Microorganisms: A Comprehensive Guide for Nursing Students
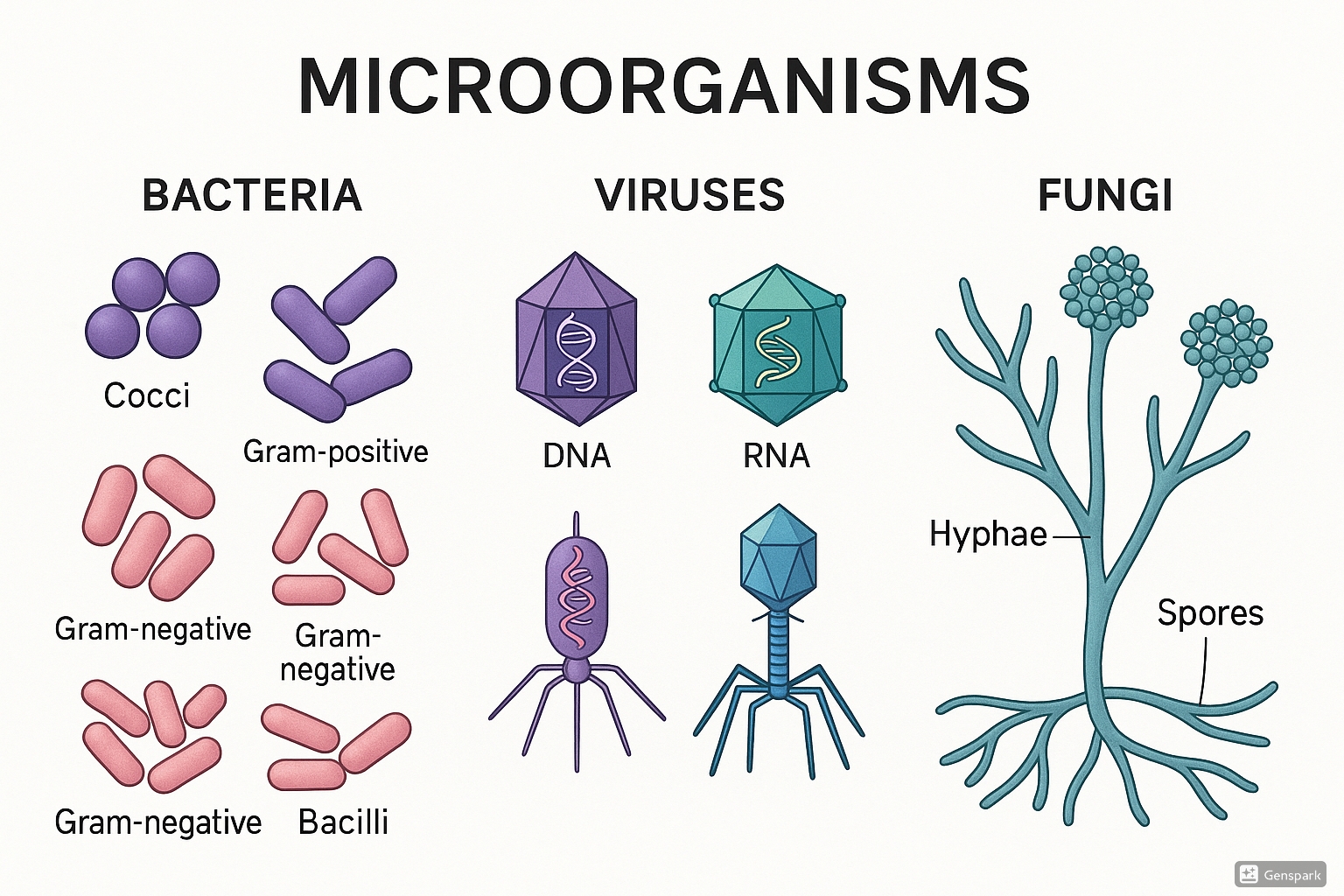
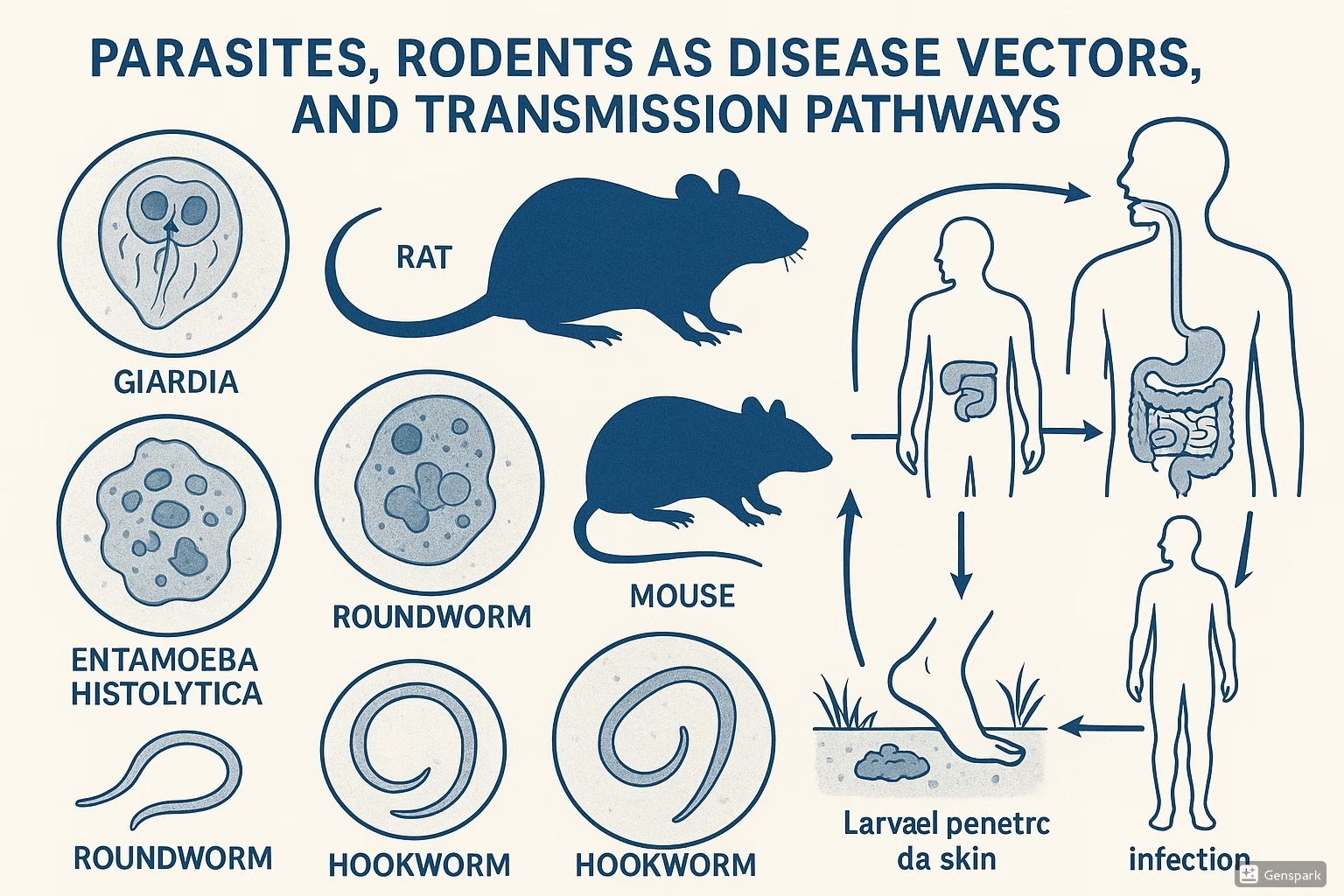
Illustration of different microorganisms including bacteria (cocci and bacilli), viruses, and fungi
1. Introduction to Microorganisms
Microorganisms are microscopic living entities that exist in all environments. As healthcare professionals, nurses need a comprehensive understanding of these organisms, their characteristics, and their impact on human health. This knowledge forms the foundation for infection control practices, antimicrobial stewardship, and patient education.
Microorganisms can be broadly classified into:
- Bacteria: Prokaryotic, single-celled organisms that can be classified by their cell wall structure (Gram-positive or Gram-negative) and morphology (cocci, bacilli, spirochetes).
- Viruses: Non-cellular infectious agents containing genetic material (DNA or RNA) surrounded by a protein coat.
- Fungi: Eukaryotic organisms that include yeasts and molds, causing both superficial and deep infections.
- Parasites: Organisms that live on or within a host and derive nutrients at the host’s expense.
- Prions: Infectious proteins that cause neurodegenerative diseases.
This guide focuses specifically on bacteria (gram-positive and gram-negative cocci and bacilli), viruses, and fungi, with special emphasis on their clinical significance for nursing practice.
2. Bacteria
Bacteria are prokaryotic microorganisms that lack a true nucleus and membrane-bound organelles. They are classified based on their:
- Morphology: Cocci (spherical), bacilli (rod-shaped), spirochetes (spiral)
- Gram stain reaction: Gram-positive (purple) or Gram-negative (pink)
- Oxygen requirements: Aerobic, anaerobic, facultative anaerobic, microaerophilic
- Motility: Presence or absence of flagella
Shape (cocci, bacilli, spirochetes)
Tinge (Gram-positive or Gram-negative)
Environment (oxygen requirements)
Propulsion (motility)
Uniqueness (special characteristics)
Pathogenicity (disease-causing potential)
2.1 Gram-Positive Cocci
Gram-positive cocci retain crystal violet dye during the Gram staining process due to their thick peptidoglycan cell wall layer. They appear purple under microscopic examination.
2.1.1 Staphylococcus
These cocci arrange in grape-like clusters and are a major cause of hospital and community-acquired infections.
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Staphylococcus aureus | Coagulase-positive, may be MRSA (Methicillin-resistant) | Skin and soft tissue infections, pneumonia, bacteremia, endocarditis, toxic shock syndrome | Contact precautions for MRSA, monitor for antimicrobial resistance |
| Staphylococcus epidermidis | Coagulase-negative, biofilm producer | Catheter-associated infections, prosthetic device infections | Aseptic technique for invasive procedures, catheter care |
| Staphylococcus saprophyticus | Coagulase-negative, urease-positive | Urinary tract infections, especially in young women | Proper hydration, collection of clean urine samples |
Skin infections (most common site)
Toxin producer (enterotoxins, TSST-1)
Abscesses (characteristic lesion)
Pus formation (pyogenic)
Hardiness (survives on dry surfaces)
2.1.2 Streptococcus
These cocci arrange in chains and are classified by their hemolytic patterns on blood agar (alpha, beta, gamma) and Lancefield grouping (A-V).
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Streptococcus pyogenes (Group A) | Beta-hemolytic, bacitracin-sensitive | Pharyngitis (strep throat), scarlet fever, impetigo, cellulitis, necrotizing fasciitis | Monitor for post-streptococcal sequelae (rheumatic fever, glomerulonephritis) |
| Streptococcus agalactiae (Group B) | Beta-hemolytic, CAMP test positive | Neonatal sepsis, meningitis, maternal infections | Screen pregnant women at 35-37 weeks, prophylactic antibiotics during labor if positive |
| Streptococcus pneumoniae | Alpha-hemolytic, lancet-shaped diplococci, optochin-sensitive | Pneumonia, otitis media, sinusitis, meningitis | Vaccination status, respiratory isolation, oxygen monitoring |
| Enterococcus (formerly Group D Strep) | Gamma-hemolytic, bile esculin positive | Urinary tract infections, endocarditis, bacteremia | Vancomycin-resistant enterococci (VRE) precautions, antimicrobial stewardship |
- Infection Control: Implement contact precautions for MRSA and VRE. Proper hand hygiene is crucial as these organisms can survive on surfaces.
- Medication Administration: Monitor for appropriate antibiotic therapy. For streptococcal infections, ensure full course completion to prevent rheumatic fever.
- Assessment: Be vigilant for signs of toxic shock syndrome with S. aureus (fever, rash, hypotension, multi-organ involvement).
- Patient Education: Teach patients with recurrent staphylococcal infections about decolonization protocols and personal hygiene.
- Surveillance: Monitor surgical sites for signs of infection, particularly in high-risk patients.
2.2 Gram-Negative Cocci
Gram-negative cocci have a thin peptidoglycan layer and an outer membrane containing lipopolysaccharides (endotoxin). They appear pink after Gram staining.
2.2.1 Neisseria
The most clinically relevant genus of gram-negative cocci, with kidney-bean shaped diplococci arrangement.
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Neisseria gonorrhoeae | Intracellular diplococci, oxidase-positive | Gonorrhea, pelvic inflammatory disease, neonatal conjunctivitis | Sexual contact tracing, prophylactic eye ointment for neonates |
| Neisseria meningitidis | Encapsulated, oxidase-positive | Meningitis, meningococcemia, Waterhouse-Friderichsen syndrome | Droplet precautions, rapid administration of antibiotics, monitor for petechial rash |
Needs special media (chocolate agar)
Easily killed by drying
Intracellular pathogens
Sexually transmitted (N. gonorrhoeae)
Serotypes determine virulence
Endotoxin producers
Rapid treatment necessary
Immune evasion mechanisms
Antimicrobial resistance increasing
- Isolation Precautions: Implement droplet precautions for patients with suspected meningococcal disease until 24 hours after effective antibiotic therapy.
- Rapid Intervention: Recognize that meningococcal disease can progress rapidly. Administer antibiotics promptly when ordered.
- Surveillance: Monitor for purpuric rash, which may indicate disseminated intravascular coagulation in meningococcemia.
- Prophylaxis Management: Identify close contacts of patients with meningococcal disease who may need prophylactic antibiotics.
- Sexual Health Education: Provide education on prevention of sexually transmitted infections for patients with gonococcal disease.
2.3 Gram-Positive Bacilli
Gram-positive bacilli are rod-shaped bacteria with thick peptidoglycan cell walls that retain crystal violet dye during Gram staining.
2.3.1 Bacillus
Large aerobic bacilli capable of forming endospores that are highly resistant to environmental stressors.
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Bacillus anthracis | Encapsulated, produces exotoxins (lethal and edema toxins) | Anthrax (cutaneous, gastrointestinal, inhalational, injection) | Bioterrorism agent awareness, post-exposure prophylaxis |
| Bacillus cereus | Produces heat-stable and heat-labile enterotoxins | Food poisoning (emetic and diarrheal types), ocular infections | Food safety education, proper refrigeration of rice and starchy foods |
2.3.2 Clostridium
Anaerobic, spore-forming bacilli responsible for several serious diseases through potent exotoxin production.
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Clostridium difficile | Produces enterotoxin A and cytotoxin B | Antibiotic-associated diarrhea, pseudomembranous colitis | Contact precautions, hand washing with soap and water (not alcohol-based sanitizer) |
| Clostridium tetani | Produces tetanospasmin neurotoxin | Tetanus (lockjaw) | Vaccination status, wound care, management of muscle spasms |
| Clostridium botulinum | Produces botulinum neurotoxin | Foodborne botulism, wound botulism, infant botulism | Respiratory support, antitoxin administration, food safety education |
| Clostridium perfringens | Produces alpha toxin and enterotoxin | Gas gangrene, food poisoning | Wound debridement, hyperbaric oxygen therapy, dietary management |
Cannot grow in oxygen (obligate anaerobes)
Love deep wounds (for C. tetani and C. perfringens)
Obligate spore-formers
Soil is common habitat
Toxin producers (primary virulence factor)
Resistant spores (heat, drying, disinfectants)
Invasive capability varies by species
Diagnosis often requires anaerobic culture
Intestinal colonization (C. difficile)
Antibiotics predispose to C. difficile infection
2.3.3 Corynebacterium
Pleomorphic gram-positive bacilli with characteristic metachromatic granules and “Chinese letter” arrangement.
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Corynebacterium diphtheriae | Produces diphtheria toxin (encoded by lysogenic phage) | Diphtheria (respiratory, cutaneous) | Droplet precautions, antitoxin administration, vaccination status |
2.3.4 Listeria
Small, facultatively anaerobic bacilli capable of intracellular survival and growth at refrigeration temperatures.
| Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Listeria monocytogenes | Tumbling motility, grows at 4°C, intracellular pathogen | Meningitis, septicemia, feto-maternal infection | Food safety for pregnant women and immunocompromised patients |
- C. difficile Management:
- Implement contact precautions with dedicated equipment
- Emphasize hand washing with soap and water, not alcohol-based hand sanitizers
- Monitor fluid balance and electrolytes during active infection
- Document stool frequency, consistency, and characteristics
- Tetanus Prevention:
- Assess vaccination status for all patients with wounds
- Provide proper wound cleaning and debridement
- Administer tetanus prophylaxis as ordered based on wound characteristics and immunization history
- Botulism Care:
- Monitor respiratory function closely
- Perform frequent neurological assessments
- Position patient to prevent aspiration
- Provide education on proper food canning and preparation
- Nutrition Counseling: Educate pregnant women and immunocompromised patients about avoiding Listeria risks (soft cheeses, deli meats, unpasteurized dairy)
2.4 Gram-Negative Bacilli
Gram-negative bacilli have a thin peptidoglycan layer with an outer membrane containing lipopolysaccharide (endotoxin). They appear pink in Gram stain and include many significant pathogens.
2.4.1 Enterobacteriaceae
A large family of facultatively anaerobic gram-negative bacilli that normally inhabit the intestinal tract.
| Genus/Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Escherichia coli | Lactose fermenter, many pathotypes (EPEC, ETEC, EHEC, EIEC, UPEC) | Urinary tract infections, sepsis, meningitis (neonates), gastroenteritis | Hand hygiene, urinary catheter care, prevent cross-contamination |
| Klebsiella pneumoniae | Encapsulated, mucoid colonies, lactose fermenter | Pneumonia, UTI, liver abscess, hospital-acquired infections | Monitor for antimicrobial resistance (KPC, ESBL), respiratory assessment |
| Salmonella species | Non-lactose fermenter, H2S producer | Gastroenteritis, typhoid fever, bacteremia | Contact precautions, food safety education, monitor for dehydration |
| Shigella species | Non-lactose fermenter, non-motile | Bacillary dysentery (shigellosis) | Low infectious dose, strict hand hygiene, fluid management |
| Proteus species | Swarming motility, urease positive | Urinary tract infections, particularly with stones | Urine pH monitoring, catheter care, prevention of stone formation |
Enterococcus faecium (gram-positive but part of the mnemonic)
Staphylococcus aureus (gram-positive but part of the mnemonic)
Klebsiella pneumoniae
Acinetobacter baumannii
Pseudomonas aeruginosa
Enterobacter species
2.4.2 Non-Fermenters
Aerobic gram-negative bacilli that cannot ferment glucose, often associated with healthcare-associated infections.
| Genus/Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Pseudomonas aeruginosa | Oxidase-positive, produces pyocyanin (blue-green pigment), sweet grape odor | Pneumonia, burn infections, UTI, otitis externa, eye infections | Antimicrobial resistance, biofilm formation, equipment disinfection |
| Acinetobacter baumannii | Oxidase-negative, coccobacilli appearance | Pneumonia, bacteremia, wound infections, meningitis | Multiple drug resistance, environmental cleaning, isolation |
| Stenotrophomonas maltophilia | Oxidase-negative, intrinsically resistant to carbapenems | Pneumonia, bacteremia in immunocompromised patients | Limited treatment options, respiratory assessment |
2.4.3 Other Significant Gram-Negative Bacilli
| Genus/Species | Key Characteristics | Common Infections | Nursing Considerations |
|---|---|---|---|
| Haemophilus influenzae | Pleomorphic, requires X (hemin) and V (NAD) factors | Meningitis, epiglottitis, pneumonia, otitis media | Vaccination status (Hib), droplet precautions |
| Bordetella pertussis | Coccobacilli, fastidious growth, produces pertussis toxin | Pertussis (whooping cough) | Droplet precautions, paroxysmal cough management, vaccination |
| Legionella pneumophila | Intracellular pathogen, requires L-cysteine and iron | Legionnaires’ disease, Pontiac fever | Water system management, respiratory assessment |
| Helicobacter pylori | Spiral-shaped, produces urease, microaerophilic | Gastritis, peptic ulcer disease, gastric cancer | Triple/quadruple therapy management, patient education |
- Infection Control:
- Implement contact precautions for multidrug-resistant organisms (CRE, ESBL, etc.)
- Ensure proper environmental cleaning, especially for non-fermenters that can survive in moist environments
- Practice strict hand hygiene to prevent cross-contamination
- Device-Associated Infection Prevention:
- Follow bundle approaches for preventing central line-associated bloodstream infections
- Implement catheter-associated urinary tract infection prevention bundles
- Perform oral care for ventilated patients to prevent ventilator-associated pneumonia
- Antimicrobial Stewardship:
- Monitor for appropriate antibiotic selection, dosing, and duration
- Be aware of local resistance patterns
- Ensure cultures are obtained before initiating antibiotics when possible
- Patient Education:
- Teach foodborne illness prevention for Salmonella and Shigella
- Educate patients on proper handwashing techniques
- Provide guidance on medication adherence for eradication therapies (H. pylori)
Bacterial Classification Flowchart
Gram Stain → Positive (Purple) or Negative (Pink)
├─ Gram-Positive
│ ├─ Cocci
│ │ ├─ Clusters → Staphylococcus
│ │ └─ Chains → Streptococcus
│ └─ Bacilli
│ ├─ Spore-forming
│ │ ├─ Aerobic → Bacillus
│ │ └─ Anaerobic → Clostridium
│ └─ Non-spore-forming
│ ├─ Pleomorphic → Corynebacterium
│ └─ Regular → Listeria
└─ Gram-Negative
├─ Cocci
│ └─ Diplococci → Neisseria
└─ Bacilli
├─ Fermenters → Enterobacteriaceae
│ (E. coli, Klebsiella, Salmonella, etc.)
└─ Non-fermenters
(Pseudomonas, Acinetobacter, etc.)
3. Viruses
Viruses are obligate intracellular parasites consisting of genetic material (DNA or RNA) enclosed in a protein coat called a capsid, sometimes surrounded by a lipid envelope. They require host cell machinery for replication and cannot reproduce independently.
3.1 Structure and Classification
Viruses are classified based on:
- Type of nucleic acid: DNA or RNA (single or double-stranded)
- Presence of envelope: Enveloped or non-enveloped
- Capsid symmetry: Icosahedral, helical, complex
- Size and shape
- Mode of replication
DNA Viruses
- Adenovirus
- Herpesvirus
- Poxvirus
- Hepadnavirus (HBV)
- Papillomavirus
Features: Generally replicate in the nucleus (except poxviruses), use host DNA polymerase, can establish latency
RNA Viruses
- Orthomyxovirus (Influenza)
- Coronavirus
- Picornavirus
- Retrovirus (HIV)
- Flavivirus
Features: Replicate in cytoplasm (except retroviruses), higher mutation rates, often cause acute infections
Enveloped Viruses
- Influenza virus
- Coronavirus
- Herpesviruses
- HIV
- Hepatitis C virus
Features: More susceptible to disinfectants, detergents, and drying; spread through respiratory droplets, blood, or sexual contact
Non-enveloped Viruses
- Adenovirus
- Norovirus
- Rotavirus
- Poliovirus
- Papillomavirus
Features: Highly resistant to environmental conditions and many disinfectants; often spread through fecal-oral route
Papillomavirus (HPV)
Adenovirus
Varicella-zoster virus (and all herpesviruses)
Epstein-Barr virus (also a herpesvirus)
Plus: Hepatitis B virus (HBV), Poxvirus
3.2 Viral Replication
Viral replication follows a general pattern with variations depending on the specific virus:
- Attachment: Virus binds to specific receptors on host cell
- Penetration: Virus enters cell by endocytosis, fusion, or direct penetration
- Uncoating: Viral genome is released into the cell
- Replication: Viral genome is replicated and viral proteins are synthesized
- Assembly: Viral components are assembled into new virions
- Release: Virions exit the cell by budding (enveloped viruses) or cell lysis (non-enveloped viruses)
Viral Replication Cycle
Attachment → Penetration → Uncoating
↓
Viral Genome Release
↓
DNA Virus → Host nucleus → DNA replication → mRNA → Protein synthesis
OR
RNA Virus → Cytoplasm → RNA replication/Protein synthesis
↓
Assembly of Viral Components
↓
Release
├─ Enveloped virus → Budding through cell membrane
└─ Non-enveloped virus → Cell lysis
3.3 Common Viruses in Clinical Settings
3.3.1 Respiratory Viruses
| Virus | Key Characteristics | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|
| Influenza virus | RNA virus, segmented genome, antigenic shift and drift | Influenza, viral pneumonia | Vaccination, droplet precautions, antiviral timing |
| SARS-CoV-2 | RNA virus, spike protein binds to ACE2 receptors | COVID-19, from asymptomatic to severe pneumonia | Droplet and contact precautions, oxygen monitoring, vaccination |
| Respiratory syncytial virus (RSV) | RNA virus, forms syncytia | Bronchiolitis in infants, pneumonia in elderly | High-risk infant protection, supportive care, oxygen therapy |
3.3.2 Herpesviruses
| Virus | Key Characteristics | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|
| Herpes simplex virus 1 (HSV-1) | DNA virus, latency in trigeminal ganglia | Oral herpes (cold sores), keratitis, encephalitis | Trigger avoidance, antiviral therapy, eye protection |
| Herpes simplex virus 2 (HSV-2) | DNA virus, latency in sacral ganglia | Genital herpes | Sexual health education, suppressive therapy options, neonatal exposure precautions |
| Varicella-zoster virus (VZV) | DNA virus, latency in dorsal root ganglia | Chickenpox (varicella), shingles (herpes zoster) | Airborne precautions for varicella, pain management for zoster, vaccination |
| Cytomegalovirus (CMV) | DNA virus, largest herpesvirus | Usually asymptomatic, severe in immunocompromised, congenital infections | Handwashing, pregnancy precautions, transplant monitoring |
| Epstein-Barr virus (EBV) | DNA virus, infects B lymphocytes | Infectious mononucleosis, associated with certain lymphomas | Rest, hydration, spleen rupture precautions |
3.3.3 Hepatitis Viruses
| Virus | Key Characteristics | Transmission | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|---|
| Hepatitis A (HAV) | RNA virus, non-enveloped | Fecal-oral | Acute hepatitis, no chronic state | Hand hygiene, vaccination, contact precautions |
| Hepatitis B (HBV) | DNA virus, enveloped | Blood, sexual, vertical | Acute or chronic hepatitis, hepatocellular carcinoma | Vaccination, standard precautions, perinatal prophylaxis |
| Hepatitis C (HCV) | RNA virus, enveloped | Primarily blood | Acute or chronic hepatitis, cirrhosis, hepatocellular carcinoma | Screening, direct-acting antiviral therapy, liver monitoring |
Always transmitted through fecal-oral route (HAV)
Blood, birth, body fluids transmit HBV
Commonly spread through blood and needles (HCV)
Deficient virus that requires HBV to replicate (HDV)
Enteric transmission, especially in water (HEV)
3.3.4 HIV and Retroviruses
HIV (Human Immunodeficiency Virus) is an RNA retrovirus that targets CD4+ T cells, leading to progressive immune system deterioration.
Key Characteristics:
- Uses reverse transcriptase to convert RNA to DNA
- Integrates viral DNA into host genome (provirus)
- Long clinical latency period
- High genetic variability
Transmission: Blood, sexual contact, vertical transmission (mother to child)
Clinical Manifestations:
- Acute HIV infection: Flu-like syndrome
- Clinical latency: Asymptomatic period
- AIDS: CD4+ count <200 cells/mm³, opportunistic infections, malignancies
- Infection Control:
- Implement appropriate isolation precautions based on virus transmission mode
- Practice proper hand hygiene and use of personal protective equipment
- Educate patients and families about preventing virus spread
- Vaccination Promotion:
- Assess vaccination status for preventable viral diseases
- Educate about vaccine benefits and address hesitancy
- Implement catch-up vaccination schedules when needed
- Symptom Management:
- Provide supportive care for fever, dehydration, pain
- Monitor for complications like respiratory distress
- Administer antivirals as ordered and monitor for efficacy and side effects
- HIV Management:
- Promote adherence to antiretroviral therapy
- Monitor for drug interactions and side effects
- Assess for opportunistic infections
- Provide psychosocial support and education
- Pregnancy Considerations:
- Implement measures to prevent congenital infections (CMV, rubella, HIV, etc.)
- Educate pregnant women about risk reduction
4. Fungi
Fungi are eukaryotic organisms that include yeasts, molds, and mushrooms. In clinical settings, fungi are classified based on their morphology (yeasts or molds) and the types of infections they cause (superficial, cutaneous, subcutaneous, systemic, or opportunistic).
Key Characteristics of Fungi:
- Eukaryotic cells with rigid cell walls containing chitin
- May exist as unicellular yeasts or multicellular filamentous molds
- Some are dimorphic (exist in both yeast and mold forms depending on conditions)
- Reproduce sexually or asexually
4.1 Superficial Mycoses
Superficial mycoses affect the outermost layers of the skin, hair, or nails without significant tissue invasion or immune response.
| Infection | Causative Organism | Clinical Presentation | Nursing Considerations |
|---|---|---|---|
| Tinea versicolor (Pityriasis versicolor) |
Malassezia furfur (formerly Pityrosporum) |
Hypo- or hyperpigmented macules on trunk and upper arms; mild scaling | Topical antifungals, selenium sulfide shampoo, prevention of recurrence |
| Tinea nigra | Hortaea werneckii | Brown-black macules, often on palms | Topical antifungals, exfoliating agents |
| White piedra | Trichosporon species | White to light brown nodules on hair shafts | Hair removal, topical or oral antifungals |
| Black piedra | Piedraia hortae | Hard, dark nodules firmly attached to hair shafts | Hair removal, topical or oral antifungals |
4.1.1 Dermatophytoses (Ringworm infections)
Dermatophytes are fungi that invade keratinized tissues (skin, hair, nails) and cause characteristic “ringworm” infections, named according to the body site affected.
| Infection | Causative Organisms | Clinical Presentation | Nursing Considerations |
|---|---|---|---|
| Tinea corporis (body ringworm) |
Trichophyton, Microsporum, Epidermophyton species | Circular, erythematous, scaling patches with central clearing | Topical antifungals, hygiene education |
| Tinea capitis (scalp ringworm) |
Trichophyton tonsurans, Microsporum species | Scaling, hair loss, kerion formation | Oral antifungals, prevention of spread in schools |
| Tinea pedis (athlete’s foot) |
Trichophyton rubrum, T. mentagrophytes, Epidermophyton floccosum | Scaling, maceration between toes; vesicular or moccasin-type distribution | Foot hygiene, keeping feet dry, topical antifungals |
| Tinea cruris (jock itch) |
Trichophyton rubrum, T. mentagrophytes, Epidermophyton floccosum | Erythematous patches in groin area, sparing scrotum | Hygiene, moisture control, loose clothing |
| Tinea unguium (onychomycosis) |
Trichophyton rubrum, T. mentagrophytes | Nail discoloration, thickening, subungual debris | Oral antifungals, patient education on long treatment duration |
Dry the affected area thoroughly
Examine for characteristic ring-like lesions
Refer severe cases for oral treatment
Moisture control is essential for prevention
Avoid sharing personal items
Treat with topical antifungals for mild cases
Oral antifungals for extensive disease
Prevent recurrence through hygiene
Hair, skin, nails can all be affected
Yield best results with complete treatment courses
Trichophyton is a common causative genus
Educate patients about transmission
4.1.2 Candidiasis
Candidiasis refers to infections caused by Candida species, particularly Candida albicans. These yeasts are normal flora in the gastrointestinal tract, mouth, and vagina but can cause opportunistic infections when host defenses are altered.
| Infection | Clinical Presentation | Risk Factors | Nursing Considerations |
|---|---|---|---|
| Oral thrush | White, removable plaques on oral mucosa | Immunosuppression, antibiotic use, infancy, denture use | Oral hygiene, antifungal solutions, denture care |
| Vulvovaginal candidiasis | Vaginal itching, white discharge, erythema | Pregnancy, diabetes, antibiotics, hormonal contraceptives | Topical or oral antifungals, hygiene education |
| Cutaneous candidiasis | Red, macerated lesions in intertriginous areas | Obesity, diabetes, moisture | Keep areas dry, topical antifungals, address underlying conditions |
| Diaper dermatitis | Red, sharply demarcated rash in diaper area | Prolonged diaper use, moisture, antibiotic use | Frequent diaper changes, barrier creams, topical antifungals |
4.2 Deep Mycoses
Deep (systemic) mycoses involve fungal invasion of deep tissues and organs. They may be caused by primary pathogenic fungi or opportunistic fungi in immunocompromised hosts.
4.2.1 Endemic Mycoses
Caused by dimorphic fungi that exist in specific geographic regions and can cause disease in immunocompetent individuals.
| Infection | Causative Organism | Geographic Distribution | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|---|
| Histoplasmosis | Histoplasma capsulatum | Ohio and Mississippi River valleys | Often asymptomatic; can cause pneumonia, disseminated disease | Respiratory assessment, antifungal management |
| Coccidioidomycosis (Valley fever) |
Coccidioides immitis, C. posadasii |
Southwestern US, parts of Central and South America | Pneumonia, erythema nodosum, disseminated disease | Travel history assessment, respiratory monitoring |
| Blastomycosis | Blastomyces dermatitidis | North America, especially Great Lakes region | Pneumonia, skin lesions, bone lesions | Long-term antifungal therapy, patient education |
| Paracoccidioidomycosis | Paracoccidioides brasiliensis | Latin America | Mucocutaneous lesions, pulmonary disease | Nutritional support, oral care for mucosal lesions |
4.2.2 Opportunistic Mycoses
Caused by fungi that typically affect immunocompromised hosts and can cause severe, often life-threatening infections.
| Infection | Causative Organism | Risk Factors | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|---|
| Invasive candidiasis | Candida species (C. albicans, C. auris, etc.) |
Central venous catheters, broad-spectrum antibiotics, neutropenia, total parenteral nutrition | Candidemia, end-organ involvement, sepsis | Catheter care, surveillance cultures, antifungal prophylaxis in high-risk patients |
| Invasive aspergillosis | Aspergillus species (A. fumigatus, A. flavus, etc.) |
Prolonged neutropenia, hematopoietic stem cell transplant, solid organ transplant, corticosteroid use | Pulmonary disease, sinusitis, disseminated disease | HEPA filtration for high-risk patients, galactomannan monitoring, voriconazole administration |
| Cryptococcosis | Cryptococcus neoformans, C. gattii |
HIV/AIDS, organ transplantation, other immunosuppression | Meningitis, pneumonia, skin lesions | Intracranial pressure monitoring, antifungal therapy, lumbar puncture assistance |
| Mucormycosis (Zygomycosis) |
Rhizopus, Mucor, Rhizomucor species |
Diabetic ketoacidosis, neutropenia, deferoxamine therapy | Rhinocerebral, pulmonary, cutaneous, or disseminated disease | Surgical debridement coordination, glucose control, amphotericin B administration |
| Pneumocystis pneumonia | Pneumocystis jirovecii (formerly P. carinii) |
HIV/AIDS, solid organ transplant, hematologic malignancies, corticosteroids | Fever, dyspnea, nonproductive cough, hypoxemia | Oxygen therapy, TMP-SMX administration, corticosteroid adjunctive therapy for hypoxemia |
Fever unresponsive to antibiotics
Underlying immunocompromise (HIV, diabetes, steroids, etc.)
Nodules (pulmonary, skin) or necrotic lesions
Growth that is slow in culture
Antibiotics failing to improve condition
Long-term therapy often required
4.2.3 Subcutaneous Mycoses
Fungi that infect the subcutaneous tissues, usually following traumatic inoculation.
| Infection | Causative Organism | Clinical Manifestations | Nursing Considerations |
|---|---|---|---|
| Sporotrichosis | Sporothrix schenckii complex | Nodular lymphangitic spread along lymphatics from inoculation site | Wound care, itraconazole administration, patient education |
| Chromoblastomycosis | Fonsecaea, Phialophora, Cladophialophora species | Verrucous plaques, often on lower extremities | Prolonged antifungal therapy, surgical excision in some cases |
| Mycetoma | Various fungi (eumycetoma) or actinomycetes (actinomycetoma) | Triad of swelling, sinus tract formation, and grain discharge | Wound care, medication adherence counseling |
- Assessment:
- Conduct thorough skin and mucous membrane assessments in at-risk patients
- Identify risk factors (immunosuppression, diabetes, antibiotic use)
- Monitor for fungal superinfection during antibiotic therapy
- Prevention:
- Maintain skin integrity and dryness, especially in intertriginous areas
- Implement protective environment measures for severely immunocompromised patients
- Provide antifungal prophylaxis as prescribed for high-risk patients
- Medication Administration:
- Administer antifungal medications correctly (topical, oral, IV)
- Monitor for drug interactions with azole antifungals
- Assess for nephrotoxicity with amphotericin B therapy
- Monitor liver function with systemic azole or echinocandin therapy
- Patient Education:
- Teach proper application of topical antifungals
- Emphasize importance of completing full course of therapy
- Provide strategies to prevent recurrence (hygiene, moisture control)
- Educate on recognition of treatment failure or complications
- Special Considerations:
- Implement isolation precautions for multidrug-resistant Candida auris
- Provide oral care for patients with oral thrush
- Address psychosocial aspects of visible fungal infections
- Coordinate multidisciplinary care for invasive fungal infections
5. Nursing Implications
5.1 Infection Control Measures
Nurses play a critical role in preventing the transmission of microorganisms within healthcare settings and the community.
5.1.1 Standard Precautions
Apply to all patients regardless of suspected or confirmed infection status:
- Hand Hygiene: The single most important measure to prevent pathogen transmission
- Personal Protective Equipment (PPE): Gloves, gowns, masks, eye protection based on anticipated exposure
- Respiratory Hygiene/Cough Etiquette: Cover mouth/nose when coughing, dispose of tissues properly
- Safe Injection Practices: Use of sterile, single-use needles and syringes
- Environmental Cleaning: Regular disinfection of patient care areas and equipment
5.1.2 Transmission-Based Precautions
Additional measures used for patients with known or suspected infections:
| Type | For Which Pathogens | Key Measures | Examples |
|---|---|---|---|
| Contact Precautions | Pathogens transmitted by direct or indirect contact | Gloves and gown for all patient contact, dedicated equipment, private room | MRSA, VRE, C. difficile, multidrug-resistant gram-negatives |
| Droplet Precautions | Pathogens transmitted by large respiratory droplets (≥5μm) | Surgical mask within 3-6 feet of patient, private room | Influenza, N. meningitidis, Bordetella pertussis |
| Airborne Precautions | Pathogens transmitted by small particles (≤5μm) that remain suspended in air | Airborne infection isolation room (negative pressure), N95 respirator or PAPR | TB, measles, varicella, disseminated zoster |
5.2 Antimicrobial Therapy Management
5.2.1 Antibacterial Agents
| Class | Examples | Mechanism of Action | Nursing Considerations |
|---|---|---|---|
| Beta-lactams | Penicillins, cephalosporins, carbapenems, monobactams | Inhibit cell wall synthesis | Monitor for allergic reactions, assess for cross-reactivity |
| Aminoglycosides | Gentamicin, tobramycin, amikacin | Inhibit protein synthesis by binding to 30S ribosomal subunit | Monitor renal function, therapeutic drug monitoring, ototoxicity assessment |
| Fluoroquinolones | Ciprofloxacin, levofloxacin | Inhibit DNA gyrase and topoisomerase IV | Tendon rupture risk, CNS effects, QT prolongation |
| Macrolides | Erythromycin, azithromycin, clarithromycin | Inhibit protein synthesis by binding to 50S ribosomal subunit | GI disturbances, drug interactions, QT prolongation |
| Glycopeptides | Vancomycin, teicoplanin | Inhibit cell wall synthesis | Infusion-related reactions (“Red Man Syndrome”), therapeutic drug monitoring |
5.2.2 Antifungal Agents
| Class | Examples | Mechanism of Action | Nursing Considerations |
|---|---|---|---|
| Polyenes | Amphotericin B, nystatin | Bind to ergosterol in fungal cell membrane | Nephrotoxicity, infusion reactions, electrolyte monitoring |
| Azoles | Fluconazole, itraconazole, voriconazole, posaconazole | Inhibit ergosterol synthesis | Drug interactions, hepatotoxicity, visual disturbances (voriconazole) |
| Echinocandins | Caspofungin, micafungin, anidulafungin | Inhibit cell wall synthesis by blocking β-1,3-glucan synthase | Generally well-tolerated, monitor for histamine reactions |
5.2.3 Antiviral Agents
| Type | Examples | For Which Viruses | Nursing Considerations |
|---|---|---|---|
| Nucleoside/nucleotide analogs | Acyclovir, valacyclovir, ganciclovir, entecavir | Herpesviruses, HBV | Adequate hydration, renal function monitoring |
| Neuraminidase inhibitors | Oseltamivir, zanamivir | Influenza A and B | Early administration for best efficacy |
| Protease inhibitors | Various HIV and HCV medications | HIV, HCV | Numerous drug interactions, adherence importance |
Right patient
Interventions (verify indications)
Good timing (right time)
Harmless (no allergies, no contraindications)
True dose and calculation
Safe route and technique
- Appropriate Specimen Collection:
- Collect specimens before starting antibiotics when possible
- Follow proper collection techniques to prevent contamination
- Label and transport specimens correctly
- Medication Administration:
- Administer antimicrobials on schedule to maintain therapeutic levels
- Monitor for side effects and adverse reactions
- Assess for drug interactions
- Monitoring Response to Therapy:
- Track clinical markers of infection (temperature, WBC count, etc.)
- Observe for resolution of symptoms
- Report lack of improvement or deterioration
- Patient Education:
- Explain the importance of completing full course of therapy
- Teach about potential side effects and when to report them
- Provide information about infection prevention measures
- Advocacy:
- Question antimicrobial orders that don’t align with patient presentation
- Advocate for de-escalation of therapy when appropriate
- Suggest infectious disease consultation for complex cases