Structure and Classification of Microbes
Comprehensive Nursing Guide to Microbiology
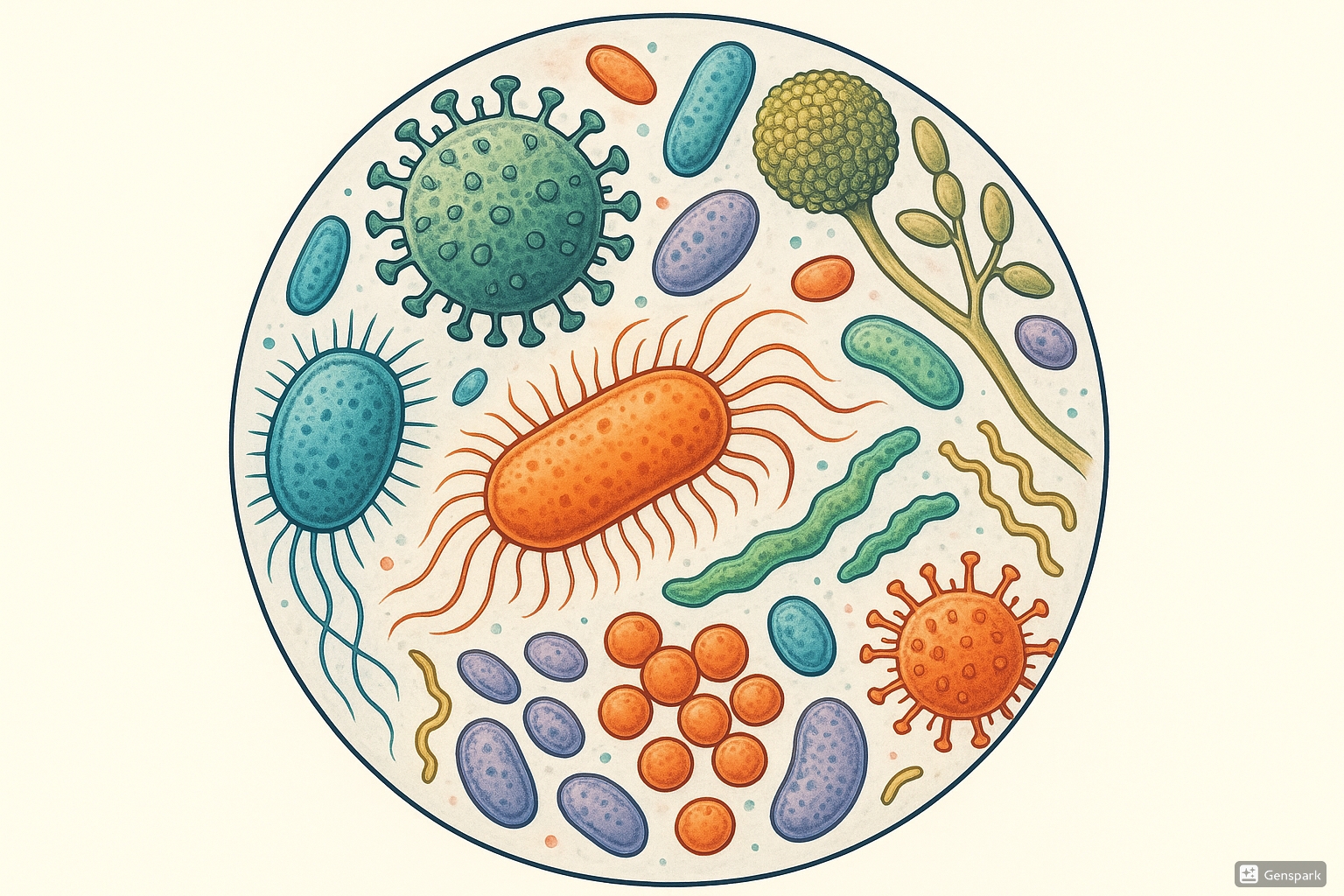
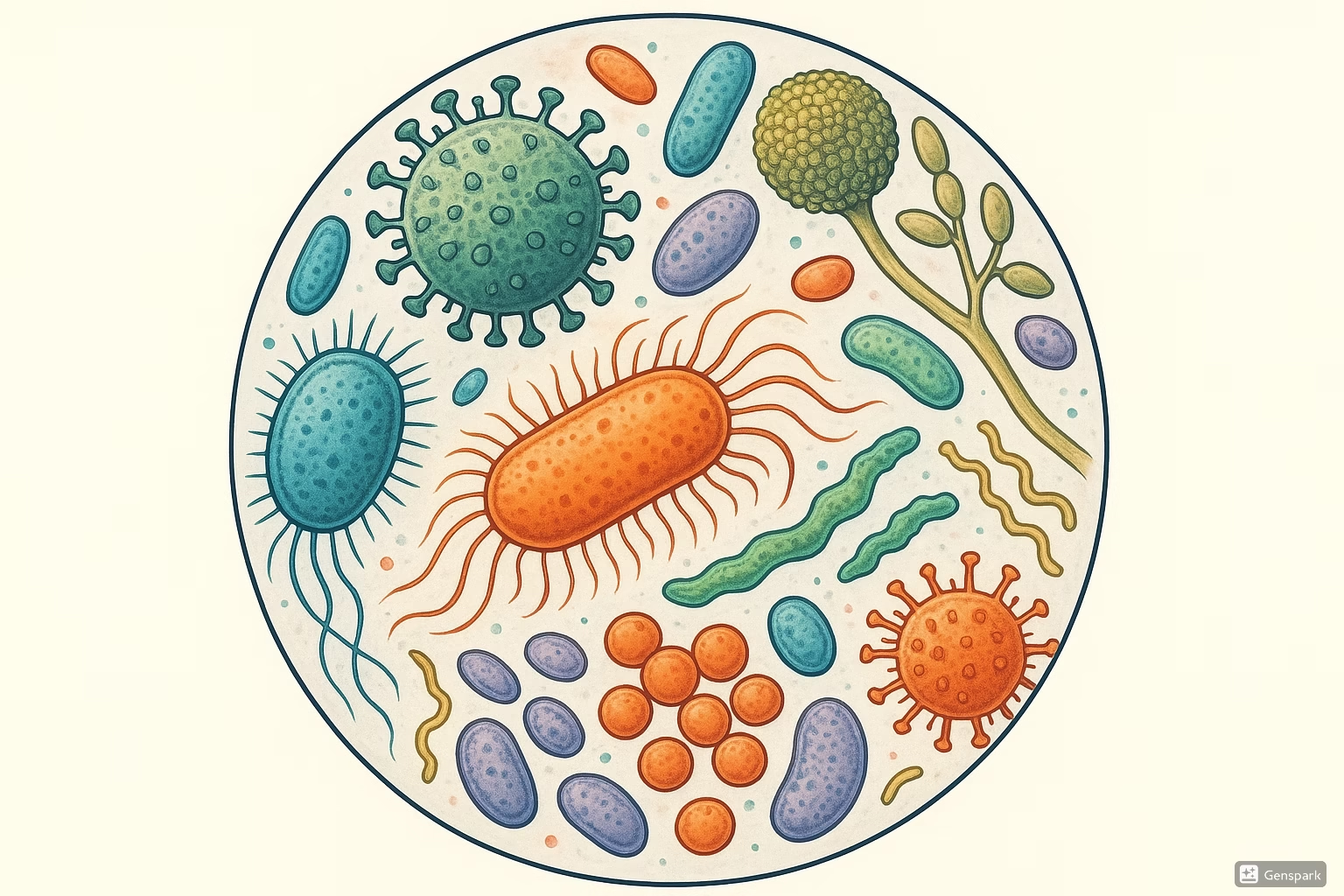
Microscopic view of various microorganisms including bacteria, viruses, and fungi showing their diverse structures and morphologies.
Table of Contents
- 1. Introduction to Microbiology
- 2. Classification of Microorganisms
- 3. Morphological Types of Microorganisms
- 4. Size and Form of Bacteria
- 5. Microbial Motility
- 6. Microbial Colonization
- 7. Growth and Nutrition of Microbes
- 8. Environmental Factors Affecting Microbial Growth
- 9. Nursing Implications and Clinical Applications
1. Introduction to Microbiology
Microbiology is the study of microorganisms, which are living organisms too small to be seen with the naked eye. These include bacteria, viruses, fungi, protozoa, algae, and helminths. As nursing professionals, understanding microbiology is crucial for preventing infections, administering appropriate treatments, and educating patients about disease processes.
Key Concept
Microorganisms are ubiquitous in our environment and play vital roles in maintaining ecological balance. While many microbes are beneficial or harmless, some can cause disease (pathogens). The balance between beneficial and harmful microbes is crucial for human health.
Microorganisms were first observed by Anton van Leeuwenhoek in the late 17th century using simple microscopes. Since then, our understanding of microbial life has expanded dramatically, revealing the complexity and diversity of these organisms that inhabit every corner of our planet, including our own bodies.
The human body hosts approximately 100 trillion microorganisms, collectively known as the human microbiome. These microorganisms outnumber human cells by a ratio of about 10:1 and play crucial roles in nutrition, immunity, and protection against pathogens.
2. Classification of Microorganisms
2.1 Taxonomic Classification
Taxonomy is the science of classifying living organisms. The hierarchical classification system organizes organisms from general to specific categories:
Mnemonic: “King Phillip Came Over For Great Spaghetti”
This helps remember the taxonomic hierarchy:
- Kingdom
- Phylum
- Class
- Order
- Family
- Genus
- Species
Microorganisms are named using a binomial nomenclature system, where the first part indicates the genus and the second part indicates the species. For example, Escherichia coli (commonly abbreviated as E. coli).
2.2 The Three Domains of Life
Modern biological classification divides all living organisms into three domains:
| Domain | Characteristics | Examples |
|---|---|---|
| Bacteria | Prokaryotic cells, single circular chromosome, peptidoglycan cell walls | Staphylococcus, Streptococcus, Escherichia |
| Archaea | Prokaryotic cells, unique membrane lipids, no peptidoglycan, often found in extreme environments | Methanococcus, Sulfolobus, Thermococcus |
| Eukarya | Eukaryotic cells with membrane-bound organelles and nucleus | Fungi, protozoa, algae, plants, animals |
Important Note: Viruses are not included in this classification system as they are not considered living organisms in the traditional sense. They lack cellular structure, cannot reproduce independently, and do not have their own metabolism.
Based on their pathogenic potential, microorganisms can be classified as:
- Pathogens: Microorganisms capable of causing disease
- Opportunistic pathogens: Normally non-pathogenic microorganisms that cause disease in immunocompromised hosts
- Non-pathogens: Microorganisms that do not cause disease
- Commensals: Microorganisms that live on or in the host without causing harm
- Mutualists: Microorganisms that form mutually beneficial relationships with the host
3. Morphological Types of Microorganisms
3.1 Bacterial Morphology
Bacteria exhibit three main morphological forms:
| Morphology | Description | Examples |
|---|---|---|
| Cocci (spherical) | Round or oval-shaped bacteria that can arrange in various patterns |
|
| Bacilli (rod-shaped) | Elongated, cylindrical bacteria that can be short, long, or curved |
|
| Spirilla (spiral) | Bacteria with twisted, corkscrew, or curved shapes |
|
Mnemonic: “CBS” – Bacterial Shapes
- Cocci – Coffee beans (round)
- Bacilli – Bread sticks (rod-shaped)
- Spirilla – Spiral pasta (twisted)
Some bacteria have specialized structures:
- Pleomorphic bacteria: Can change their shape (e.g., Mycoplasma)
- Filamentous bacteria: Form long filaments (e.g., Actinomyces)
- Stalked bacteria: Have extensions called stalks (e.g., Caulobacter)
- Appendaged bacteria: Have appendages (e.g., Ancalomicrobium)
3.2 Viral Morphology
Viruses are much smaller than bacteria and consist of genetic material (DNA or RNA) surrounded by a protein coat called a capsid. Some viruses also have a lipid envelope.
Based on their shape, viruses can be classified as:
- Icosahedral: 20-sided symmetrical structures (e.g., Adenovirus, Poliovirus)
- Helical: Coiled nucleic acid with protein coating (e.g., Influenza virus, Tobacco mosaic virus)
- Complex: Combination of different symmetries or unique shapes (e.g., Bacteriophages with head and tail)
- Envelope: Presence of lipid bilayer derived from host cell membranes (e.g., HIV, Herpes viruses)
Key Concept
Viruses are obligate intracellular parasites, meaning they can only replicate inside host cells by hijacking cellular machinery. This property makes viral infections challenging to treat without affecting host cells.
3.3 Fungal Morphology
Fungi are eukaryotic organisms that can exist in two basic morphological forms:
- Yeasts: Unicellular fungi that reproduce by budding (e.g., Candida albicans, Saccharomyces cerevisiae)
- Molds/Filamentous fungi: Multicellular fungi that grow as branching, thread-like structures called hyphae, which collectively form a mycelium (e.g., Aspergillus, Penicillium)
- Dimorphic fungi: Can exist as either yeast or mold depending on environmental conditions (e.g., Histoplasma capsulatum, Blastomyces dermatitidis)
Fungal cell walls contain chitin, a polysaccharide not found in plant or bacterial cell walls. This unique composition makes fungi susceptible to different antimicrobial agents than bacteria.
3.4 Protozoal Morphology
Protozoa are single-celled eukaryotic microorganisms that can be classified based on their locomotion method:
- Amoebae: Move using pseudopodia (temporary extensions of cytoplasm) (e.g., Entamoeba histolytica)
- Flagellates: Move using whip-like structures called flagella (e.g., Giardia lamblia, Trichomonas vaginalis)
- Ciliates: Move using hair-like structures called cilia (e.g., Paramecium)
- Sporozoans: Non-motile as adults, form spores during reproduction (e.g., Plasmodium species, which cause malaria)
Nursing Application
When collecting stool samples for protozoa identification, nurses should ensure specimens are fresh or properly preserved. Trophozoites (active feeding stage) degrade quickly, while cysts (dormant stage) remain viable longer. Proper sample handling is crucial for accurate diagnosis.
4. Size and Form of Bacteria
4.1 Basic Shapes and Arrangements
Bacterial size typically ranges from 0.2 to 2.0 micrometers (μm) in diameter for cocci, and 0.5 to 5.0 μm in length for bacilli. For comparison, human red blood cells are approximately 7-8 μm in diameter.
Bacterial Shapes and Arrangements
COCCI (Spherical) BACILLI (Rod-shaped) SPIRILLA (Spiral)
├── Single (Micrococcus) ├── Single (E. coli) ├── Vibrio (comma)
├── Pairs (Diplococci) ├── Pairs (Diplobacilli) ├── Spirilla (rigid spiral)
│ └── Streptococcus pneumoniae │ └── Klebsiella pneumoniae │ └── Campylobacter
├── Chains (Streptococci) ├── Chains (Streptobacilli) └── Spirochetes (flexible)
│ └── Streptococcus pyogenes │ └── Bacillus anthracis └── Treponema pallidum
├── Clusters (Staphylococci) ├── Palisades (Corynebacterium)
│ └── Staphylococcus aureus └── Coccobacilli (Haemophilus)
├── Tetrads (Micrococcus)
└── Cubes/Sarcinae (Sarcina)
The size and shape of bacteria are determined by their cell wall and cytoskeleton components. The bacterial cell wall provides structural support, maintains cell shape, and prevents osmotic lysis in hypotonic environments.
4.2 Cell Wall Structure and Gram Staining
The Gram stain is a differential staining technique used to classify bacteria into two groups based on their cell wall composition:
| Characteristic | Gram-Positive Bacteria | Gram-Negative Bacteria |
|---|---|---|
| Cell Wall Thickness | Thick (20-80 nm) | Thin (8-12 nm) |
| Peptidoglycan Layer | Thick (multiple layers) | Thin (single layer) |
| Outer Membrane | Absent | Present |
| Lipopolysaccharide (LPS) | Absent | Present (endotoxin) |
| Teichoic Acids | Present | Absent |
| Periplasmic Space | Minimal or absent | Present |
| Gram Stain Appearance | Purple/Blue | Pink/Red |
| Examples | Staphylococcus, Streptococcus, Bacillus, Clostridium | Escherichia, Pseudomonas, Salmonella, Neisseria |
Mnemonic: “POP LESS” – Gram-Positive vs. Gram-Negative
Purple – Gram-Positive
One membrane only (no outer membrane)
Peptidoglycan thick
Lipopolysaccharide absent
Endotoxin absent
Simple structure
Susceptible to penicillins (generally)
Some bacteria lack a cell wall entirely (e.g., Mycoplasma) or have modified cell walls that do not respond typically to Gram staining (e.g., Mycobacteria, which require acid-fast staining).
Nursing Application
Understanding Gram staining characteristics helps nurses anticipate the empiric antibiotic choices physicians may make before culture results are available. For example, many β-lactam antibiotics target peptidoglycan synthesis and are more effective against Gram-positive bacteria with their thick peptidoglycan layer.
5. Microbial Motility
5.1 Flagellar Movement
Flagella are thin, whip-like appendages that provide locomotion for many bacteria. They are composed primarily of the protein flagellin and extend from the bacterial cell surface.
Based on the number and arrangement of flagella, bacteria can be classified as:
- Monotrichous: Single flagellum at one end (e.g., Vibrio cholerae)
- Lophotrichous: Multiple flagella at one end (e.g., Pseudomonas fluorescens)
- Amphitrichous: Flagella at both ends (e.g., Spirillum volutans)
- Peritrichous: Flagella all over the surface (e.g., Escherichia coli, Salmonella typhi)
Mnemonic: “FLAP” – Flagellar Arrangements
Flagellum: Monotrichous (one)
Lophotrichous (tuft at one end)
Amphitrichous (at both ends)
Peritrichous (all around)
Flagellar motility allows bacteria to:
- Move toward nutrients (chemotaxis)
- Escape harmful substances
- Disperse to new environments
- Increase pathogenicity by enabling invasion of host tissues
5.2 Other Forms of Microbial Movement
Axial Filaments (Endoflagella): Spirochetes like Treponema pallidum (causative agent of syphilis) have flagella wrapped around their cell body between the cell membrane and outer sheath, giving them a corkscrew-like motion.
Gliding Motility: Some bacteria (e.g., Myxococcus, Cytophaga) can move across solid surfaces without visible appendages through secretion of slime or by using focal adhesion complexes.
Twitching Motility: Mediated by type IV pili that extend, attach to a surface, and then retract, pulling the bacterium forward (e.g., Pseudomonas aeruginosa, Neisseria gonorrhoeae).
Swimming Motility: Bacteria with flagella can swim through liquid environments. The flagella rotate like propellers, driven by a molecular motor at the base.
Key Concept
Bacterial motility tests, such as the “hanging drop” method or motility agar, are used in clinical laboratories to help identify bacterial species. Motility can also be a virulence factor, allowing pathogens to spread within host tissues.
6. Microbial Colonization
6.1 Biofilm Formation
Biofilms are complex communities of microorganisms attached to surfaces and embedded in a self-produced extracellular polymeric substance (EPS) matrix. This lifestyle offers several advantages to the microbes:
Stages of Biofilm Formation
1. Initial Attachment 2. Irreversible 3. Maturation I 4. Maturation II 5. Dispersion
(reversible) Attachment (early) (late)
↓ ↓ ↓ ↓ ↓
Planktonic cells → Surface adhesion → Microcolony → EPS production → Mature biofilm → Cell release
formation 3D structure
Biofilms are clinically significant because they:
- Increase resistance to antimicrobial agents (up to 1,000 times more resistant)
- Protect against host immune defenses
- Allow bacterial communication through quorum sensing
- Enable nutrient capture and metabolic cooperation
- Contribute to persistent and chronic infections
Common examples of biofilm-associated infections include:
- Dental plaque (leading to caries and periodontal disease)
- Catheter-associated urinary tract infections
- Chronic wounds
- Cystic fibrosis lung infections (particularly with Pseudomonas aeruginosa)
- Prosthetic joint infections
- Endocarditis
6.2 The Human Microbiome
The human microbiome refers to all microorganisms living on and inside the human body. Different body sites harbor distinct microbial communities adapted to local conditions:
| Body Site | Predominant Microorganisms | Functions |
|---|---|---|
| Skin | Staphylococcus epidermidis, Propionibacterium acnes, Malassezia species | Prevent colonization by pathogens, modulate immune responses |
| Oral Cavity | Streptococcus species, Actinomyces, Veillonella, Fusobacterium | Aid in initial food digestion, protect against pathogens |
| Gastrointestinal Tract | Bacteroides, Prevotella, Bifidobacterium, Lactobacillus, Escherichia | Aid digestion, produce vitamins, train immune system, prevent pathogen colonization |
| Respiratory Tract | Streptococcus, Haemophilus, Corynebacterium, Neisseria | Prevent pathogen adherence, modulate local immunity |
| Urogenital Tract | Lactobacillus species (in vagina), Corynebacterium, Staphylococcus | Maintain acidic pH (vagina), prevent pathogen colonization |
Nursing Application
Broad-spectrum antibiotics can disrupt the normal microbiota, leading to secondary infections like Clostridioides difficile colitis or vaginal candidiasis. Nurses should educate patients about these potential complications and monitor for symptoms. Probiotic supplementation may be recommended during antibiotic therapy to mitigate disruption of the gut microbiome.
7. Growth and Nutrition of Microbes
7.1 Nutritional Types of Microorganisms
Microorganisms can be classified based on their carbon and energy sources:
| Classification | Carbon Source | Energy Source | Examples |
|---|---|---|---|
| Photoautotrophs | CO₂ (inorganic) | Light | Cyanobacteria, algae, plants |
| Photoheterotrophs | Organic compounds | Light | Purple non-sulfur bacteria, green non-sulfur bacteria |
| Chemoautotrophs | CO₂ (inorganic) | Inorganic chemical reactions | Nitrifying bacteria, sulfur-oxidizing bacteria |
| Chemoheterotrophs | Organic compounds | Organic chemical reactions | Most bacteria, fungi, protozoa, animals |
Based on oxygen requirements, microorganisms can be classified as:
- Obligate aerobes: Require oxygen for growth (e.g., Mycobacterium tuberculosis, Pseudomonas aeruginosa)
- Microaerophiles: Require oxygen but at concentrations lower than atmospheric levels (e.g., Campylobacter jejuni, Helicobacter pylori)
- Facultative anaerobes: Can grow with or without oxygen (e.g., Escherichia coli, Staphylococcus aureus)
- Obligate anaerobes: Cannot tolerate oxygen and are killed by it (e.g., Clostridium species, Bacteroides fragilis)
- Aerotolerant anaerobes: Do not use oxygen but can tolerate its presence (e.g., Lactobacillus)
Mnemonic: “FAME O” – Oxygen Requirements
Facultative anaerobes (adaptable to oxygen presence)
Aerobes (oxygen-loving)
Microaerophiles (prefer low oxygen levels)
Endure oxygen (aerotolerant anaerobes)
Obligate anaerobes (oxygen is toxic)
7.2 Microbial Growth Phases
In a closed system (batch culture), bacterial growth follows a predictable pattern with four distinct phases:
Bacterial Growth Curve
Number of
Bacteria (log)
^
| Stationary Phase
| ______________________
| /
| /
| / Exponential/Log Phase
| /
| /
| /
| /
| /
| Lag Phase / Death Phase
| __________/ \
| / \
| / \
|/ \
+------------------------------------------>
Time
- Lag Phase: Cells adapt to the new environment, synthesize enzymes, and prepare for reproduction. Little or no cell division occurs.
- Exponential/Log Phase: Cells divide at a constant rate, with population doubling at regular intervals. This is the period of most rapid growth.
- Stationary Phase: Growth rate equals death rate, resulting in a stable population. This occurs when nutrients become limiting or waste products accumulate to inhibitory levels.
- Death/Decline Phase: Death rate exceeds growth rate, leading to a decrease in viable cells.
The generation time (doubling time) varies among bacterial species:
- E. coli: ~20 minutes under optimal conditions
- Staphylococcus aureus: ~30 minutes
- Mycobacterium tuberculosis: ~24 hours
7.3 Measuring Microbial Growth
Several methods are used to measure microbial growth in laboratory and clinical settings:
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Direct Count | Counting cells under a microscope using counting chambers (e.g., hemocytometer) | Simple, direct visualization | Cannot distinguish living from dead cells, labor-intensive |
| Viable Count (Plate Count) | Diluting sample and culturing on agar plates to count colonies | Counts only viable cells, quantitative | Time-consuming (24-48 hours), assumes one colony forms from one cell |
| Turbidity Measurement | Measuring light scattering (optical density) using a spectrophotometer | Rapid, non-destructive, can monitor growth over time | Cannot distinguish living from dead cells, less sensitive at low cell densities |
| Dry Weight | Measuring mass of cells after removing water | Simple, good for filamentous organisms | Not sensitive, destructive sampling |
| Metabolic Activity | Measuring oxygen consumption, CO₂ production, or ATP levels | Measures active cells, can be automated | Specialized equipment needed, indirect measurement |
Nursing Application
Understanding bacterial growth phases helps nurses appreciate why completing the full course of antibiotics is crucial. During stationary phase, bacteria are less metabolically active and may be less susceptible to antibiotics that target actively growing cells. Incomplete treatment can allow surviving bacteria to resume growth once the antibiotic pressure is removed.
8. Environmental Factors Affecting Microbial Growth
8.1 Temperature Effects
Temperature profoundly affects microbial growth rates and survival. Microorganisms can be classified based on their temperature preferences:
| Classification | Optimal Growth Temperature | Examples | Habitat |
|---|---|---|---|
| Psychrophiles | 0-15°C (32-59°F) | Psychrobacter, Polaromonas | Arctic/Antarctic waters, deep oceans |
| Psychrotrophs | 20-30°C (68-86°F) | Listeria monocytogenes, Pseudomonas fluorescens | Refrigerated foods, soil, water |
| Mesophiles | 30-45°C (86-113°F) | E. coli, Staphylococcus aureus, most human pathogens | Animal bodies, temperate environments |
| Thermophiles | 45-80°C (113-176°F) | Bacillus stearothermophilus, Thermus aquaticus | Hot springs, compost heaps |
| Hyperthermophiles | 80-121°C (176-250°F) | Pyrococcus, Thermococcus | Deep-sea hydrothermal vents, geothermal areas |
Mnemonic: “Please Make The Heat Happen” – Temperature Categories
Psychrophiles – Cold-loving (below 15°C)
Mesophiles – Moderate temperature (30-45°C)
Thermophiles – Heat-loving (45-80°C)
Hyperthermophiles – Extreme heat (above 80°C)
Temperature affects:
- Enzyme activity and protein stability
- Membrane fluidity and permeability
- Nucleic acid stability (DNA and RNA)
- Metabolic rates and overall growth kinetics
Key Concept
The principle of thermal sterilization and pasteurization is based on the susceptibility of microorganisms to high temperatures. Autoclaving (121°C, 15 psi, for 15-20 minutes) destroys all forms of microbial life, including highly resistant bacterial endospores.
8.2 Moisture Requirements
Water availability is critical for microbial growth. Water activity (aw) is a measure of the available water in a substance, with pure water having an aw of 1.0.
Based on water requirements, microorganisms can be classified as:
- Hydrophiles: Require high water activity (aw > 0.95) for growth (most bacteria, including all human pathogens)
- Xerotolerant: Can grow at reduced water activity (aw = 0.80-0.90) (some yeasts and molds)
- Xerophiles: Prefer or require low water activity (aw < 0.80) (some fungi and halophilic archaea)
Methods for controlling microbial growth by reducing water activity include:
- Drying/Dehydration: Removing water (e.g., dried foods, lyophilization)
- Adding Solutes: Increasing osmotic pressure (e.g., salting, sugaring)
- Freeze-drying: Combining freezing with dehydration under vacuum
| Food/Material | Approximate Water Activity (aw) | Microorganisms that Can Grow |
|---|---|---|
| Fresh meat, fruits, vegetables | 0.97-0.99 | Most bacteria, yeasts, and molds |
| Bread, cheese | 0.95-0.96 | Most bacteria, yeasts, and molds |
| Jam, syrup | 0.80-0.85 | Most yeasts and molds, no pathogenic bacteria |
| Dried fruits | 0.60-0.70 | Some xerotolerant molds, no bacteria |
| Honey, chocolate | 0.40-0.60 | Few extreme xerophiles |
| Crackers, dried pasta | 0.10-0.30 | No microbial growth |
Nursing Application
Keeping wound dressings dry is crucial in wound care, as moisture promotes microbial growth. For highly exudating wounds, appropriate moisture-wicking dressings should be selected and changed according to the manufacturer’s recommendations. Nurses should document the amount and characteristics of wound drainage and adapt dressing selection accordingly.
8.3 Blood and Body Fluids as Microbial Environments
Blood and body fluids provide rich nutrients for microbial growth but also contain antimicrobial factors that help prevent infections:
Blood as a Microbial Environment:
- Normally sterile in healthy individuals (bacteremia is abnormal)
- Rich in nutrients (glucose, proteins, minerals)
- Contains antimicrobial components:
- Complement system
- Antibodies
- Phagocytic cells (neutrophils, monocytes)
- Antimicrobial peptides (e.g., defensins)
- Transferrin (binds and sequesters iron)
- Supports growth of many pathogens if they can overcome host defenses
Other Body Fluids:
| Body Fluid | Normal Microbiota | Antimicrobial Factors | Common Pathogens |
|---|---|---|---|
| Urine | Normally sterile (before reaching urethra) | Low pH, flushing action, antimicrobial peptides | E. coli, Klebsiella, Proteus, Enterococcus |
| Cerebrospinal Fluid | Normally sterile | Blood-brain barrier, limited nutrients | Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae |
| Saliva | Diverse microbiota (>700 species) | Lysozyme, lactoferrin, IgA antibodies | Streptococcus mutans (dental caries), Porphyromonas (periodontitis) |
| Vaginal Fluid | Lactobacillus species dominant | Acidic pH (3.8-4.5), antimicrobial peptides | Candida albicans, Trichomonas vaginalis, Gardnerella vaginalis |
| Synovial Fluid | Normally sterile | Limited nutrients, antimicrobial peptides | Staphylococcus aureus, Neisseria gonorrhoeae, Streptococci |
Nursing Application
When collecting blood cultures, proper skin antisepsis is essential to prevent contamination with skin flora. The venipuncture site should be disinfected with chlorhexidine gluconate in alcohol (preferred) or alcohol followed by iodine, working in a concentric circle from the center outward. Multiple blood culture sets from different venipuncture sites increase the likelihood of detecting bacteremia while helping to distinguish true bacteremia from contamination.
9. Nursing Implications and Clinical Applications
Understanding microbial structure, classification, and growth factors is fundamental to nursing practice in infection prevention, control, and management. Key nursing implications include:
Infection Prevention and Control
- Hand Hygiene: Based on understanding of transient vs. resident flora and microbial survival on surfaces
- Aseptic Technique: Preventing introduction of microorganisms during invasive procedures
- Personal Protective Equipment (PPE): Selecting appropriate barriers based on transmission routes
- Environmental Cleaning: Targeting specific microbial threats with appropriate disinfectants
- Sterilization and Disinfection: Choosing methods based on microbial resistance hierarchy (spores most resistant, lipid-enveloped viruses least resistant)
Assessment and Monitoring
- Recognizing Signs of Infection: Understanding how microbial growth triggers inflammatory responses
- Specimen Collection: Proper techniques to ensure accurate microbiology results
- Interpreting Culture Results: Distinguishing pathogens from normal flora
- Monitoring Treatment Response: Recognizing expected clinical improvement patterns based on microbial killing kinetics
Treatment Considerations
- Antibiotic Administration: Timing, dosing, and monitoring based on pharmacokinetics and microbial growth characteristics
- Antimicrobial Stewardship: Promoting appropriate use of antimicrobials to prevent resistance
- Wound Care: Selecting appropriate dressings and techniques based on microbial considerations
- Management of Indwelling Devices: Preventing and managing biofilm-associated infections
Patient Education
- Medication Adherence: Explaining the importance of completing antimicrobial courses
- Infection Prevention: Teaching patients about hand hygiene, food safety, and preventing spread of infections
- Symptom Recognition: Educating patients about signs of infection that require medical attention
- Microbiome Health: Guidance on probiotics, diet, and avoiding unnecessary antibiotics
Nurses play a crucial role in breaking the chain of infection by understanding and addressing the six links:
Chain of Infection and Nursing Interventions
┌──────────────┐
Break here → ──┤ Infectious │── ← Break here
│ Agent │
┌─────────────────────>│ (Pathogen) │<─────────────────┐
│ └──────────────┘ │
│ ↑ │
│ │ │
┌────┴─────┐ │ ┌────┴─────┐
Break here → ──┤ Portal │ │ │ Reservoir │── ← Break here
│ of Entry │ │ │ │
└────┬─────┘ │ └────┬─────┘
│ │ │
│ │ │
│ ┌────────┴─────────┐ │
│ │ Mode of │ │
│ │ Transmission │ │
└───────────────────────┤ ├──────────────┘
Break here → └──────────────────┘ ← Break here
│ Susceptible
│ Host
└─────────── ← Break here
By applying knowledge of microbial structure, growth, and environmental requirements, nurses can develop evidence-based interventions that effectively break the chain of infection at multiple points, improving patient outcomes and reducing healthcare-associated infections.