Crush and tear injuries
- Depth: Variable, often deep tissue involvement
- Infection Rate: 5-25% depending on location
- Common Organisms: Staphylococcus, Streptococcus, Pasteurella
- High-Risk Areas: Hand, face, joints, genitals
Cat Bite Characteristics
- Mechanism: Deep puncture wounds
- Depth: Small surface, deep penetration
- Infection Rate: 30-50% (highest risk)
- Common Organisms: Pasteurella multocida (75%)
- Rapid Onset: Infection within 12-24 hours
ANIMAL-CARE Protocol
A – Assess wound depth and contamination
N – Note animal behavior and vaccination status
I – Irrigate wound thoroughly with saline
M – Monitor for signs of infection
A – Apply appropriate dressing
L – Look for foreign material in wound
C – Consider rabies and tetanus prophylaxis
A – Antibiotic prophylaxis evaluation
R – Report to animal control if required
E – Educate patient on wound care
Wound Classification and Management
| Wound Grade | Description | First Aid Approach | Professional Care Needed |
|---|---|---|---|
| Grade I | Superficial abrasion, no bleeding | Gentle cleansing, topical antiseptic | Optional unless high-risk patient |
| Grade II | Puncture/laceration, minimal bleeding | Irrigation, pressure dressing | Recommended within 12 hours |
| Grade III | Deep wound, active bleeding | Direct pressure, immediate transport | Emergency care required |
| Grade IV | Bone/joint involvement, severe tissue damage | Hemostasis, immobilization | Immediate surgical evaluation |
Step-by-Step Management Protocol
Initial Assessment & Control
Wound Cleansing & Documentation
Rabies Risk Assessment
High-Risk Scenarios:
- • Unprovoked attack by wild animal
- • Bat exposure (any contact)
- • Unknown vaccination status of domestic animal
- • Animal exhibits abnormal behavior
- • Animal unavailable for observation
Lower-Risk Scenarios:
- • Provoked attack by healthy domestic animal
- • Current rabies vaccination documented
- • Animal available for 10-day observation
- • Normal animal behavior witnessed
- • Rodent or rabbit bites (rare carriers)
Nursing Implementation for Animal Bites
Assessment Priorities:
Evaluate wound depth using sterile probe if trained, assess neurovascular function distal to injury, photograph wounds for documentation, and obtain detailed history of attack circumstances.
Infection Prevention:
Maintain strict aseptic technique during wound care, educate patient on signs of infection (increased pain, redness, warmth, purulent drainage, red streaking), and emphasize importance of follow-up care.
Patient Education:
Discuss proper wound care techniques, signs requiring immediate medical attention, importance of completing antibiotic courses if prescribed, and strategies for bite prevention in the future.
Insect Bite Management
Insect bites and stings range from minor local reactions to life-threatening systemic anaphylaxis. Understanding the difference between local inflammatory responses and allergic reactions is crucial for appropriate first aid intervention.
Hymenoptera (Bees, Wasps)
- Venom: Histamine, melittin, phospholipase
- Local: Pain, swelling, erythema
- Systemic: Possible anaphylaxis
- Special: Remove stinger if present
Arachnids (Spiders, Ticks)
- Venom: Neurotoxins, cytotoxins
- Local: Variable, may be minimal
- Systemic: Neurological symptoms possible
- Special: Species identification important
Blood Feeders (Mosquitos, Fleas)
- Mechanism: Allergic reaction to saliva
- Local: Itching, papules, wheals
- Systemic: Rare unless mass exposure
- Special: Disease transmission risk
STING Management Protocol
S – Stinger removal (scrape, don’t squeeze)
T – Treatment of local symptoms (ice, elevation)
I – Identify signs of systemic reaction
N – Note time of sting and progression
G – Give antihistamines for local reactions
M – Monitor for anaphylaxis symptoms
A – Activate EMS if systemic symptoms
N – Never ignore respiratory symptoms
Allergic Reaction Classification
| Reaction Type | Symptoms | Onset Time | First Aid Response |
|---|---|---|---|
| Local | Pain, swelling, redness at site (<10cm) | Immediate | Ice, elevation, antihistamines |
| Large Local | Swelling >10cm, may spread to adjacent areas | 2-12 hours | Cold compress, oral antihistamines, monitor |
| Mild Systemic | Generalized urticaria, mild respiratory symptoms | 5-60 minutes | Antihistamines, prepare for escalation |
| Anaphylaxis | Respiratory distress, cardiovascular collapse | 5-30 minutes | Epinephrine, call 911, support ABCs |
Anaphylaxis Recognition
Respiratory
- • Wheezing
- • Stridor
- • Dyspnea
- • Cyanosis
Cardiovascular
- • Hypotension
- • Tachycardia
- • Weak pulse
- • Shock
Dermatologic
- • Generalized urticaria
- • Angioedema
- • Flushing
- • Pruritus
Gastrointestinal
- • Nausea/vomiting
- • Diarrhea
- • Cramping
- • Sense of doom
Specific Management Protocols
Bee/Wasp Sting Protocol
- 1. Stinger Removal:
- • Use credit card edge to scrape
- • Avoid tweezers (may inject more venom)
- • Remove within 30 seconds if possible
- 2. Local Treatment:
- • Apply ice pack for 15-20 minutes
- • Elevate affected extremity
- • Clean area with soap and water
- 3. Symptom Management:
- • Oral antihistamines (diphenhydramine)
- • Topical calamine lotion
- • Monitor for systemic symptoms
Spider Bite Protocol
- 1. Identification Attempt:
- • Note size, color, markings
- • Photograph if safely possible
- • Preserve specimen if available
- 2. Wound Care:
- • Clean with soap and water
- • Apply cold compress
- • Avoid direct ice application
- 3. Monitoring:
- • Watch for necrotic changes
- • Monitor neurological symptoms
- • Seek care for worsening symptoms
Nursing Implementation for Insect Bites
Allergy History Assessment:
Obtain detailed history of previous reactions, current medications (especially ACE inhibitors, beta-blockers), and availability of prescribed epinephrine auto-injectors.
Anaphylaxis Preparedness:
Maintain high index of suspicion for systemic reactions, ensure epinephrine availability, establish IV access in high-risk patients, and prepare for advanced airway management.
Patient Education:
Teach recognition of allergic reaction progression, proper use of epinephrine auto-injectors, avoidance strategies for high-risk individuals, and importance of medical alert identification.
Human Bite Management
Human bites represent one of the highest-risk bite injuries due to the polymicrobial nature of human oral flora and potential for viral transmission. These injuries require aggressive first aid management and prompt professional evaluation.
Why Human Bites Are High-Risk
Microbiology Concerns:
- • 100+ bacterial species in human mouth
- • High concentration of anaerobic bacteria
- • Streptococcus and Staphylococcus predominance
- • Eikenella corrodens (unique to human bites)
- • Infection rate: 10-50% depending on location
Viral Transmission Risk:
- • Hepatitis B and C transmission possible
- • HIV transmission extremely rare but documented
- • Herpes simplex virus transmission
- • CMV and EBV potential transmission
- • Risk increases with visible blood in saliva
Types of Human Bite Injuries
| Bite Type | Mechanism | Common Locations | Complications |
|---|---|---|---|
| Occlusal Bite | True bite with dental impressions | Extremities, trunk, face | Deep tissue damage, infection |
| Clenched Fist | Fist strikes teeth, wounds knuckles | 3rd/4th metacarpophalangeal joints | Joint infection, tendon damage |
| Self-Inflicted | Accidental or intentional self-harm | Tongue, lips, cheek | Usually lower infection risk |
HUMAN-BITE Protocol
H – Halt bleeding with direct pressure
U – Universal precautions mandatory
M – Meticulously irrigate wound
A – Assess depth and tissue involvement
N – Note exact bite pattern and location
B – Blood-borne pathogen consideration
I – Immediate professional evaluation needed
T – Tetanus prophylaxis assessment
E – Emergency department referral always
Immediate First Aid Protocol
Immediate (0-5 min)
- • Don gloves immediately
- • Control bleeding with pressure
- • Do NOT close wound
- • Photograph if possible
Early Care (5-15 min)
- • Copious irrigation with saline
- • Remove visible debris
- • Apply loose sterile dressing
- • Elevate if extremity involved
Transport (15+ min)
- • Arrange immediate transport
- • Gather perpetrator information
- • Document circumstances
- • Reassure patient
Wound Irrigation Technique
Equipment Needed:
- • Sterile saline solution (preferred)
- • 20mL syringe with 18-gauge needle
- • Clean water if saline unavailable
- • Sterile gauze pads
- • Protective eyewear
Irrigation Steps:
- 1. Use high-pressure irrigation (8-12 psi)
- 2. Direct stream into wound depths
- 3. Use minimum 250mL total volume
- 4. Continue until effluent runs clear
- 5. Pat dry with sterile gauze
Blood-Borne Pathogen Protocol
Immediate Actions: Determine if biter’s blood is visible in saliva, assess biter’s risk factors (known HIV, hepatitis status), and document exposure circumstances thoroughly.
Victim Counseling: Explain transmission risks honestly but reassuringly, discuss testing timeline and procedures, and arrange follow-up with infectious disease specialist if indicated.
Legal Considerations: Human bites may involve assault charges, mandatory reporting may be required, and detailed documentation is crucial for legal proceedings.
Nursing Implementation for Human Bites
Priority Assessment:
Evaluate wound depth with particular attention to joint capsule involvement, assess neurovascular function, obtain detailed history including time of injury and circumstances, and photograph wounds before and after cleansing.
Infection Prevention:
Maintain strict universal precautions, perform aggressive wound irrigation, avoid primary closure in most cases, and educate patient on signs of infection requiring immediate return.
Psychosocial Support:
Address patient’s anxiety about infection transmission, provide emotional support for traumatic circumstances, coordinate with social services if domestic violence suspected, and ensure appropriate follow-up care.
Assessment and Documentation
Systematic assessment and thorough documentation are critical components of bite management. Proper documentation serves medical, legal, and quality improvement purposes while ensuring continuity of care.
DOCUMENTATION Mnemonic
D – Date, time, and circumstances of bite
O – Objective wound assessment findings
C – Creature identification if possible
U – Universal precautions used
M – Medications given or recommended
E – Education provided to patient
N – Neurological and vascular assessment
T – Tetanus immunization status
A – Actions taken and patient response
T – Transport arrangements made
I – Instructions for follow-up care
O – Outcome at time of documentation
N – Next steps in care plan
Comprehensive Assessment Framework
Primary Assessment
Airway: Patency, swelling, voice changes
Breathing: Rate, effort, adventitious sounds
Circulation: Pulse, blood pressure, perfusion
Disability: Neurological function, consciousness
Exposure: Full wound visualization, temperature
Secondary Assessment
Wound Characteristics: Size, depth, location, contamination
Neurovascular: Sensation, movement, pulses
Pain Assessment: Intensity, quality, radiation
Functional Impact: Range of motion, strength
Infection Signs: Erythema, warmth, drainage
Wound Assessment Scale
| Assessment Parameter | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|---|
| Tissue Damage | No visible injury | Superficial abrasion | Partial thickness wound | Full thickness to bone/joint |
| Bleeding | None | Minimal oozing | Moderate, easily controlled | Severe, difficult to control |
| Contamination | Clean | Minimal debris | Moderate contamination | Heavily contaminated |
| Infection Risk | Minimal | Low | Moderate | High |
Legal Documentation Requirements
Critical Documentation Elements
Mandatory Information:
- • Exact time and date of injury
- • Precise location of incident
- • Witnesses present (names, contact info)
- • Animal description and ownership
- • Circumstances leading to bite
- • Patient’s account of events
- • Pre-existing medical conditions
Professional Responsibilities:
- • Objective, factual language only
- • Avoid subjective interpretations
- • Include direct quotes when relevant
- • Document all interventions with times
- • Note patient’s response to treatment
- • Record discharge instructions given
- • Sign and date all entries
Photographic Documentation
When to Photograph: All bite wounds should be photographed when possible, with patient consent, using proper medical photography protocols.
Technical Requirements: Use ruler or coin for scale reference, ensure adequate lighting, capture multiple angles, include distant and close-up views, and maintain patient privacy.
Storage and Security: Follow institutional HIPAA guidelines, use secure medical imaging systems, ensure proper patient identifiers, and maintain chain of custody documentation.
Nursing Documentation Standards
Assessment Documentation:
Use consistent terminology and measurement units, document findings in anatomical position reference, include negative findings when relevant, and reassess and document changes over time.
Intervention Documentation:
Record all first aid measures with specific details, document patient education provided and understanding demonstrated, note family involvement and concerns, and include referrals made and appointments scheduled.
Follow-up Documentation:
Plan for systematic reassessment intervals, document patient compliance with instructions, record any complications or concerns reported, and ensure continuity between care providers.
Nursing Implementation in Practice
Nursing professionals play a crucial role in bite management across various healthcare settings. Understanding scope of practice, evidence-based interventions, and collaborative care approaches ensures optimal patient outcomes and professional safety.
Setting-Specific Protocols
Emergency Department
- Triage Priority: ESI Level 2-4 based on systemic symptoms
- Rapid Assessment: ABC evaluation within 5 minutes
- Resource Coordination: Lab studies, radiology, consultation
- Discharge Planning: Follow-up arrangements, prescription coordination
Urgent Care/Clinic
- Screening: Identify cases requiring ED transfer
- Wound Management: Irrigation, debridement, dressing
- Prophylaxis: Tetanus, antibiotics, rabies consideration
- Education: Home care, warning signs, follow-up
Community/Home
- Scene Safety: Environmental hazard assessment
- Basic First Aid: Bleeding control, wound protection
- Decision Making: Transport vs. self-care guidance
- Resource Connection: EMS activation, family support
Evidence-Based Interventions
Research-Supported Practices
Wound Irrigation:
- • High-pressure irrigation reduces infection risk by 40%
- • Minimum 250mL volume for puncture wounds
- • Sterile saline preferred over tap water
- • 8-12 psi optimal pressure for debris removal
Antibiotic Prophylaxis:
- • Indicated for high-risk wounds (hand, immunocompromised)
- • Amoxicillin-clavulanate first-line for animal bites
- • Duration: 3-7 days for prophylaxis
- • Monitor for allergic reactions and resistance
Wound Closure:
- • Primary closure contraindicated for most bite wounds
- • Delayed primary closure at 3-5 days if no infection
- • Facial wounds exception due to cosmetic considerations
- • Loose approximation without tension preferred
Pain Management:
- • Multimodal approach combining pharmacologic/non-pharmacologic
- • Local anesthetics for procedure-related pain
- • NSAIDs effective for inflammatory pain
- • Avoid excessive opioid prescribing
Collaborative Care Team
| Team Member | Primary Responsibilities | When to Involve | Key Communications |
|---|---|---|---|
| Emergency Physician | Medical evaluation, treatment decisions, prescriptions | All ED presentations, complex wounds | Assessment findings, intervention response |
| Surgeon | Operative management, complex reconstructions | Deep wounds, functional impairment, infection | Wound characteristics, neurovascular status |
| Infectious Disease | Antibiotic selection, resistant organisms | Severe infections, immunocompromised patients | Culture results, clinical response |
| Public Health | Disease surveillance, rabies evaluation | Animal bites, potential rabies exposure | Exposure circumstances, animal information |
| Social Services | Abuse evaluation, resource coordination | Suspicious circumstances, vulnerable populations | Injury pattern, social history |
NURSING Excellence in Bite Care
N – Navigate scope of practice appropriately
U – Use evidence-based interventions
R – Recognize complications early
S – Systematically assess and reassess
I – Implement appropriate first aid measures
N – Note all findings and interventions
G – Give clear patient education
E – Ensure appropriate follow-up
X – eXamine for signs of infection
C – Collaborate with healthcare team
E – Evaluate outcomes continuously
Professional Development
Competency Maintenance: Participate in continuing education on wound care advances, maintain certification in first aid and CPR, attend trauma and emergency care workshops, and stay current with evidence-based practice guidelines.
Quality Improvement: Participate in bite management protocol development, contribute to patient outcome tracking, engage in case review and analysis, and advocate for resource allocation and equipment updates.
Leadership Opportunities: Mentor new staff in bite management protocols, lead community education programs, participate in policy development, and contribute to professional nursing organizations.
Complications and Prevention
Understanding potential complications and implementing effective prevention strategies are essential components of comprehensive bite management. Early recognition and prompt intervention can prevent serious morbidity and mortality.
Common Complications by Category
Infectious Complications
Cellulitis (Most Common)
Onset: 24-72 hours. Signs: Erythema, warmth, swelling, pain. Treatment: Antibiotics, elevation, warm compresses.
Abscess Formation
Onset: 3-7 days. Signs: Fluctuant mass, severe pain, fever. Treatment: Incision and drainage, antibiotics.
Septic Arthritis
Onset: 1-5 days. Signs: Joint pain, limited ROM, fever. Treatment: Emergency orthopedic consultation.
Systemic Sepsis
Onset: Variable. Signs: SIRS criteria, altered mental status. Treatment: ICU management, broad-spectrum antibiotics.
Systemic Complications
Anaphylaxis
Onset: Minutes. Signs: Respiratory distress, hypotension, urticaria. Treatment: Epinephrine, IV fluids, steroids.
Coagulopathy (Snake bites)
Onset: Hours. Signs: Bleeding, abnormal clotting studies. Treatment: Antivenom, blood products.
Neurotoxicity
Onset: Variable. Signs: Weakness, paralysis, altered consciousness. Treatment: Supportive care, antivenom.
Compartment Syndrome
Onset: Hours. Signs: Severe pain, tense swelling, paresthesias. Treatment: Emergency fasciotomy.
PREVENT Complications Strategy
P – Prompt and appropriate first aid
R – Recognize high-risk factors early
E – Educate patients on warning signs
V – Vigilant monitoring and follow-up
E – Early intervention when complications arise
N – Never delay definitive care
T – Team approach to complex cases
Prevention Strategies
Primary Prevention
- Animal Safety:
- • Never approach unfamiliar animals
- • Supervise children around pets
- • Maintain pet vaccinations
- • Secure garbage and food sources
- Environmental Awareness:
- • Use protective clothing outdoors
- • Check shoes and clothing
- • Maintain clean living spaces
- • Remove habitat attractants
Secondary Prevention
- Immediate Care:
- • Rapid first aid implementation
- • Appropriate wound cleaning
- • Tetanus prophylaxis
- • Professional evaluation
- Risk Mitigation:
- • Antibiotic prophylaxis when indicated
- • Proper wound dressing
- • Activity modification
- • Close monitoring protocols
Tertiary Prevention
- Complication Management:
- • Early infection recognition
- • Aggressive treatment protocols
- • Specialist consultation
- • Rehabilitation planning
- Long-term Follow-up:
- • Functional assessment
- • Psychological support
- • Prevention education
- • Community resources
High-Risk Patient Populations
| Risk Factor | Increased Complications | Special Considerations | Preventive Measures |
|---|---|---|---|
| Immunocompromised | Severe infections, delayed healing | Lower threshold for antibiotics | Aggressive wound care, close monitoring |
| Diabetes | Poor wound healing, infection | Glucose control, vascular assessment | Meticulous wound care, podiatry referral |
| Peripheral Vascular Disease | Ischemia, delayed healing | Vascular surgery consultation | Avoid tourniquets, optimize perfusion |
| Advanced Age | Frailty, multiple comorbidities | Comprehensive geriatric assessment | Fall prevention, caregiver education |
| Pediatric | Anxiety, compliance issues | Age-appropriate communication | Family education, safety counseling |
Nursing Role in Prevention
Community Education:
Develop and deliver bite prevention programs for schools and community groups, create educational materials for high-risk populations, participate in public health campaigns, and collaborate with animal control and wildlife agencies.
Patient Advocacy:
Advocate for accessible preventive care, support policy development for bite prevention, ensure culturally appropriate education, and address social determinants affecting bite risk.
Quality Improvement:
Track bite injury patterns and outcomes, identify system improvement opportunities, develop evidence-based protocols, and mentor colleagues in prevention strategies.
Memory Aids and Mnemonics
Clinical mnemonics and memory aids enhance retention and recall of critical information during high-stress situations. These tools support systematic thinking and help prevent omission of important assessment or intervention steps.
General Assessment: BITE-SAFE
B – Bleeding control and blood pressure
I – Identify the creature/mechanism
T – Time of injury documentation
E – Evaluate wound characteristics
S – Systemic symptom assessment
A – Antibiotic and tetanus prophylaxis
F – Follow-up care arrangements
E – Education and discharge planning
Emergency Priorities: ABC-BITE
A – Airway patency and protection
B – Breathing assessment and support
C – Circulation and hemorrhage control
B – Bite wound evaluation
I – Immobilization of affected area
T – Transport decision and preparation
E – Emergency interventions implemented
Snake Bite Severity: SNAKE-GRADE
S – Swelling progression and measurement
N – Neurological symptoms present
A – Airway compromise signs
K – Keep monitoring vital signs
E – Extremity neurovascular status
G – GI symptoms (nausea, vomiting)
R – Respiratory effort and rate
A – Altered consciousness level
D – Discoloration and ecchymosis
E – Envenomation syndrome severity
Anaphylaxis Recognition: FAST-HELP
F – Face: angioedema, lip swelling
A – Airway: stridor, voice changes
S – Skin: urticaria, flushing, pruritus
T – Tachycardia and hypotension
H – Help needed: call for assistance
E – Epinephrine administration
L – Lung sounds: wheezing assessment
P – Position: supine with legs elevated
Time-Critical Interventions: “Golden Hour” Priorities
0-5 Minutes
- • Scene safety assessment
- • Primary survey (ABCs)
- • Bleeding control
- • Call for help/EMS
5-15 Minutes
- • Detailed wound assessment
- • Immobilization
- • Vital signs monitoring
- • IV access if trained
15-30 Minutes
- • Transport preparation
- • Documentation
- • Family notification
- • Continuous monitoring
30+ Minutes
- • Hospital notification
- • Reassessment
- • Comfort measures
- • Handoff preparation
Wound Assessment: DEEPER
D – Depth and dimensions measurement
E – Edges: regular vs. irregular
E – Erythema and inflammation signs
P – Perfusion and capillary refill
E – Exudate character and amount
R – Range of motion assessment
Discharge Teaching: CARE-HOME
C – Cleaning techniques and frequency
A – Activity restrictions and modifications
R – Return instructions and warning signs
E – Emergency contact information
H – Hand hygiene importance
O – Over-the-counter pain management
M – Medication compliance education
E – Elevation and rest instructions