Concepts of Health & Illness/Disease
A Comprehensive Guide for Nursing Students
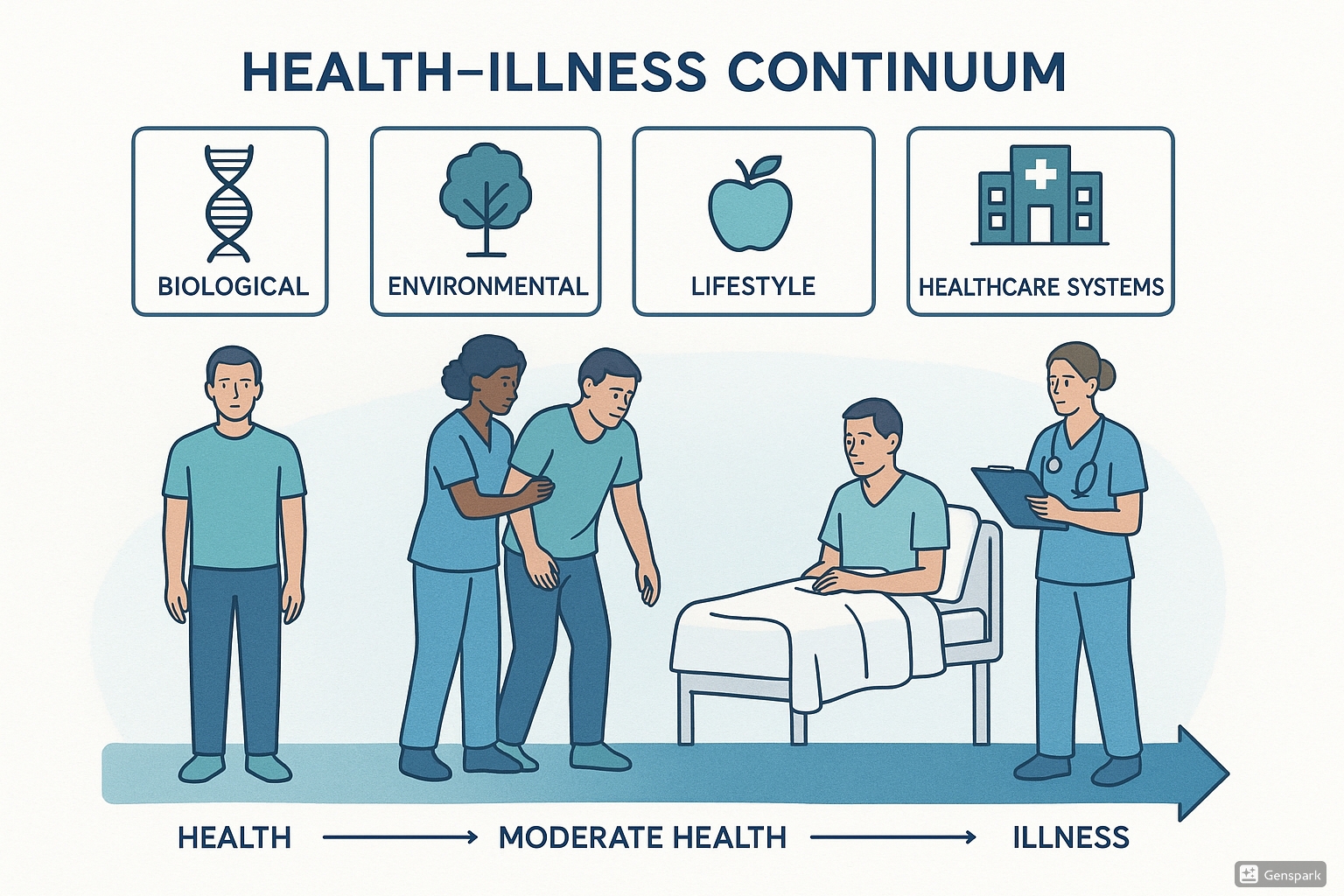
Table of Contents
1. Introduction
Understanding the concepts of health and illness forms the foundation of nursing practice. These concepts shape how we approach patient care, develop treatment plans, and implement interventions. The journey from health to illness and back is not linear but exists on a complex continuum influenced by numerous factors. This comprehensive guide explores these concepts in detail, providing nursing students with a robust framework for understanding health, illness, and disease.
As future healthcare providers, nurses must recognize that their perspective on health and illness directly impacts patient care delivery. A holistic understanding of these concepts enables nurses to:
- Assess patients more comprehensively
- Develop person-centered care plans
- Identify appropriate interventions
- Evaluate outcomes effectively
- Advocate for preventive measures
Throughout history, our understanding of health and disease has evolved significantly. From ancient humoral theories to modern biopsychosocial models, these conceptualizations reflect the scientific knowledge, cultural values, and healthcare priorities of their time. Today’s nursing practice draws on this rich history while incorporating contemporary evidence-based approaches.
2. Definitions of Health and Disease
2.1 Defining Health
Health has been defined in various ways throughout history, reflecting evolving perspectives on human wellbeing. The most widely cited definition comes from the World Health Organization (WHO), established in 1948:
“Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” – World Health Organization (WHO)
This definition marked a significant departure from previous conceptualizations that viewed health simply as the absence of disease. It introduced a holistic perspective that acknowledged multiple dimensions of wellbeing. However, critics have pointed out several limitations:
- The term “complete” sets an unrealistic standard, as few people experience perfect wellbeing in all dimensions
- It doesn’t account for the ability to adapt to physical, mental, and social challenges
- It fails to recognize cultural variations in how health is understood
In response to these criticisms, more dynamic definitions have emerged. For example, Huber et al. (2011) proposed:
“Health as the ability to adapt and self-manage in the face of social, physical, and emotional challenges.”
This conceptualization emphasizes resilience and functionality rather than complete absence of problems. It acknowledges that people with chronic conditions can still experience health through effective adaptation and management.
2.2 Defining Illness and Disease
While often used interchangeably, illness and disease represent distinct concepts:
| Concept | Definition | Focus | Example |
|---|---|---|---|
| Disease | A pathological process with a characteristic set of signs and symptoms that affect the body with known or unknown etiology | Objective, biomedical abnormalities | Hypertension, diabetes mellitus, tuberculosis |
| Illness | The subjective experience of disease or discomfort; how the disease is perceived, lived with, and responded to by individuals and their families | Subjective perception and experience | Feelings of fatigue, pain, emotional distress |
| Sickness | The social role or status accorded to an individual with disease/illness by society | Social recognition and role adjustment | Being excused from work, receiving social support |
These distinctions highlight important considerations for nursing practice:
- A person may have a disease without feeling ill (e.g., early hypertension)
- A person may feel ill without having an identifiable disease (e.g., certain pain syndromes)
- Cultural factors significantly influence how illness is experienced and expressed
Mnemonic: “DIE” Distinction
D – Disease is Diagnosed through objective clinical findings
I – Illness is Individual’s subjective experience
E – External social context shapes how both are recognized (Environment)
3. Dimensions of Health
Health encompasses multiple interconnected dimensions that contribute to overall wellbeing. Understanding these dimensions helps nurses provide holistic care that addresses all aspects of a person’s health status.
Dimensions of Health
3.1 Physical Dimension
The physical dimension encompasses bodily structure and function, including:
- Anatomical integrity
- Physiological functioning
- Physical fitness and energy levels
- Absence of physical disease
- Capacity to perform physical activities of daily living
Physical health is influenced by genetics, lifestyle choices, environmental exposures, and healthcare interventions. Nursing assessments typically begin with evaluation of physical parameters, but should extend beyond to include other dimensions.
3.2 Mental/Psychological Dimension
Mental health involves cognitive and emotional wellbeing, including:
- Cognitive function and clarity
- Emotional regulation and resilience
- Ability to cope with stress
- Self-concept and identity
- Freedom from psychological distress
Mental health significantly impacts overall wellbeing and influences how individuals perceive and respond to physical symptoms. Nurses must assess mental health status alongside physical complaints to develop comprehensive care plans.
3.3 Social Dimension
Social health refers to one’s ability to form relationships and interact effectively with others, including:
- Quality of interpersonal relationships
- Social support networks
- Communication skills
- Community engagement
- Fulfillment of social roles
Social connections significantly impact health outcomes, with strong social support associated with better recovery from illness and increased longevity. Nurses should assess patients’ social resources when planning care.
3.4 Spiritual Dimension
Spiritual health involves finding meaning and purpose in life, which may include but is not limited to religious beliefs:
- Sense of purpose and meaning
- Value system and ethical framework
- Connection to something greater than oneself
- Inner peace and harmony
- Hope and transcendence
Spiritual wellbeing can provide strength during illness and influence treatment decisions. Culturally sensitive nursing care respects spiritual beliefs and incorporates them into holistic care planning.
3.5 Environmental Dimension
Environmental health considers how surroundings impact wellbeing:
- Physical environment (housing, air quality, water safety)
- Occupational environment
- Access to healthcare resources
- Community infrastructure
- Exposure to environmental hazards
Environmental factors can significantly impact health outcomes and must be considered when assessing health status and planning interventions.
Key Point: Health dimensions are interdependent and mutually reinforcing. Changes in one dimension often affect others, highlighting the need for holistic assessment and care planning in nursing practice.
4. Determinants of Health and Disease
Health determinants are factors that influence health status and disease outcomes. Understanding these factors helps nurses identify risk populations, develop targeted interventions, and advocate for health-promoting policies.
4.1 Categories of Health Determinants
Health determinants can be organized into several key categories:
| Category | Examples | Impact on Health | Nursing Considerations |
|---|---|---|---|
| Biological and Genetic Factors | Age, sex, genetic predispositions, family history | Influence susceptibility to disease, response to treatment | Identify genetic risk factors; tailor interventions to age/sex-specific needs |
| Individual Behavior | Diet, physical activity, substance use, sleep habits | Direct impact on risk of chronic disease, injury, and mental health | Provide education and support for behavior change; understand barriers to healthy behaviors |
| Social Environment | Family structure, social networks, cultural practices, socioeconomic status | Affects stress levels, access to resources, health behaviors | Assess social support systems; connect patients with community resources |
| Physical Environment | Housing conditions, pollution, workplace hazards, community design | Exposure to toxins, safety risks, accessibility of health-promoting resources | Identify environmental risks; advocate for safe living/working conditions |
| Health Services | Access to care, quality of services, health insurance coverage | Timeliness of treatment, preventive care utilization, health outcomes | Facilitate access to appropriate care; coordinate services; navigate health systems |
| Policies and Systems | Health policies, economic systems, educational opportunities | Shape distribution of resources and opportunities that affect health | Engage in policy advocacy; recognize systemic barriers to health |
4.2 Social Determinants of Health (SDOH)
Social determinants of health have gained increasing recognition as critical factors shaping health outcomes. The WHO defines SDOH as “the conditions in which people are born, grow, live, work, and age, including the health system.”
Key social determinants include:
- Education: Educational attainment correlates strongly with health outcomes, influencing health literacy, income potential, and health behaviors.
- Income and Wealth: Economic resources affect access to healthcare, nutrition, housing quality, and exposure to stress.
- Employment: Job security, working conditions, and occupational hazards impact both physical and mental health.
- Housing: Housing quality, stability, and affordability influence exposure to environmental hazards and stress.
- Transportation: Ability to access healthcare services, employment, and social connections.
- Food Security: Access to sufficient, nutritious food affects nutritional status and chronic disease risk.
- Social Support: Community connections and relationships buffer against stress and provide practical assistance.
Mnemonic: “HEALTHIER”
Housing conditions
Education access
Access to healthcare
Lifestyle choices
Transportation options
Hereditary factors
Income and employment
Environmental exposures
Relationships and social support
4.3 Health Inequities
Health inequities are avoidable differences in health status between population groups. These differences often reflect deeper social inequalities and power imbalances. Nurses should understand:
- The distinction between health inequalities (measurable differences) and health inequities (unjust differences)
- How social determinants cluster and compound, creating cumulative disadvantage for some populations
- The role of structural racism, sexism, and other forms of discrimination in perpetuating health inequities
- How health systems may inadvertently reinforce disparities through access barriers or bias
5. Natural History of Disease
The natural history of disease describes the progression of a disease process from onset to resolution in the absence of intervention. Understanding this concept helps nurses recognize where in the disease trajectory a patient may be and identify opportunities for prevention or early intervention.
5.1 Stages in the Natural History of Disease
The classic model divides disease progression into several key stages:
Natural History of Disease Flow
Risk factors present but disease not yet developed
Disease process begins but no symptoms appear
Horizon of Clinical Detection
Symptoms and signs become apparent
Recovery and return to health
OR
Persistent health problems
OR
Fatal outcome
5.2 The Iceberg Concept of Disease
The iceberg concept illustrates that the clinically apparent cases of disease (those above the “waterline”) represent only a fraction of the total disease burden in a population. Below the surface are:
- Subclinical cases: Disease is present but not yet producing recognizable symptoms
- Preclinical cases: Pathological changes have begun but are not detectable with current methods
- Susceptible individuals: Those with risk factors but without disease
This concept has important implications for screening programs, early detection initiatives, and preventive interventions. Nurses should recognize that symptoms often represent advanced stages of pathological processes that have been developing over time.
5.3 Spectrum of Disease
For many conditions, disease manifestation exists on a spectrum from mild to severe. The concept of disease spectrum encompasses:
- Variations in symptom presentation and severity
- Different disease phenotypes or subtypes
- Range of complications and sequelae
- Variations in individual response to the same pathogen or process
Understanding disease spectrum helps nurses recognize atypical presentations and individualize care based on where a patient falls on the continuum of disease severity.
5.4 Levels of Prevention
Prevention strategies can be implemented at different points in the natural history of disease:
| Level | Stage in Natural History | Goal | Examples |
|---|---|---|---|
| Primary Prevention | Susceptibility | Prevent disease onset | Immunizations, health education, smoking cessation |
| Secondary Prevention | Subclinical/Early Clinical | Early detection and prompt intervention | Screening programs, regular check-ups, case finding |
| Tertiary Prevention | Clinical/Resolution/Chronic | Minimize complications and disability | Rehabilitation, disease management programs |
| Quaternary Prevention | Any stage | Prevent overdiagnosis and overtreatment | Avoiding unnecessary tests, evidence-based protocols |
Mnemonic: “The Four P’s of Prevention”
Primary: Protect before disease begins
Secondary: Spot disease early
Tertiary: Treat complications and rehabilitate
Quaternary: Question unnecessary interventions
6. Implementation in Nursing Practice
Understanding the concepts of health, illness, and disease provides the theoretical foundation for nursing practice. This knowledge informs every aspect of the nursing process and shapes the delivery of holistic patient care.
6.1 Application to Nursing Assessment
Comprehensive nursing assessment goes beyond physical symptoms to evaluate all dimensions of health:
Holistic Assessment Framework
- Physical assessment: Systematic examination of body systems, vital signs, functional abilities
- Psychological assessment: Mental status, emotional wellbeing, coping strategies, stress levels
- Social assessment: Support systems, relationship dynamics, social roles, cultural factors
- Spiritual assessment: Sources of meaning/purpose, religious practices, existential concerns
- Environmental assessment: Home environment, occupational exposures, community resources
- Health determinants assessment: Identifying risk factors and health barriers
When conducting assessments, nurses should:
- Consider both objective findings and subjective experiences
- Assess for both disease (pathological processes) and illness (personal experience)
- Identify where patients are in the natural history of disease
- Recognize how social determinants impact the patient’s health status
- Document both strengths/resources and challenges/deficits
6.2 Nursing Diagnosis and Planning
Nursing diagnoses should reflect holistic understanding of health and illness:
| Health Concept | Nursing Diagnosis Examples | Planning Considerations |
|---|---|---|
| Physical Dimension | Impaired Physical Mobility, Acute Pain, Ineffective Breathing Pattern | Address physiological needs; restore functional abilities; manage symptoms |
| Psychological Dimension | Anxiety, Disturbed Body Image, Ineffective Coping | Support emotional adjustment; provide therapeutic communication; enhance coping strategies |
| Social Dimension | Social Isolation, Ineffective Role Performance, Interrupted Family Processes | Strengthen support systems; facilitate role adaptation; promote healthy relationships |
| Spiritual Dimension | Spiritual Distress, Risk for Spiritual Distress, Readiness for Enhanced Spiritual Wellbeing | Support meaning-making; respect religious practices; address existential concerns |
| Health Determinants | Deficient Knowledge, Ineffective Health Management, Readiness for Enhanced Health Management | Address modifiable risk factors; enhance health literacy; connect to resources |
6.3 Nursing Interventions Across the Health-Illness Continuum
Nursing interventions vary based on where patients are in the health-illness continuum:
Intervention Framework
- Health promotion: Education on healthy lifestyle, stress management techniques, preventive health measures
- Health protection: Immunizations, safety measures, risk reduction strategies
- Disease prevention: Screening activities, early case finding, risk assessment
- Acute care: Symptom management, treatment administration, monitoring for complications
- Restoration: Rehabilitation interventions, adaptation assistance, recovery support
- Palliative care: Comfort measures, symptom relief, end-of-life support
Effective nurses tailor interventions to address:
- The specific stage in the natural history of disease
- Individual determinants of health affecting the patient
- Cultural factors influencing health perceptions and practices
- Available resources and support systems
6.4 Patient Education
Health education is a core nursing responsibility and should reflect comprehensive understanding of health concepts:
- Health literacy assessment: Evaluate patients’ ability to obtain, process, and understand health information
- Personalized education: Tailor information to patients’ knowledge level, cultural background, and learning preferences
- Self-management support: Build skills for disease management and health maintenance
- Empowerment approach: Foster patients’ sense of control and self-efficacy
- Addressing determinants: Provide resources to overcome barriers related to social determinants
Key Point: Effective patient education acknowledges the patient’s explanatory model of illness—their understanding of what caused their condition, how it works, what treatments are appropriate, and what outcomes they expect.
6.5 Advocacy and System Change
Nurses’ understanding of health determinants positions them as advocates for healthier environments and policies:
- Individual advocacy: Ensuring patients receive appropriate care; navigating health systems
- Community advocacy: Addressing environmental health hazards; improving community resources
- Policy advocacy: Supporting health-promoting policies; addressing structural inequities
- Interdisciplinary collaboration: Working with other sectors (housing, education, etc.) to address determinants
Nurses can contribute to health-promoting systems by:
- Participating in quality improvement initiatives
- Developing evidence-based protocols
- Implementing screening programs
- Designing health promotion programs
- Advocating for vulnerable populations
7. Preventive Strategies in Healthcare
Prevention is a cornerstone of modern healthcare, aiming to intervene before disease occurs or progresses. Nurses play a vital role in implementing preventive strategies across all levels of care.
7.1 Primary Prevention Strategies
Primary prevention aims to prevent disease before it occurs by reducing risk factors and enhancing protective factors:
| Strategy | Examples | Nursing Role |
|---|---|---|
| Health Education | Nutrition counseling, smoking cessation, physical activity promotion | Provide evidence-based information; tailor education to individual needs; use motivational interviewing |
| Immunization | Childhood vaccines, influenza vaccination, travel immunizations | Administer vaccines; educate about benefits; address concerns and misconceptions |
| Environmental Interventions | Water purification, air quality improvement, workplace safety measures | Identify environmental risks; advocate for healthy environments; teach safety practices |
| Lifestyle Modifications | Stress management techniques, healthy diet adoption, regular exercise routines | Assess readiness for change; assist with goal setting; provide ongoing support |
| Chemical Prophylaxis | Fluoride supplementation, malaria prophylaxis, pre-exposure HIV prevention | Provide information on appropriate use; monitor for side effects; ensure adherence |
7.2 Secondary Prevention: Screening and Early Detection
Secondary prevention focuses on early disease detection when treatment is more effective:
- Screening principles: Target conditions with significant burden; use reliable screening tests; ensure follow-up capacity
- Common screening programs: Blood pressure monitoring, mammography, cervical cancer screening, diabetes screening
- Risk assessment tools: Cardiovascular risk calculators, falls risk assessments, depression screenings
- Case finding: Targeted assessment of high-risk individuals; opportunistic screening during routine visits
Key Point: Effective secondary prevention requires both the identification of disease/risk AND timely intervention. Nurses must ensure appropriate follow-up for abnormal findings.
7.3 Tertiary Prevention: Management and Rehabilitation
Tertiary prevention aims to reduce the impact of established disease by limiting complications and disability:
- Disease management programs: Structured approaches to chronic conditions like diabetes, heart failure, COPD
- Rehabilitation services: Physical therapy, occupational therapy, speech therapy, cardiac rehabilitation
- Self-management support: Teaching symptom monitoring, medication management, lifestyle modifications
- Complication prevention: Pressure injury prevention, fall prevention, infection control measures
- Adaptive strategies: Assistive devices, environmental modifications, compensatory techniques
8. Case Studies
Case Study 1: Type 2 Diabetes – A Perspective on Health Determinants
Patient Profile: Maria, a 52-year-old Hispanic woman recently diagnosed with Type 2 diabetes.
Multiple Determinants Analysis:
- Biological determinants: Family history of diabetes (mother and sister); age; female sex
- Behavioral determinants: Sedentary job; limited physical activity; diet high in processed foods
- Social determinants: Works two jobs with irregular hours; limited time for meal preparation; financial stress
- Environmental determinants: Lives in a neighborhood with few grocery stores; limited safe spaces for exercise
- Healthcare access: No health insurance; relies on emergency department for care; language barriers
Natural History Analysis:
- Susceptibility stage: Family history, ethnicity, and lifestyle created risk factors
- Subclinical stage: Insulin resistance and beta-cell dysfunction developed over years
- Clinical manifestation: Diagnosed after presenting with symptoms of polyuria, polydipsia
- Current stage: Early clinical disease with potential to prevent complications
Nursing Implementation:
- Assessment: Comprehensive evaluation of all health dimensions; identify barriers to self-management
- Planning: Develop culturally appropriate care plan addressing social determinants
- Interventions:
- Connect with community health worker for language-concordant education
- Provide simple meal planning strategies compatible with work schedule
- Link to medication assistance programs
- Teach self-monitoring skills
- Connect with community resources (food assistance, exercise programs)
- Prevention focus: Secondary prevention (preventing complications) and tertiary prevention (managing disease)
Case Study 2: Community Health Assessment – A Population Perspective
Community Profile: A rural community with aging population and limited healthcare resources.
Health Status Assessment:
- High prevalence of chronic conditions (hypertension, COPD, arthritis)
- Limited preventive care utilization
- Higher-than-average mortality from preventable causes
- Mental health concerns, particularly depression and isolation among elderly
Determinant Analysis:
- Healthcare access: Shortage of providers; distant specialty care; limited public transportation
- Economic factors: Declining local economy; fixed incomes; high poverty rates
- Social factors: Outmigration of younger residents; weakened social networks
- Environmental factors: Limited walkability; harsh winter conditions; aging housing stock
Public Health Nursing Implementation:
- Primary prevention:
- Community-based exercise programs for seniors
- Health education through local organizations
- Home safety assessments to prevent falls
- Secondary prevention:
- Mobile screening clinics for blood pressure, diabetes, cancer
- Depression screening at community events
- Telehealth initiatives for early intervention
- Systems approach:
- Developing volunteer transportation network
- Creating community health worker program
- Advocating for rural health policy improvements
- Building partnerships with regional healthcare systems
9. Summary and Key Takeaways
Core Concepts Review
- Health is multidimensional – encompassing physical, mental, social, spiritual, and environmental aspects that interact dynamically.
- Disease and illness are distinct concepts – disease refers to objective pathological processes while illness represents subjective experiences.
- Health determinants are complex and interconnected – including biological, behavioral, social, environmental, and systemic factors that collectively shape health outcomes.
- The natural history of disease follows predictable patterns – from susceptibility through subclinical changes to clinical manifestation and ultimate outcomes.
- Prevention operates at multiple levels – primary (preventing disease onset), secondary (early detection), tertiary (minimizing complications), and quaternary (preventing overtreatment).
- Nursing practice applies these concepts – through holistic assessment, comprehensive planning, and interventions that address all dimensions of health and illness.
- Health inequities reflect social injustice – requiring nursing awareness and advocacy to address underlying social determinants and structural barriers.
Implications for Nursing Practice
Understanding the concepts of health and illness equips nurses to:
- Provide truly holistic care that addresses all dimensions of health
- Recognize how social and environmental factors shape health experiences
- Identify opportunities for prevention at all levels of the healthcare continuum
- Advocate effectively for individuals, communities, and populations
- Collaborate across disciplines to address complex health determinants
- Support patient empowerment through enhanced health literacy and self-management
- Contribute to healthcare systems that promote health equity and accessibility
Mnemonic: “HEALTH CARE”
Holistic assessment of all health dimensions
Equity focus to address determinants and disparities
Advocacy for individuals and communities
Lifecourse perspective on health development
Timely interventions at all prevention levels
Health promotion integrated into all care
Culturally responsive approaches
Adaptation support during illness transitions
Resilience building for patients and communities
Evidence-based practice grounded in health science
Continuing Professional Development
Nurses should continually develop their understanding of health and illness concepts by:
- Following emerging research on social determinants of health
- Engaging with interdisciplinary perspectives on health and illness
- Exploring diverse cultural understandings of health and healing
- Reflecting on how personal values and beliefs influence care delivery
- Participating in population health initiatives that address upstream factors
- Advocating for health-promoting policies in healthcare and beyond
References
- Huber, M., Knottnerus, J. A., Green, L., et al. (2011). How should we define health? BMJ, 343, d4163.
- Marmot, M., & Allen, J. J. (2014). Social determinants of health equity. American Journal of Public Health, 104(S4), S517-S519.
- McEwen, M., & Wills, E. M. (2018). Theoretical basis for nursing (5th ed.). Lippincott Williams & Wilkins.
- Kleinman, A. (1988). The illness narratives: Suffering, healing, and the human condition. Basic Books.
- World Health Organization. (1948). Constitution of the World Health Organization. Geneva: WHO.
- World Health Organization. (2010). A conceptual framework for action on the social determinants of health. Geneva: WHO.
- Fawcett, J. (2017). Applying conceptual models of nursing: Quality improvement, research, and practice. Springer Publishing Company.
- Braveman, P., & Gottlieb, L. (2014). The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports, 129(Suppl 2), 19-31.
- Nutbeam, D. (2008). The evolving concept of health literacy. Social Science & Medicine, 67(12), 2072-2078.
- Pender, N. J., Murdaugh, C. L., & Parsons, M. A. (2015). Health promotion in nursing practice (7th ed.). Pearson.
