First Aid Management of Frostbite & Effects of Heat
Comprehensive Nursing Notes for Emergency Care
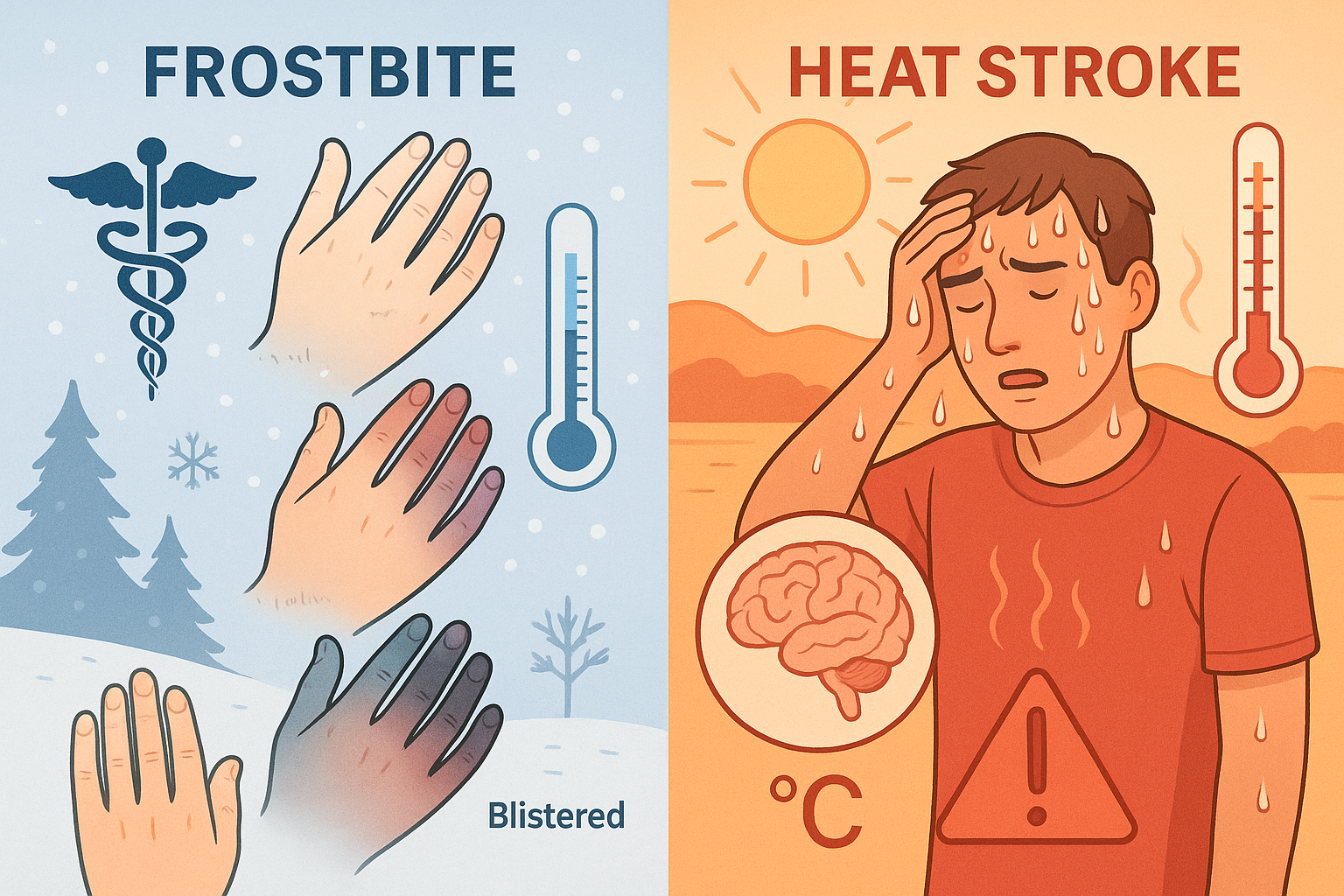
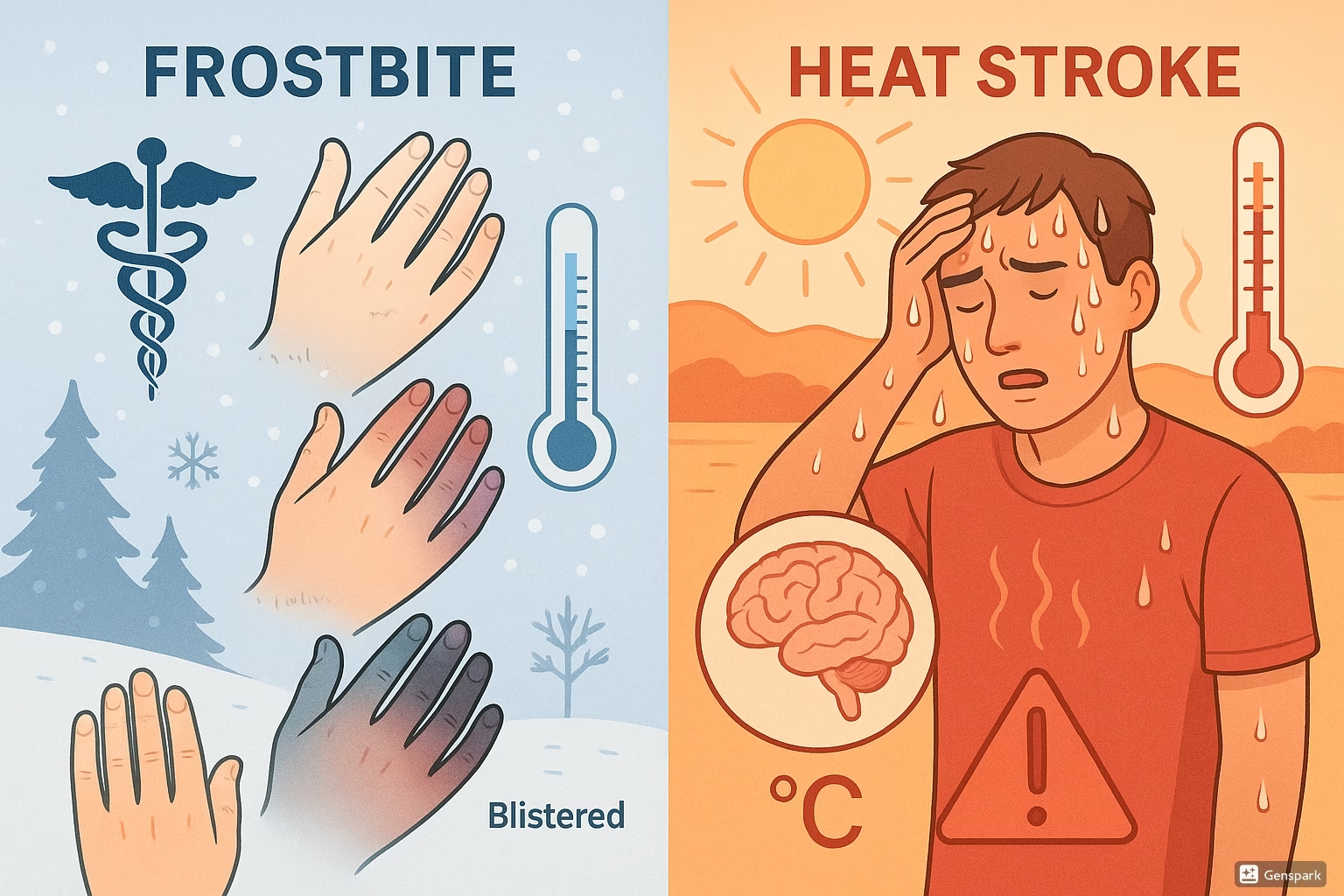
Figure 1: Comparison of frostbite and heat stroke manifestations and pathophysiology
Table of Contents
FROSTBITE MANAGEMENT
FROSTBITE MANAGEMENT
1. Introduction & Pathophysiology
Definition & Mechanism
Frostbite is a freezing cold injury (FCI) that occurs when tissue is exposed to temperatures below 0°C (32°F), resulting in cellular damage through ice crystal formation and vascular compromise.
Pathophysiological Process:
- Phase 1: Vasoconstriction → Reduced blood flow (250 ml/min → 20-50 ml/min)
- Phase 2: Ice crystal formation → Cellular membrane disruption
- Phase 3: Microvascular thrombosis → Tissue ischemia
- Phase 4: Reperfusion injury → Inflammatory cascade
Memory Aid: FROSTBITE Risk Factors
F – Freezing temperatures
R – Recreational exposure
O – Older age/pediatric
S – Substance abuse
T – Tight clothing/footwear
B – Blood vessel disease
I – Immobilization
T – Tobacco use
E – Extremes of weather
2. Classification Systems
Traditional Depth Classification
1st Degree (Superficial)
Numbness, central pallor, erythema, desquamation
2nd Degree (Partial thickness)
Clear blisters, surrounding edema and erythema
3rd Degree (Full thickness)
Hemorrhagic blisters, tissue necrosis
4th Degree (Deep)
Involves muscle, bone; requires amputation
Cauchy Classification (Prognostic)
Grade 1
No cyanosis; no amputation risk
Grade 2
Distal phalanx cyanosis; soft tissue loss
Grade 3
Intermediate/proximal phalanx; bone amputation
Grade 4
Carpal/tarsal involvement; limb amputation
3. Nursing Assessment
Primary Assessment Framework
History Taking
- • Duration of exposure
- • Environmental temperature
- • Wind chill factors
- • Wet vs. dry conditions
- • Previous cold injuries
- • Medication history
Physical Examination
- • Skin color and temperature
- • Capillary refill time
- • Sensation testing
- • Range of motion
- • Pulse assessment
- • Blister characteristics
Systemic Assessment
- • Core body temperature
- • Hypothermia signs
- • Cardiovascular status
- • Neurological function
- • Respiratory status
- • Hydration status
Assessment Mnemonic: COLD HANDS
C – Color (pale, white, blue, mottled)
O – Onset and duration of exposure
L – Location and extent of injury
D – Depth of tissue involvement
H – Hardness and texture of tissue
A – Ability to move affected area
N – Numbness and sensation loss
D – Deformity or swelling present
S – Systemic hypothermia signs
4. First Aid & Emergency Interventions
EMERGENCY PRIORITIES
IMMEDIATE ACTIONS:
- Remove from cold environment
- Assess for hypothermia (PRIORITY)
- Handle affected area gently
- Remove constrictive items
- Protect from further injury
AVOID THESE ACTIONS:
- Rubbing or massaging area
- Direct heat application
- Walking on frostbitten feet
- Thawing if refreezing possible
- Breaking blisters
Rewarming Protocol
Step-by-Step Process:
Critical Points:
Temperature Check: Use thermometer – water should feel warm, not hot
Pain Management: Expect severe pain during rewarming – provide analgesics
Success Indicator: Return of sensation and pink coloration
Stop Criteria: If no improvement after 30 minutes
Post-Rewarming Nursing Care
Wound Care
- • Apply loose, dry dressings
- • Separate digits with gauze
- • Elevate affected extremity
- • Monitor for infection signs
- • Daily dressing changes
Pain Management
- • NSAIDs (ibuprofen preferred)
- • Narcotic analgesics PRN
- • Topical anesthetics
- • Positioning for comfort
- • Monitor pain scores
Monitoring
- • Circulation assessment
- • Sensation testing
- • Temperature monitoring
- • Signs of compartment syndrome
- • Infection surveillance
5. Complications & Prevention
Potential Complications
Immediate (0-7 days)
- • Infection and cellulitis
- • Compartment syndrome
- • Electrolyte imbalances
Long-term (weeks to months)
- • Cold hypersensitivity
- • Phantom pain
- • Arthritis and joint stiffness
- • Growth disturbances (pediatric)
Prevention Strategies
Environmental
- • Layer clothing appropriately
- • Keep extremities dry
- • Avoid tight footwear
- • Limit exposure time
Physiological
- • Maintain hydration
- • Avoid alcohol/smoking
- • Proper nutrition
- • Regular movement
HEAT-RELATED ILLNESS MANAGEMENT
6. Heat Illness Spectrum
Progressive Spectrum of Heat-Related Disorders
Heat Cramps
Muscle spasms in major muscle groups
Core temp: Normal | Mental status: Normal
Heat Exhaustion
Fatigue, weakness, nausea, headache, profuse sweating
Core temp: <40°C | Mental status: May be impaired
Heat Stroke
Life-threatening condition with CNS dysfunction
Core temp: >40°C | Mental status: Always altered
Heat Stroke Recognition: HOT & DRY
H – High temperature (>40°C/104°F)
O – Onset of confusion/altered mental status
T – Tachycardia and hypotension
D – Dry skin (classic) or continued sweating (exertional)
R – Rapid, shallow breathing
Y – Young athletes or elderly at highest risk
7. Pathophysiology & Risk Factors
Thermoregulatory Failure Cascade
Normal Thermoregulation
- • Hypothalamic temperature control center
- • Peripheral vasodilation
- • Increased cardiac output
- • Evaporative cooling via sweating
- • Behavioral adaptations
Heat Stroke Pathophysiology
- • Heat production > heat dissipation
- • Protein denaturation at cellular level
- • Membrane lipid disruption
- • Multiorgan system failure
- • Coagulation cascade activation
Individual Risk Factors
- • Advanced age (>65 years)
- • Pediatric population (<4 years)
- • Chronic medical conditions
- • Dehydration
- • Poor physical conditioning
- • Alcohol/drug use
- • Sleep deprivation
Medication-Related
- • Anticholinergics
- • Beta-blockers
- • Diuretics
- • Phenothiazines
- • Tricyclic antidepressants
- • Antihistamines
- • Stimulants (amphetamines)
Environmental
- • High ambient temperature
- • High humidity (>75%)
- • Poor air circulation
- • Direct sun exposure
- • Intense physical activity
- • Protective equipment/clothing
- • Confined spaces
8. Clinical Assessment
Systematic Assessment Protocol
Primary Survey (ABCs)
- Airway: Assess patency, consider airway protection
- Breathing: Rate, depth, pattern (expect tachypnea)
- Circulation: Heart rate, BP, perfusion status
- Disability: Neurological assessment (GCS)
- Exposure: Core temperature measurement
Secondary Assessment
- Neurological: Confusion, seizures, coma
- Cardiovascular: Dysrhythmias, hypotension
- Respiratory: Hyperventilation, pulmonary edema
- Gastrointestinal: Nausea, vomiting, diarrhea
- Renal: Oliguria, acute kidney injury
Laboratory Investigations
Essential Tests
- • Complete Blood Count (CBC)
- • Comprehensive Metabolic Panel
- • Arterial Blood Gas (ABG)
- • Coagulation studies (PT/PTT)
- • Creatine kinase (CK)
- • Urine myoglobin
Expected Findings
- • Respiratory alkalosis
- • Hypernatremia/normonatremia
- • Elevated liver enzymes
- • Acute kidney injury markers
- • Coagulopathy
Monitoring Parameters
Continuous Monitoring
- • Core temperature (rectal/esophageal)
- • Cardiac rhythm
- • Blood pressure
- • Oxygen saturation
- • Neurological status
- • Urine output
Additional Studies
- • 12-lead ECG
- • Chest X-ray
- • CT head (if indicated)
- • Toxicology screen
9. Emergency Management
RAPID COOLING PROTOCOL – TIME CRITICAL!
Goal: Reduce core temperature by 0.2°C/min to 38-39°C
Ice Water Immersion
GOLD STANDARD
- • Water temperature: 1-15°C
- • Immerse to neck level
- • Fastest cooling method
- • May not be practical in elderly
Evaporative Cooling
PRACTICAL ALTERNATIVE
- • Remove all clothing
- • Spray with lukewarm water
- • Use large fans for air circulation
- • Easier monitoring access
Ice Pack Application
ADJUNCTIVE THERAPY
- • Apply to neck, axillae, groin
- • Target major blood vessels
- • Less effective than immersion
- • Avoid direct skin contact
Concurrent Supportive Management
Cardiovascular Support
- • IV access with large-bore catheters
- • Isotonic crystalloid fluid resuscitation
- • Monitor for fluid overload
- • Vasopressors if hypotensive
- • Correct electrolyte abnormalities
Neurological Management
- • Protect airway if altered mental status
- • Seizure precautions and management
- • Avoid antipyretics (ineffective/harmful)
- • Consider benzodiazepines for agitation
- • Monitor for increased ICP
Heat Stroke Management: COOL FAST
C – Core temperature monitoring
O – Oxygen and airway management
O – Optimize circulation (IV fluids)
L – Laboratory studies (baseline)
F – Fast cooling methods
A – Assess neurological status
S – Stop cooling at 38-39°C
T – Transfer to ICU if severe
10. Nursing Implementation in Practice
Comprehensive Nursing Care Plan
Priority Nursing Diagnoses
Frostbite:
- • Impaired tissue integrity
- • Acute pain
- • Risk for infection
- • Ineffective peripheral perfusion
- • Deficient knowledge
Heat Stroke:
- • Hyperthermia
- • Decreased cardiac output
- • Risk for imbalanced fluid volume
- • Impaired gas exchange
- • Risk for injury
Temperature Management
- • Monitor core temperature continuously
- • Apply cooling/warming measures appropriately
- • Document temperature trends
- • Adjust interventions based on response
- • Prevent temperature overshoot
Cardiovascular Support
- • Monitor vital signs frequently
- • Assess peripheral perfusion
- • Manage fluid balance carefully
- • Watch for dysrhythmias
- • Evaluate response to interventions
Neurological Assessment
- • Perform neurological checks q15min
- • Monitor Glasgow Coma Scale
- • Assess for seizure activity
- • Maintain safe environment
- • Document mental status changes
Critical Documentation Elements
Assessment Findings:
- • Initial and ongoing temperature
- • Skin assessment and changes
- • Neurological status
- • Pain level and characteristics
- • Fluid intake and output
Interventions & Response:
- • Cooling/warming methods used
- • Medications administered
- • Patient response to treatment
- • Family education provided
- • Discharge planning needs
Patient & Family Education Priorities
Prevention Education:
- • Recognize early warning signs
- • Environmental risk awareness
- • Appropriate clothing/hydration
- • Activity modification strategies
- • When to seek medical attention
Home Care Instructions:
- • Wound care techniques (frostbite)
- • Activity restrictions
- • Follow-up appointments
- • Complication recognition
- • Emergency contact information
Quality Care Indicators
Key Takeaways for Nursing Practice
Critical Success Factors
- • Early recognition saves tissue and lives
- • Rapid intervention is time-critical for both conditions
- • Continuous monitoring prevents complications
- • Patient education prevents recurrence
- • Interprofessional collaboration optimizes outcomes
Common Pitfalls to Avoid
- • Don’t rub frostbitten areas
- • Avoid rewarming if refreezing possible
- • Don’t use antipyretics for heat stroke
- • Never ignore altered mental status
- • Don’t stop cooling too early or too late
Evidence-Based References
1. Handford C, Buxton P, Russell K, Imray CE, McIntosh SE, Freer L, et al. Frostbite: a practical approach to hospital management. Extrem Physiol Med. 2014;3:7.
2. McIntosh SE, Freer L, Grissom CK, et al. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Frostbite: 2019 Update. Wilderness Environ Med. 2019;30(4S):S19-S32.
3. Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978-88.
4. Leon LR, Bouchama A. Heat stroke. Compr Physiol. 2015;5(2):611-47.
5. Casa DJ, McDermott BP, Lee EC, Yeargin SW, Armstrong LE, Maresh CM. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35(3):141-9.
6. American Burn Association. Clinical Practice Guidelines on the Treatment of Severe Frostbite. J Burn Care Res. 2024;45(3):541-556.
7. Nursing CE Central. Frostbite Assessment and Treatment. Professional Development Resources. 2023.
8. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Frostbite; Heat Stroke. Available from: https://www.ncbi.nlm.nih.gov/books/