Appendicitis
Comprehensive Nursing Study Notes
Table of Contents
Introduction to Appendicitis
Quick Definition
Appendicitis is the acute inflammation of the vermiform appendix, a small tube-like structure attached to the cecum. It represents one of the most common surgical emergencies worldwide, affecting approximately 7% of the population during their lifetime.
Key Statistics
- Peak incidence: 10-30 years of age
- Male to female ratio: 1.4:1
- Lifetime risk: ~7-8%
- Mortality rate: <1% when uncomplicated
Time-Critical Nature
Appendicitis progression follows a predictable timeline that makes early recognition and intervention crucial for optimal patient outcomes.
Why Nurses Need to Master Appendicitis Care
First Line Assessment
Nurses are often the first healthcare providers to assess patients with abdominal pain, making early recognition skills essential.
Continuous Monitoring
Ongoing assessment for symptom progression and complications requires specialized nursing knowledge and vigilance.
Holistic Care
From pain management to post-operative care, nurses provide comprehensive support throughout the patient journey.
Anatomy & Pathophysiology
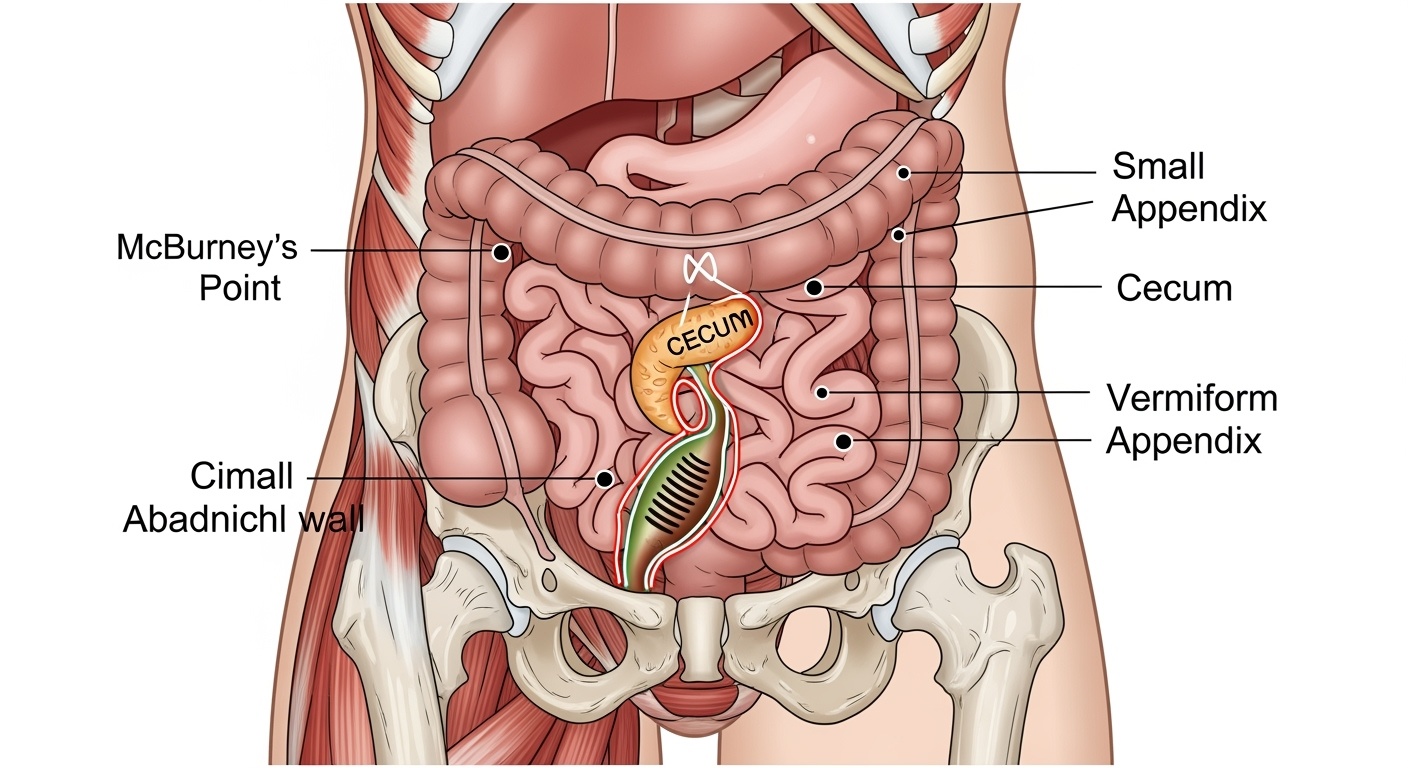
Anatomical location of the appendix and McBurney’s point in relation to abdominal structures
Appendix Anatomy
Key Anatomical Features
- Location: Attached to the cecum at the ileocecal junction
- Length: 5-10 cm (average 8 cm)
- Diameter: 6-8 mm
- Position: Variable – retrocecal (most common), pelvic, subcecal
- Blood Supply: Appendicular artery (branch of ileocolic artery)
- Nerve Supply: Sympathetic and parasympathetic fibers
Memory Aid: Appendix Positions
- Retrocecal (65%)
- Pelvic (30%)
- Subcecal (2%)
- Paracecal (3%)
Pathophysiology Timeline
Stage 1: Obstruction (0-12 hours)
Appendiceal lumen becomes blocked by fecalith, lymphoid hyperplasia, or foreign body. Mucus secretion continues, causing distension.
Stage 2: Inflammation (12-24 hours)
Increased intraluminal pressure leads to venous congestion, bacterial overgrowth, and inflammatory response. Pain localizes to RLQ.
Stage 3: Ischemia (24-48 hours)
Arterial compromise occurs due to swelling and pressure. Tissue necrosis begins, increasing perforation risk.
Stage 4: Perforation (>48 hours)
Necrotic tissue ruptures, releasing infected contents into peritoneal cavity. Generalized peritonitis may develop.
McBurney’s Point – The Landmark
Location & Significance
- Located at junction of lateral 1/3 and medial 2/3 of line from anterior superior iliac spine to umbilicus
- Point of maximum tenderness in typical appendicitis
- Approximately 4-5 cm from anterior superior iliac spine
Clinical Importance
McBurney’s point tenderness is present in approximately 50-60% of appendicitis cases, making it a valuable but not definitive diagnostic sign.
Clinical Presentation & Specific Signs
Classic Appendicitis Triad
Abdominal Pain
Periumbilical → RLQ migration
Fever
Low-grade initially (100-101°F)
Anorexia
Loss of appetite often earliest sign
Early Signs & Symptoms
0-6 Hours
- • Vague periumbilical or epigastric pain
- • Anorexia (loss of appetite)
- • Nausea without vomiting
- • General malaise
6-12 Hours
- • Pain migrates to right lower quadrant
- • Nausea with possible vomiting
- • Low-grade fever begins
- • McBurney’s point tenderness develops
12-24 Hours
- • Localized RLQ pain and tenderness
- • Guarding and rigidity
- • Fever elevation (101-102°F)
- • Positive special signs
Specific Physical Signs
McBurney’s Sign
Point tenderness at McBurney’s point (1/3 distance from ASIS to umbilicus)
Rovsing’s Sign
RLQ pain when LLQ is palpated
Psoas Sign
RLQ pain with right hip flexion against resistance
Obturator Sign
RLQ pain with internal rotation of flexed right hip
Atypical Presentations
Pediatric
- • Diffuse abdominal pain
- • Higher fever
- • Irritability, crying
- • Rapid progression
Elderly
- • Vague symptoms
- • Minimal fever
- • Delayed presentation
- • Higher complication rate
Pregnant
- • RUQ pain (3rd trimester)
- • Mild leukocytosis normal
- • Nausea/vomiting common
- • Higher perforation risk
Obese
- • Delayed diagnosis
- • Difficult examination
- • Imaging challenges
- • Increased complications
Memory Aid: Appendicitis Symptoms
- Anorexia (loss of appetite)
- Pain migration (periumbilical to RLQ)
- Point tenderness (McBurney’s)
- Elevated temperature
- Nausea and vomiting
- Distension (mild)
- Increased WBC count
- Cramping pain initially
- Intensifying symptoms
- Time-sensitive condition
- Infection signs
- Surgical emergency
Diagnostic Criteria & Assessment Tools
Laboratory Investigations
| Test | Normal Range | Appendicitis Findings |
|---|---|---|
| WBC Count | 4,500-11,000/μL | 12,000-18,000/μL |
| Neutrophils | 40-70% | 75-90% (left shift) |
| CRP | <3 mg/L | 10-100 mg/L |
| Urinalysis | Normal | Mild pyuria/hematuria |
Important Notes
- • Normal WBC doesn’t rule out appendicitis (10-15% of cases)
- • Elderly patients may have minimal elevation
- • CRP rises 6-12 hours after symptom onset
- • Urinalysis helps exclude urinary tract pathology
Imaging Studies
CT Scan (Gold Standard)
Advantages
- • 95-99% accuracy
- • Shows complications
- • Rules out other pathology
- • Guides surgical planning
CT Findings
- • Appendiceal wall thickening
- • Fat stranding
- • Fluid collection
- • Appendicolith
Ultrasound
Best For
- • Pediatric patients
- • Pregnant women
- • No radiation exposure
- • Point-of-care assessment
Limitations
- • Operator dependent
- • Difficult in obese patients
- • Gas interference
- • 70-90% accuracy
MRI
Reserved for specific situations:
- • Pregnant patients (2nd/3rd trimester)
- • Contraindication to CT contrast
- • Equivocal CT findings
- • High accuracy (97-99%)
Clinical Scoring Systems
Alvarado Score
| Criteria | Points |
|---|---|
| Migratory RLQ pain | 1 |
| Anorexia | 1 |
| Nausea/vomiting | 1 |
| RLQ tenderness | 2 |
| Rebound tenderness | 1 |
| Fever >37.3°C | 1 |
| Leukocytosis | 2 |
| Left shift | 1 |
- • 1-4: Low probability
- • 5-6: Intermediate probability
- • 7-10: High probability
Pediatric Appendicitis Score
| Criteria | Points |
|---|---|
| Fever >38°C | 1 |
| Anorexia | 1 |
| Nausea/vomiting | 1 |
| RLQ tenderness | 2 |
| Cough/percussion tenderness | 2 |
| Hopping tenderness | 2 |
| WBC >10,000 | 1 |
- • 0-3: Low risk
- • 4-6: Intermediate risk
- • 7-10: High risk
Comprehensive Nursing Assessment
Critical Assessment Priority
Nurses must quickly identify patients with potential appendicitis to prevent complications. Early recognition and appropriate triage can be life-saving, as appendicitis progression follows a predictable but rapid timeline.
Primary Assessment (ABCDE)
Airway & Breathing
- • Assess respiratory rate and pattern
- • Note any signs of respiratory distress
- • Monitor oxygen saturation
- • Observe for shallow breathing due to pain
Circulation
- • Vital signs (BP, HR, temperature)
- • Assess for signs of shock or dehydration
- • Check capillary refill and peripheral pulses
- • Monitor for tachycardia (early sepsis sign)
Disability (Neurological)
- • Level of consciousness and orientation
- • Pain assessment (location, intensity, character)
- • Glasgow Coma Scale if altered mental status
- • Assess for confusion (may indicate sepsis)
Exposure
- • Full abdominal examination
- • Inspect for distension, scars, masses
- • Maintain patient dignity and warmth
- • Look for signs of peritonitis
Focused Abdominal Assessment
Assessment Sequence
Inspection
Look for distension, visible peristalsis, asymmetry, surgical scars
Auscultation
Listen to bowel sounds in all four quadrants before palpation
Light Palpation
Begin away from painful area, assess for tenderness and guarding
Special Tests
Perform McBurney’s, Rovsing’s, psoas, and obturator signs
Assessment Memory Aid
- Inspection first
- Never palpate painful area first
- Sounds before touch (auscultation)
- Palpation light then deep
- Examine for rebound tenderness
- Check special signs
- Time symptoms and progression
Pain Assessment in Appendicitis
Location Progression
Pain Characteristics
- • Initially crampy, colicky
- • Becomes constant, sharp
- • Worsens with movement
- • Coughing/sneezing intensifies
- • Walking bent forward
Pain Scale Usage
- • Use age-appropriate scales
- • Document initial score
- • Monitor progression
- • Note response to position
- • Assess with movement
Key Nursing Assessment Points
What to Document
- • Exact time of symptom onset
- • Pain migration pattern and timing
- • Associated symptoms (nausea, vomiting, fever)
- • Last oral intake and bowel movement
- • Medications taken for pain relief
- • Position of comfort
Red Flag Signs
- • Sudden severe pain relief (may indicate perforation)
- • High fever (>102°F) with rigidity
- • Hypotension or tachycardia
- • Altered mental status
- • Abdominal distension
- • Cessation of bowel sounds
Evidence-Based Nursing Interventions
Critical “DO NOT” Guidelines
Absolutely Avoid
- • NO heat application to abdomen
- • NO enemas or cathartics
- • NO oral intake until cleared
- • NO strong analgesics before diagnosis
Why These Are Dangerous
- • Heat can cause perforation
- • Enemas increase perforation risk
- • Oral intake contraindicated pre-surgery
- • Pain masking delays diagnosis
Pre-Operative Interventions
Immediate Stabilization
- IV Access: Establish large-bore IV for fluids and medications
- Fluid Resuscitation: Normal saline or lactated Ringer’s as ordered
- NPO Status: Nothing by mouth in preparation for surgery
- Positioning: Semi-Fowler’s or position of comfort
Medication Administration
| Medication | Purpose | Nursing Considerations |
|---|---|---|
| Antibiotics | Infection prevention | Give within 1 hour of surgery |
| Analgesics | Pain management | Avoid masking diagnostic signs |
| Antiemetics | Nausea control | Monitor for extrapyramidal effects |
Pre-Operative Preparation
Physical Preparation
- • Informed consent obtained
- • Surgical site marking
- • Pre-operative shower/prep
- • Remove jewelry, dentures
Documentation
- • Baseline vital signs
- • Pain assessment
- • Allergies verified
- • Time of last oral intake
Post-Operative Care
Immediate Post-Op Monitoring
Vital Signs
- • Every 15 min x 4, then every 30 min
- • Monitor for signs of shock
- • Temperature elevation patterns
- • Respiratory status assessment
Surgical Site
- • Inspect dressing for drainage
- • Monitor for bleeding
- • Assess for signs of infection
- • Document wound characteristics
Early Mobilization Plan
6 Hours Post-Op
Assist with turning, deep breathing, coughing exercises
12 Hours Post-Op
Assist to sitting position, dangling legs
24 Hours Post-Op
Ambulation with assistance, progressive activity
Complication Monitoring
Watch For
- • Increased abdominal pain
- • Fever >101.5°F after 48h
- • Purulent wound drainage
- • Abdominal distension
- • Absent bowel sounds >48h
Immediate Actions
- • Notify physician immediately
- • Document findings thoroughly
- • Prepare for diagnostic tests
- • Monitor vital signs closely
- • Ensure IV access patent
Pain Management Strategies
Pain Management Memory Aid: “PQRST”
Provocative
What makes it worse/better?
Quality
Sharp, dull, crampy?
Region
Location and radiation
Severity
0-10 pain scale
Timing
Onset, duration, pattern
Complications of Appendicitis
Early Complications
Perforation (15-20% of cases)
Risk Factors
- • Delayed diagnosis >24 hours
- • Age <5 or >65 years
- • Retrocecal position
- • Immunocompromised state
Clinical Signs
- • Sudden pain relief followed by worsening
- • High fever (>102°F)
- • Abdominal rigidity
- • Tachycardia and hypotension
Abscess Formation
Localized collection of pus, usually occurs when perforation is contained by omentum and adjacent organs.
Generalized Peritonitis
Widespread inflammation of peritoneal cavity due to spillage of infected appendiceal contents.
Late Complications
Post-Operative Complications
| Complication | Incidence | Time Frame |
|---|---|---|
| Wound infection | 3-5% | 3-7 days |
| Intra-abdominal abscess | 2-4% | 5-10 days |
| Ileus | 5-10% | 1-3 days |
| Adhesions | 10-15% | Weeks to years |
Nursing Alert Signs
Immediate Concerns
- Fever >101.5°F after 48h
- Tachycardia >100 bpm
- Respiratory distress
- Altered mental status
Abdominal Signs
- Increasing distension
- Absent bowel sounds
- Purulent drainage
- Increasing rigidity
Prevention Strategies
Early Recognition
Prompt identification and treatment within 24 hours significantly reduces complication rates.
Multidisciplinary Care
Coordinated approach between nursing, surgical, and pharmacy teams optimizes outcomes.
Evidence-Based Protocols
Following standardized care pathways reduces variation and improves patient safety.
Patient & Family Education
Education Goals
Effective patient education for appendicitis focuses on recognition of symptoms, post-operative care, and prevention of complications. Education should be tailored to the patient’s age, literacy level, and cultural background.
Recognition
Symptom awareness
Recovery
Post-op care
Prevention
Complication avoidance
Pre-Operative Education
What to Expect
- Surgery Timing: Usually within 12-24 hours of diagnosis
- Procedure Duration: 30-60 minutes (laparoscopic), 1-2 hours (open)
- Hospital Stay: 1-3 days depending on complexity
- Recovery Time: 2-4 weeks for full activity
Pre-Surgery Instructions
Do
- • Remove all jewelry and makeup
- • Shower with antibacterial soap
- • Arrange post-op transportation
- • Bring list of current medications
Don’t
- • Eat or drink anything (NPO)
- • Take medications unless approved
- • Use lotions or deodorant
- • Smoke before surgery
Post-Operative Education
Recovery Timeline
First 24 Hours
Clear liquids, walking, pain management
Days 2-3
Regular diet, increased activity, home discharge
Week 1
Light activities, follow-up appointment
Weeks 2-4
Gradual return to normal activities
Home Care Instructions
| Activity | Instructions |
|---|---|
| Wound Care | Keep dry for 48h, then gentle washing allowed |
| Diet | Start with clear liquids, advance as tolerated |
| Activity | No lifting >10 lbs for 2 weeks |
| Medications | Take pain medication as prescribed |
When to Seek Medical Attention
Call 911 Immediately If
- Severe abdominal pain with fever >102°F
- Signs of shock (dizziness, rapid pulse, confusion)
- Uncontrolled vomiting with dehydration
- Chest pain or severe breathing difficulty
Contact Healthcare Provider If
- Fever >101°F that persists
- Wound redness, swelling, or drainage
- Increasing abdominal pain
- No bowel movement for 3 days
Patient Education Memory Aid: “TEACH”
Time
Recovery timeline expectations
Emergency
When to seek help
Activity
What you can/cannot do
Care
Wound and self-care
Help
Support resources
Evidence-Based Practice & Current Research
Current Evidence Trends in Appendicitis Management
Recent research has transformed appendicitis care, with evidence supporting conservative antibiotic therapy for uncomplicated cases, improved diagnostic accuracy through clinical scoring systems, and enhanced recovery protocols that optimize patient outcomes while reducing healthcare costs.
Antibiotic Therapy Research
Conservative Management Evidence
Key Findings
- • 70-80% success rate with antibiotics alone for uncomplicated appendicitis
- • Lower morbidity compared to immediate surgery
- • 20-30% eventually require surgery within 1 year
- • Cost-effective approach in selected patients
Selection Criteria
- • Uncomplicated appendicitis on imaging
- • No signs of perforation or abscess
- • Patient able to tolerate oral intake
- • Close follow-up possible
Nursing Implications
- Enhanced patient monitoring and assessment skills required
- Patient education about symptom progression critical
- Clear communication pathways for deterioration
- Detailed documentation of symptom changes
Diagnostic Innovations
Biomarker Research
| Biomarker | Sensitivity | Clinical Use |
|---|---|---|
| Calprotectin | 85-90% | Early detection |
| Procalcitonin | 70-80% | Severity assessment |
| Interleukin-6 | 75-85% | Inflammation marker |
AI-Assisted Diagnosis
Machine learning algorithms are being developed to improve diagnostic accuracy by analyzing clinical data, imaging, and laboratory results.
- • 95%+ accuracy in image interpretation
- • Reduced diagnostic time by 30-40%
- • Improved consistency across providers
Quality Improvement Initiatives
Time-to-Treatment
Standardized Protocols
- • Clinical pathways implementation
- • Nursing-driven protocols
- • Standardized order sets
- • Quality metrics tracking
Patient Outcomes
- • Length of stay reduction
- • Decreased readmission rates
- • Improved patient satisfaction
- • Lower complication rates
Evidence-Based Practice Memory Aid: “RESEARCH”
R – Review
Current literature and guidelines
E – Evaluate
Quality of evidence
S – Synthesize
Best available evidence
E – Examine
Patient preferences and values
A – Apply
Evidence to clinical practice
R – Re-evaluate
Outcomes and effectiveness
C – Continuous
Quality improvement
H – Healthcare
Team collaboration
Global Best Practices in Appendicitis Care
International Approaches to Appendicitis Management
Healthcare systems worldwide have developed innovative approaches to appendicitis care, focusing on early diagnosis, conservative management options, and improved patient outcomes. These global practices provide valuable insights for optimizing nursing care and patient management strategies.
Scandinavian Model
Finland & Sweden Approach
Conservative-First Strategy
- • 70% of uncomplicated cases treated with antibiotics first
- • Surgery reserved for failed conservative treatment
- • Reduced healthcare costs by 25-30%
- • Lower complication rates overall
Nursing Excellence Features
- • Specialized appendicitis assessment protocols
- • Extended monitoring capabilities
- • Patient education specialists
- • 24/7 telephone consultation services
Outcomes Achieved
- • 95% patient satisfaction rates
- • 20% reduction in unnecessary surgeries
- • Shorter hospital stays
- • Lower readmission rates
Dutch Quality Initiative
Netherlands Excellence Program
Standardized Care Pathways
- • National guidelines implementation
- • Mandatory quality reporting
- • Continuous professional development
- • Inter-hospital best practice sharing
Technology Integration
- • AI-assisted diagnostic support systems
- • Electronic scoring system automation
- • Real-time quality metrics dashboards
- • Patient-reported outcome tracking
Nursing Innovation
- • Nurse-led appendicitis clinics
- • Advanced practice nurse involvement
- • Comprehensive discharge planning
- • Post-discharge follow-up protocols
Emerging Global Innovations
Mobile Health Solutions
Australia’s HealthDirect
24/7 nurse helpline with appendicitis assessment protocols
UK’s NHS App
Symptom checker with direct hospital referral pathways
Canada’s Virtual Care
Remote monitoring for conservative treatment patients
Education Excellence
Singapore’s Simulation Centers
High-fidelity appendicitis scenarios for nursing education
Germany’s Competency Programs
Specialized appendicitis care certification for nurses
Japan’s Quality Circles
Continuous improvement teams for appendicitis care
Outcome Optimization
Swiss Quality Metrics
Real-time tracking of appendicitis care quality indicators
New Zealand’s ERAS
Enhanced recovery protocols reducing length of stay
