Comprehensive Nursing Care Plan for Dengue Fever
A Guide for Nursing Students
Table of Contents
Introduction to Dengue Fever Pathophysiology & Clinical Manifestations Nursing Assessment Nursing Diagnoses & Care Plans Complications Prevention Strategies Helpful Mnemonics Additional ResourcesIntroduction to Dengue Fever
Dengue fever is a mosquito-borne viral infection caused by the dengue virus (DENV), which belongs to the Flaviviridae family. It is transmitted primarily by the Aedes aegypti mosquito and, to a lesser extent, by Aedes albopictus.
Key Facts
- Dengue is endemic in more than 100 countries in tropical and subtropical regions
- The World Health Organization (WHO) estimates 100-400 million infections yearly
- Four distinct but closely related dengue virus serotypes exist (DENV-1, DENV-2, DENV-3, and DENV-4)
- Recovery from infection by one serotype provides lifelong immunity against that serotype but only partial and temporary protection against other serotypes
- Subsequent infections with different serotypes increase the risk of developing severe dengue
Clinical Classification (WHO)
- Dengue without warning signs: Fever with nausea/vomiting, rash, aches and pains, leukopenia
- Dengue with warning signs: Abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, liver enlargement, increasing hematocrit with decreasing platelets
- Severe dengue: Severe plasma leakage, severe bleeding, or severe organ impairment
Typical Course of Dengue Fever
Incubation Period (4-10 days)
Virus replicates in target tissues. Patient is asymptomatic.
Febrile Phase (2-7 days)
High fever of sudden onset (39-40°C/102-104°F), severe headache, retro-orbital pain, myalgia, arthralgia, nausea, vomiting, and rash.
Critical Phase (24-48 hours)
Occurs around time of defervescence (fever breaking). Period of increased risk for plasma leakage and hemorrhagic manifestations. Patient should be closely monitored.
Recovery Phase (2-7 days)
Gradual reabsorption of extravascular fluid, improved well-being, stable hemodynamic status, diuresis, and recovery of appetite.
Pathophysiology & Clinical Manifestations
Pathophysiology of Dengue Fever
Viral Entry & Replication
Dengue virus enters through mosquito bite and infects dendritic cells and monocytes
Viral Dissemination
Infected cells travel to lymph nodes and spread virus through lymphatic system and bloodstream
Immune Response
Body mounts immune response with cytokine production causing fever and inflammation
Vascular Permeability
Cytokines disrupt endothelial cell junctions causing increased vascular permeability
Plasma Leakage & Thrombocytopenia
Fluid leaks into tissue spaces; platelets decrease due to bone marrow suppression & immune-mediated destruction
Antibody-Dependent Enhancement (ADE)
In secondary infections with a different dengue serotype, pre-existing antibodies from the primary infection may bind to the new serotype but fail to neutralize it. Instead, these antibody-virus complexes can enhance viral entry into cells, leading to higher viral loads and more severe disease.
Clinical Manifestations
Febrile Phase
- High fever (103-105°F)
- Severe headache
- Retro-orbital pain
- Myalgia and arthralgia
- Nausea and vomiting
- Flushed skin
Critical Phase
- Defervescence (temperature drops)
- Plasma leakage
- Pleural effusion
- Ascites
- Hypoproteinemia
- Hemoconcentration
- Shock (in severe cases)
Recovery Phase
- Reabsorption of extravasated fluid
- Improved well-being
- Stable vital signs
- Increased appetite
- Diuresis
- Bradycardia (sometimes)
- Convalescent rash
Warning Signs of Severe Dengue
- Severe abdominal pain
- Persistent vomiting
- Rapid breathing
- Bleeding gums or nose
- Blood in vomit or stool
- Fatigue, restlessness
- Liver enlargement
- Rising hematocrit with falling platelets
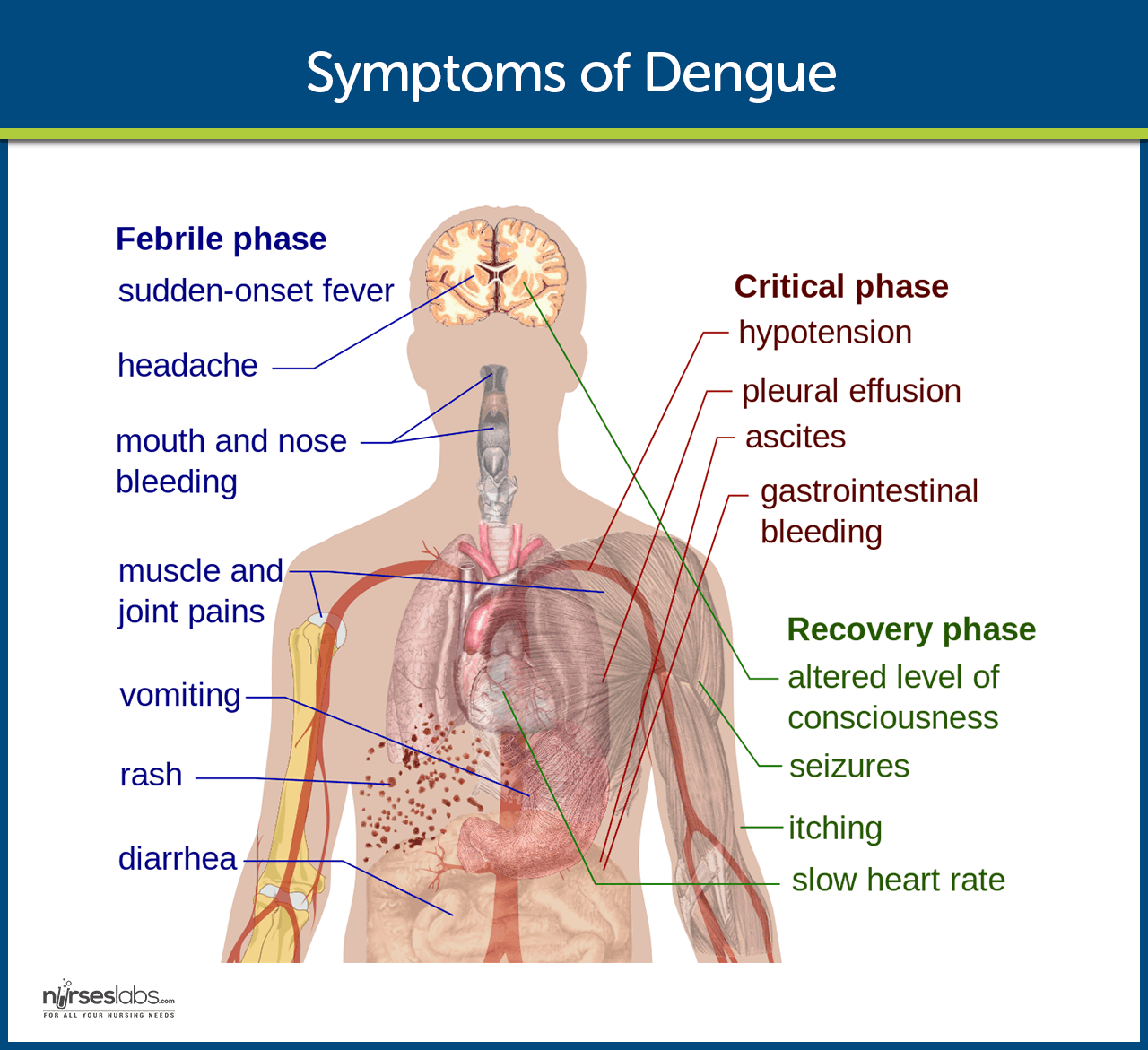
Fig 1: Common symptoms of dengue fever (Source: Nurseslabs)
Nursing Assessment
Comprehensive Assessment for Dengue Fever
Subjective Data (Patient History)
- Travel History: Recent travel to endemic areas within past 14 days
- Mosquito Exposure: History of mosquito bites, especially during daytime
- Onset of Symptoms: Sudden high fever, severe headache, pain behind eyes
- Pain Assessment: Location, duration, character, aggravating/relieving factors of headache, muscle, joint, and bone pain
- Gastrointestinal Symptoms: Nausea, vomiting, loss of appetite, abdominal pain
- Previous Dengue History: Previous episodes of dengue (increases risk of severe dengue)
Objective Data (Physical Examination)
- Vital Signs: Temperature, heart rate, respiratory rate, blood pressure, oxygen saturation
- Skin Assessment: Presence of rash (maculopapular or petechial), flushing, capillary refill time
- Hydration Status: Skin turgor, mucous membranes, urine output
- Bleeding Manifestations: Petechiae, ecchymosis, gum bleeding, epistaxis
- Abdominal Examination: Tenderness, hepatomegaly, ascites
- Respiratory Assessment: Breathing pattern, signs of pleural effusion
- Neurological Assessment: Level of consciousness, irritability, lethargy
Diagnostic Findings
| Laboratory Test | Expected Findings in Dengue | Nursing Implications |
|---|---|---|
| Complete Blood Count (CBC) |
– Leukopenia (WBC <5,000/mm³) – Thrombocytopenia (platelets <150,000/mm³) – Increased hematocrit (>20% from baseline) |
– Monitor for signs of bleeding – Observe for signs of hemoconcentration – Implement bleeding precautions |
| Liver Function Tests |
– Elevated AST and ALT – Mild elevation in bilirubin |
– Assess for jaundice – Monitor for hepatomegaly – Adjust medications metabolized by liver |
| Dengue NS1 Antigen | Positive during first week of illness |
– Early confirmation of diagnosis – Initiate dengue management protocol |
| Dengue Antibody Tests (IgM, IgG) |
– IgM: Positive 5-7 days after onset – IgG: Positive in later stage or secondary infection |
– Helps determine primary vs. secondary infection – Secondary infections have higher risk for severe dengue |
| Coagulation Profile |
– Prolonged PT/PTT – Decreased fibrinogen |
– Increased monitoring for bleeding – Prepare for possible blood product administration |
| Chest X-ray / Ultrasound |
– Pleural effusion – Ascites |
– Monitor respiratory status – Position patient appropriately – Prepare for possible drainage procedures |
Assessment Tip
The tourniquet test can be performed to assess capillary fragility. A blood pressure cuff is inflated to a point between systolic and diastolic pressure for 5 minutes. A positive test shows 20 or more petechiae per square inch and suggests increased capillary fragility, which can occur in dengue fever.
Nursing Diagnoses & Care Plans
The following nursing diagnoses address the most common problems encountered in patients with dengue fever. Each diagnosis includes specific interventions, rationales, and expected outcomes to guide comprehensive nursing care.
1. Hyperthermia
Related to: Inflammatory process secondary to dengue viral infection
As evidenced by: Temperature >38.5°C (101.3°F), flushed skin, tachycardia, chills, headache
Interventions
- Monitor body temperature every 2-4 hours or as indicated
- Administer antipyretics (acetaminophen ONLY) as prescribed
- Apply tepid sponging to forehead, axilla, and groin
- Provide cooling measures like light clothing and reduced room temperature
- Encourage adequate fluid intake (oral or IV) to prevent dehydration
- Document temperature pattern and response to interventions
Rationales
- Regular monitoring detects trends and evaluates effectiveness of interventions
- Acetaminophen reduces fever without affecting platelet function (avoid NSAIDs/aspirin)
- Tepid sponging promotes heat loss through conduction and evaporation
- Environmental modifications facilitate heat dissipation
- Adequate hydration compensates for increased insensible water loss during fever
- Documentation enables evaluation of treatment effectiveness and disease progression
Expected Outcomes
- Body temperature returns to normal range (36.5-37.5°C) within 24-48 hours
- Heart rate and respiratory rate return to patient’s baseline
- Patient reports increased comfort and decreased headache
- No signs of dehydration are present
- Patient/caregiver demonstrates understanding of fever management
Critical Consideration
NEVER administer aspirin, ibuprofen, or other NSAIDs for fever in dengue patients as they may increase the risk of bleeding due to their antiplatelet effects.
2. Risk for Deficient Fluid Volume
Related to: Increased vascular permeability, plasma leakage, fever, vomiting, and decreased oral intake
Risk factors: Hemoconcentration, decreased urinary output, dry mucous membranes, tachycardia, hypotension
Interventions
- Monitor vital signs, especially blood pressure and heart rate, every 1-4 hours
- Maintain strict intake and output monitoring
- Assess skin turgor, mucous membranes, capillary refill, and JVP regularly
- Administer IV fluids as prescribed (typically isotonic crystalloids)
- Weigh patient daily at same time using same scale
- Monitor laboratory values, especially hematocrit, BUN/creatinine ratio
- Encourage oral fluid intake if tolerated
- Position patient appropriately to optimize hemodynamics
Rationales
- Early detection of impending shock by identifying tachycardia and narrowing pulse pressure
- Accurate fluid balance assessment helps guide fluid replacement therapy
- Physical assessment provides immediate indicators of hydration status
- IV fluid restores intravascular volume, especially during critical phase
- Weight changes reflect fluid status (1 kg = approximately 1 liter of fluid)
- Rising hematocrit indicates hemoconcentration due to plasma leakage
- Oral hydration contributes to overall fluid balance when feasible
- Proper positioning enhances venous return and cardiac output
Expected Outcomes
- Vital signs remain within patient’s normal range
- Urine output maintained at >0.5 ml/kg/hr
- Mucous membranes moist, good skin turgor, capillary refill <3 seconds
- Stable weight within 2% of baseline
- Electrolytes within normal range
- Hematocrit stabilizes within normal range
- No signs of fluid overload (crackles, edema, distended neck veins)
Fluid Management Tip
Follow the WHO guideline for fluid management in dengue. During the critical phase, administer the minimum IV fluid volume required to maintain good perfusion and urine output of about 0.5 ml/kg/hr. Avoid excessive fluid administration, which can lead to fluid overload, especially during the recovery phase when extravasated fluid is reabsorbed.
3. Acute Pain
Related to: Inflammatory process, muscle and joint involvement, headache
As evidenced by: Self-reported pain, facial grimacing, guarding behavior, restlessness, changes in vital signs
Interventions
- Assess pain using appropriate scale (0-10) including location, character, intensity
- Administer acetaminophen as prescribed for pain management
- Apply cold or warm compresses to painful joints and muscles as appropriate
- Implement non-pharmacological pain relief measures (positioning, relaxation techniques)
- Provide quiet, comfortable environment
- Limit activity during acute pain episodes
- Document pain assessment before and after interventions
Rationales
- Systematic pain assessment guides appropriate interventions and evaluates effectiveness
- Acetaminophen provides analgesic and antipyretic effects without affecting platelet function
- Temperature therapy reduces muscle spasm and joint inflammation
- Non-pharmacological methods complement medication for enhanced pain relief
- Environmental modifications reduce stimuli that may exacerbate pain
- Rest reduces metabolic demands and may decrease pain intensity
- Documentation enables evaluation of pain management effectiveness
Expected Outcomes
- Patient reports pain reduced to acceptable level (≤3/10) within 30 minutes of intervention
- Vital signs return to patient’s normal range
- Increased participation in self-care activities
- Improved sleep and rest patterns
- Patient demonstrates use of non-pharmacological pain relief techniques
- Patient/caregiver verbalizes understanding of pain management plan
Important Note
Avoid all NSAIDs (ibuprofen, naproxen, aspirin) for pain management in dengue patients due to increased bleeding risk. Use acetaminophen (paracetamol) as the drug of choice for both fever and pain.
4. Risk for Bleeding
Related to: Thrombocytopenia, coagulopathy, vascular changes, prolonged prothrombin time
Risk factors: Platelet count <100,000/mm³, positive tourniquet test, previous bleeding episodes, hematologic abnormalities
Interventions
- Monitor platelet count and coagulation studies
- Assess for bleeding manifestations (petechiae, ecchymosis, epistaxis, gum bleeding, hematemesis, melena)
- Test all body excretions for occult blood
- Implement bleeding precautions (soft toothbrush, electric razor, avoid IM injections)
- Minimize venipuncture and apply prolonged pressure to puncture sites
- Maintain bed rest for severe thrombocytopenia (platelets <20,000/mm³)
- Prepare for platelet transfusion if ordered
- Educate patient/family about bleeding precautions
Rationales
- Laboratory monitoring helps assess bleeding risk and need for intervention
- Early detection of bleeding allows prompt intervention
- Occult blood testing detects bleeding not visibly apparent
- Preventive measures reduce trauma to mucous membranes and skin
- Minimizing invasive procedures reduces potential bleeding sites
- Activity restriction reduces risk of injury and bleeding
- Platelet transfusion may be necessary for severe thrombocytopenia with active bleeding
- Education promotes self-monitoring and adherence to precautions
Expected Outcomes
- No evidence of active bleeding
- Stable hemoglobin and hematocrit values
- Vital signs within patient’s normal range
- Patient/family demonstrates understanding of bleeding precautions
- Patient reports bleeding manifestations promptly
- Platelet count begins to recover within 7-10 days of onset
Bleeding Precautions Mnemonic: “PROTECT”
P – Pressure applied to puncture sites for longer periods
R – Rest during periods of severe thrombocytopenia
O – Oral care with soft toothbrush
T – Trauma prevention through fall precautions
E – Electric razors instead of blades
C – Constipation prevention to avoid straining
T – Test all excretions for occult blood
5. Fatigue
Related to: Inflammatory process, altered body metabolism, inadequate nutrition
As evidenced by: Verbalization of exhaustion, lethargy, decreased performance, inability to maintain normal routines
Interventions
- Assess level of fatigue using standardized scale (0-10)
- Plan care activities to allow for rest periods
- Assist with activities of daily living as needed
- Encourage small, frequent nutrient-dense meals
- Monitor electrolyte levels and replace as prescribed
- Promote adequate sleep environment (reduce noise, light control)
- Implement energy conservation techniques
- Gradually increase activity as tolerated during recovery phase
Rationales
- Quantitative assessment guides interventions and evaluates progress
- Scheduled rest prevents excessive fatigue and promotes recovery
- Assistance conserves patient energy for healing
- Frequent small meals require less energy for digestion while providing nutrition
- Electrolyte imbalances can contribute to fatigue
- Quality sleep promotes healing and reduces fatigue
- Energy conservation techniques maximize available energy
- Gradual increase in activity rebuilds strength without overexertion
Expected Outcomes
- Patient reports decreased fatigue level
- Demonstrates increased ability to participate in self-care
- Verbalizes understanding of energy conservation techniques
- Establishes a balanced activity-rest pattern
- Shows improved nutritional intake
- Demonstrates gradual return to normal activity level during recovery
Energy Conservation Tip
Teach patients to prioritize activities, sit when possible, use assistive devices, and organize the environment to reduce unnecessary steps. Fatigue can persist for weeks after dengue fever, so patients need strategies for the post-discharge period.
6. Ineffective Tissue Perfusion
Related to: Plasma leakage, hypovolemia, and altered blood flow in severe dengue
As evidenced by: Decreased peripheral pulses, skin color changes, cool extremities, altered mental status, reduced urine output
Interventions
- Monitor vital signs, especially blood pressure and pulse pressure
- Assess peripheral circulation (capillary refill, color, temperature)
- Monitor urine output hourly in severe cases
- Administer IV fluids as prescribed
- Assess for signs of shock (tachycardia, hypotension, restlessness)
- Monitor oxygen saturation and administer oxygen if needed
- Position patient to maximize perfusion (supine with legs elevated 15-30°)
- Maintain normothermia
- Monitor level of consciousness
Rationales
- Narrowing pulse pressure is an early sign of shock in dengue
- Peripheral circulation assessment provides early indication of perfusion status
- Urine output reflects renal perfusion and overall volume status
- IV fluids restore intravascular volume and improve perfusion
- Early recognition of shock allows rapid intervention
- Oxygen supplementation improves oxygen delivery to tissues
- Proper positioning enhances venous return and cardiac output
- Temperature regulation reduces metabolic demands on the body
- Mental status changes may indicate cerebral hypoperfusion
Expected Outcomes
- Vital signs within patient’s normal range
- Skin warm and pink with capillary refill <3 seconds
- Urine output >0.5 ml/kg/hour
- Alert and oriented mental status
- Strong peripheral pulses
- No signs of shock
- Oxygen saturation >95% on room air
Warning Signs of Shock
Monitor for narrowing pulse pressure (≤20 mmHg), which can occur before hypotension and is an early sign of shock in dengue. Other early signs include tachycardia, cool extremities, and delayed capillary refill despite normal systolic blood pressure.
7. Impaired Skin Integrity
Related to: Dengue rash, petechiae, ecchymosis, pruritus
As evidenced by: Maculopapular or petechial rash, skin lesions, scratching, complaints of itchiness
Interventions
- Assess skin condition daily, documenting characteristics of rash
- Apply moisturizers to dry skin areas
- Keep fingernails short and clean
- Use mild soap and lukewarm water for bathing
- Apply calamine lotion for pruritus as ordered
- Administer oral antihistamines as prescribed
- Maintain cool ambient temperature
- Use loose, cotton clothing
- Change patient’s position every 2 hours if mobility is limited
Rationales
- Regular assessment allows for tracking progression and identification of complications
- Moisturizers prevent dryness that can exacerbate itching
- Short nails reduce skin damage from scratching
- Mild cleansing products minimize chemical irritation
- Calamine has cooling and anti-pruritic effects
- Antihistamines reduce histamine-mediated itching
- Cool temperatures reduce sweating and related pruritus
- Loose cotton clothing reduces skin irritation and promotes air circulation
- Regular position changes prevent pressure injuries
Expected Outcomes
- Reduced scratching behavior
- Patient reports decreased pruritus
- No evidence of secondary skin infections
- Skin remains intact without excoriation
- Patient demonstrates skin care techniques
- Resolution of rash during recovery phase
Dengue Rash Patterns
Dengue rash typically occurs in two forms: an early flushing erythematous rash during the first 24-48 hours of fever and a later maculopapular or petechial rash as fever subsides. A characteristic “islands of white in a sea of red” appearance may be seen during convalescence.
8. Anxiety
Related to: Unfamiliar environment, diagnostic procedures, knowledge deficit, and uncertainty about disease progression
As evidenced by: Expressed concerns, restlessness, increased questioning, focus on self, insomnia
Interventions
- Assess level of anxiety and specific concerns
- Provide clear, concise information about dengue fever and treatment plan
- Explain procedures and reasons for monitoring
- Create calm, quiet environment
- Use therapeutic communication techniques
- Allow family presence when possible
- Teach relaxation techniques (deep breathing, guided imagery)
- Provide realistic reassurance about prognosis
- Listen actively to concerns
Rationales
- Assessment helps identify specific triggers for targeted intervention
- Knowledge reduces fear of the unknown
- Procedural explanations increase sense of control
- Environmental modifications reduce stimuli that may increase anxiety
- Therapeutic communication builds trust and rapport
- Family support provides comfort and reduces isolation
- Relaxation techniques reduce physiological manifestations of anxiety
- Realistic reassurance prevents false hopes while providing comfort
- Active listening validates concerns and promotes expression of feelings
Expected Outcomes
- Patient reports decreased anxiety levels
- Demonstrates reduced physical symptoms of anxiety (tachycardia, restlessness)
- Uses taught relaxation techniques effectively
- Verbalizes understanding of disease process and treatment
- Exhibits improved sleep patterns
- Participates in decision-making regarding care
Communication Tip
Use the “Ask-Tell-Ask” method: first ASK what the patient knows about dengue, then TELL them relevant information in simple terms, then ASK if they understand or have questions. This approach ensures information is tailored to the patient’s needs and level of understanding.
9. Risk for Ineffective Breathing Pattern
Related to: Pleural effusion, ascites, respiratory muscle fatigue, anxiety
Risk factors: Dyspnea, tachypnea, decreased oxygen saturation, use of accessory muscles, abnormal breath sounds
Interventions
- Monitor respiratory rate, depth, and pattern every 2-4 hours
- Assess lung sounds every 4-8 hours
- Monitor oxygen saturation continuously or regularly
- Position patient to optimize ventilation (semi-Fowler’s or high Fowler’s)
- Administer oxygen as prescribed
- Encourage deep breathing exercises every 2 hours
- Monitor for signs of increasing respiratory distress
- Monitor chest X-ray results for pleural effusion
- Prepare for thoracentesis if ordered for significant effusion
Rationales
- Regular monitoring detects early changes in respiratory status
- Auscultation identifies abnormal breath sounds indicating fluid accumulation
- Oxygen saturation monitoring detects hypoxemia requiring intervention
- Proper positioning reduces work of breathing and improves lung expansion
- Supplemental oxygen improves tissue oxygenation
- Deep breathing exercises prevent atelectasis and improve lung expansion
- Early recognition of respiratory compromise allows prompt intervention
- Radiographic monitoring tracks development or resolution of effusions
- Thoracentesis may be necessary to relieve respiratory distress from large effusions
Expected Outcomes
- Respiratory rate within normal range (12-20 breaths/min)
- Oxygen saturation ≥95% on room air
- Clear breath sounds bilaterally
- No use of accessory muscles for breathing
- Reports no dyspnea
- Demonstrates effective breathing techniques
- Resolution of pleural effusion with treatment
Critical Assessment
Pleural effusion and ascites commonly develop during the critical phase of dengue due to plasma leakage. These can compromise respiratory function and should be closely monitored. Report respiratory rate >30/min, decreasing oxygen saturation, or increased work of breathing immediately.
10. Knowledge Deficit
Related to: Unfamiliarity with dengue fever, home care management, and prevention strategies
As evidenced by: Verbalization of misconceptions, questions, request for information, inappropriate behaviors
Interventions
- Assess current knowledge of dengue fever
- Provide education about disease process, transmission, and warning signs
- Teach medication management (acetaminophen use, avoiding NSAIDs)
- Educate about hydration requirements and oral rehydration solutions
- Instruct on home monitoring of temperature and bleeding signs
- Teach mosquito bite prevention strategies
- Instruct on when to seek medical attention
- Provide written instructions for reference
- Use teach-back method to confirm understanding
Rationales
- Assessment identifies gaps in knowledge for targeted education
- Understanding the disease promotes adherence to treatment and recognition of complications
- Proper medication management prevents NSAID-related bleeding complications
- Adequate hydration is essential to prevent shock and support recovery
- Home monitoring allows early detection of recurrence or complications
- Prevention strategies reduce risk of transmission to others and future infection
- Knowledge of warning signs promotes timely medical intervention
- Written instructions provide reference when verbal information is forgotten
- Teach-back method confirms comprehension and corrects misunderstandings
Expected Outcomes
- Patient/caregiver verbalizes understanding of dengue fever
- Demonstrates correct medication administration
- Describes warning signs requiring medical attention
- Demonstrates preparation of oral rehydration solution
- Explains strategies to prevent mosquito breeding and bites
- Verbalizes post-discharge activity restrictions
- Successfully completes teach-back demonstrations
Warning Signs Mnemonic: “DENGUE ALERT”
D – Dizziness or reduced consciousness
E – Exhaustion or increased fatigue
N – No urine output for 4-6 hours
G – Gum or nose bleeding
U – Unbearable abdominal pain
E – Excessive vomiting (≥3 times in 24 hours)
A – Alertness decreased or lethargy
L – Liver enlargement (>2 cm)
E – Easy bruising or spontaneous bleeding
R – Restlessness or irritability
T – Temperature drops but patient deteriorates
Complications of Dengue Fever
Dengue Hemorrhagic Fever (DHF)
A severe form of dengue characterized by:
- High fever lasting 2-7 days
- Hemorrhagic manifestations (petechiae, ecchymosis, purpura, bleeding from mucosa, GI tract)
- Thrombocytopenia (platelets <100,000/mm³)
- Plasma leakage (hemoconcentration, pleural effusion, ascites)
Nursing Focus: Monitor for bleeding manifestations, implement bleeding precautions, prepare for platelet transfusion, provide meticulous skin care.
Dengue Shock Syndrome (DSS)
The most severe form of dengue, characterized by:
- All criteria of DHF plus circulatory failure
- Rapid, weak pulse with narrow pulse pressure (<20 mmHg)
- Hypotension for age
- Cold, clammy skin
- Restlessness or lethargy
Nursing Focus: Aggressive fluid resuscitation, close hemodynamic monitoring, prepare for ICU transfer, monitor acid-base balance, provide oxygen support.
Organ Involvement
Liver
- Hepatomegaly
- Elevated liver enzymes
- Jaundice
- Acute liver failure (rare)
Neurological
- Encephalopathy
- Seizures
- Altered consciousness
- Guillain-Barré syndrome
Cardiac
- Myocarditis
- Arrhythmias
- Reduced ejection fraction
Renal
- Acute kidney injury
- Proteinuria
- Glomerulonephritis
Nursing Focus: Organ-specific monitoring, supportive care, early recognition of multi-organ dysfunction, interdisciplinary collaboration.
Post-dengue Syndrome
Persistent symptoms after the acute phase, including:
- Fatigue and weakness lasting weeks to months
- Persistent musculoskeletal pain
- Neurocognitive complaints (difficulty concentrating, memory problems)
- Depression and anxiety
- Reduced quality of life
Nursing Focus: Patient education about expected recovery timeline, symptom management, gradual activity progression, psychological support.
Prevention Strategies
Personal Protection Measures
- Protective Clothing: Wear long-sleeved shirts, long pants, socks, and shoes when outdoors
- Insect Repellent: Use EPA-registered repellents containing DEET, picaridin, IR3535, oil of lemon eucalyptus, or 2-undecanone
- Timing: Be especially careful during peak mosquito activity times (early morning and late afternoon)
- Accommodation: Stay in air-conditioned or well-screened housing
- Bed Nets: Use permethrin-treated bed nets if sleeping areas are not screened
Dengue Prevention Mnemonic: “ABCD”
A – Avoid mosquito bites using repellents and protective clothing
B – Be aware of peak biting times (dawn and dusk)
C – Clean up breeding sites by removing stagnant water
D – Defend yourself with screens, nets, and air conditioning
Mosquito Control Measures
- Eliminate Breeding Sites: Remove standing water from containers around homes (flowerpots, buckets, tires, etc.)
- Water Storage: Cover water storage containers with tight-fitting lids
- Biological Control: Introduce larvae-eating fish in water storage containers
- Insecticides: Use approved larvicides in water that cannot be emptied or covered
- Home Protection: Install and maintain window/door screens
- Community Action: Participate in community clean-up campaigns
Community Education
Nurses play a crucial role in community education about dengue prevention. Educational programs should emphasize the “4S strategy” promoted by WHO:
- Search and destroy mosquito breeding places
- Self-protection measures (repellents, clothing)
- Seek early consultation for fever
- Say no to indiscriminate fogging (only during outbreaks)
Helpful Mnemonics for Dengue Fever
Symptoms of Dengue: “DENGUE”
D – Debilitating fever (>101°F/38.3°C)
E – Extreme pain (headache, retroorbital, joints)
N – Nausea and vomiting
G – Gums and other sites bleeding
U – Unwell feeling and fatigue
E – Erythematous rash or petechiae
Phases of Dengue: “FICER”
F – Febrile phase (2-7 days)
I – Incubation period (4-10 days)
C – Critical phase (24-48 hours)
E – Equilibration occurs gradually
R – Recovery phase (2-7 days)
Critical Phase Assessment: “PLASMA LEAK”
P – Pulse pressure narrowing
L – Low platelets (falling trend)
A – Abdominal pain (severe)
S – Serosal effusions (pleural, ascites)
M – Mucosal bleeding
A – Altered mental status
L – Liver enlargement
E – Excessive vomiting
A – Alarming hematocrit rise (>20%)
K – Keep monitoring vital signs
Fluid Management: “CRYSTAL”
C – Calculate fluid requirements carefully
R – Replacement with isotonic crystalloids
Y – Yield to minimum amount needed
S – Strict input-output monitoring
T – Titrate according to vital signs
A – Assess regularly for overload
L – Lab values guide therapy (hematocrit)
Pain Management: “COMFORT”
C – Cool compresses for comfort
O – Only acetaminophen for pain
M – Monitor pain using scale
F – Fever control reduces discomfort
O – Optimize positioning
R – Relaxation techniques help
T – Tackle anxiety which worsens pain
Discharge Education: “MOSQUITO”
M – Medication safety (acetaminophen only)
O – Oral hydration importance
S – Signs requiring immediate care
Q – Quiet rest for recovery
U – Understanding the disease course
I – Inspection for bleeding signs
T – Temperature monitoring at home
O – Organize follow-up appointment
Additional Resources
References for Nursing Care
- World Health Organization (WHO): Dengue and Severe Dengue Fact Sheet
- CDC: Information for Healthcare Providers
- NANDA-I: Nursing Diagnoses: Definitions and Classification 2021-2023
- NIC: Nursing Interventions Classification, 7th Edition
- NOC: Nursing Outcomes Classification, 6th Edition
- PAHO: Dengue: Guidelines for Patient Care in the Region of the Americas
Continued Learning
For nursing students seeking to deepen their understanding of dengue fever management, consider:
- Volunteering in community dengue prevention programs
- Participating in simulation exercises for managing dengue shock
- Following case studies of patients through all phases of dengue
- Reviewing regional guidelines specific to your practice area
- Joining international nursing networks focused on tropical diseases