Nutritional Needs of Infants and Children
Comprehensive Nursing Study Notes
Nutrition during infancy and early childhood is crucial for optimal growth, development, and long-term health outcomes. Proper nutrition establishes healthy eating patterns and can prevent various health conditions later in life.
Critical Periods in Infant Nutrition
Nutritional requirements change rapidly during the first year of life as infants transition from a milk-based diet to consuming family foods. The first 1000 days (from conception to age 2) represent a critical window for establishing optimal health.
Growth and Nutritional Needs
- Infants typically double their birth weight by 5-6 months
- Triple their birth weight by 12 months
- Growth velocity is highest during the first 3 months of life
- Caloric requirements per kilogram decrease as the infant grows
| Age | Average Weight | Caloric Needs | Protein Needs | Fluid Needs |
|---|---|---|---|---|
| 0-3 months | 3.5-6 kg | 110-120 kcal/kg/day | 2.2 g/kg/day | 150 ml/kg/day |
| 4-6 months | 6-8 kg | 100 kcal/kg/day | 1.6 g/kg/day | 130 ml/kg/day |
| 7-12 months | 8-10 kg | 95 kcal/kg/day | 1.5 g/kg/day | 120 ml/kg/day |
| 1-3 years | 10-14 kg | 85 kcal/kg/day | 1.1 g/kg/day | 100 ml/kg/day |
Mnemonic: “GROWTH” – Essential Nutrients for Infants
G – Glucose and carbohydrates (main energy source)
R – Rich proteins (for tissue building and repair)
O – Omega fatty acids (for brain development)
W – Water (for hydration and temperature regulation)
T – Trace minerals (zinc, iron, calcium for development)
H – Vitamins (A, D, E, K, B, C for various functions)
Breastfeeding is considered the gold standard of infant nutrition. Human milk is specifically designed to meet the nutritional needs of infants and changes in composition over time to match an infant’s developmental requirements.
Brain Development
Contains DHA and fatty acids essential for optimal brain growth
Immunity
Provides antibodies and immune factors that protect against infections
Digestive Health
Contains prebiotics that promote healthy gut bacteria
Chronic Disease
Reduces risk of obesity, diabetes, and cardiovascular disease
Benefits for Mother
- Promotes bonding with infant
- Reduces postpartum bleeding
- Speeds return to pre-pregnancy weight
- Reduces risk of breast and ovarian cancer
- Delays return of fertility (natural spacing of pregnancies)
- Reduces risk of type 2 diabetes
Breastfeeding Positions
Cradle Hold
Baby’s head in the crook of your elbow, body along forearm and hand supporting baby’s bottom
Cross-Cradle Hold
Similar to cradle but with opposite arm supporting baby’s head for more control
Football/Clutch Hold
Baby tucked under arm like a football, good for mothers who had C-sections
Side-Lying Position
Mother and baby lying side by side, good for night feeds and recovering from birth

Mnemonic: “LATCH” – Signs of Effective Breastfeeding
L – Lips flanged outward
A – Asymmetrical latch (more areola visible above than below)
T – Tongue visible under breast when lower lip pulled down
C – Chin touching breast
H – Hearing swallowing sounds
Important Considerations
- Breastfeeding is a learned skill for both mother and baby
- Support from healthcare providers, family, and lactation consultants is crucial
- Common challenges include latch issues, nipple pain, and concerns about milk supply
- Proper positioning and latch are key to successful breastfeeding
Composition of Breast Milk
| Type | When Produced | Characteristics | Significance |
|---|---|---|---|
| Colostrum | First 2-4 days | Thick, yellowish, high in protein and antibodies | Provides immunity, cleanses bowel |
| Transitional Milk | Days 4-14 | Increased volume, higher fat and lactose | Bridge between colostrum and mature milk |
| Mature Milk | After 2 weeks | More watery appearance, optimal balance of nutrients | Complete nutrition for growth and development |
| Foremilk | Beginning of feed | Thinner, lower fat content, higher in lactose | Quenches thirst |
| Hindmilk | End of feed | Creamier, higher fat content | Provides satiety and essential calories |
Exclusive breastfeeding means an infant receives only breast milk and no other liquids or solids, not even water (except for oral rehydration solutions, drops or syrups consisting of vitamins, minerals supplements or medicines when needed).
WHO and UNICEF Recommendation
The World Health Organization (WHO) and UNICEF recommend exclusive breastfeeding for the first 6 months of life. After 6 months, complementary foods should be introduced while continuing breastfeeding for up to 2 years or beyond.
Evidence-Based Benefits of Exclusive Breastfeeding
- Reduces infant mortality due to common childhood illnesses
- Speeds recovery during illness
- Provides all the energy and nutrients needed for the first 6 months
- Protects against gastrointestinal infections (particularly important in developing countries)
- Reduces risk of allergies and food intolerances
- Associated with higher IQ scores and better school performance
Challenges to Exclusive Breastfeeding
- Lack of support from family or healthcare providers
- Workplace barriers and short maternity leave
- Insufficient knowledge about breastfeeding techniques
- Misconceptions about milk supply
- Maternal health issues
- Cultural practices that encourage early introduction of other foods
Supporting Exclusive Breastfeeding
- Early initiation within the first hour of birth
- Rooming-in and demand feeding
- Avoid supplementation unless medically indicated
- Proper positioning and attachment
- Breastfeeding education for mothers
- Peer counseling and support groups
Contraindications to Breastfeeding
While breastfeeding is optimal for most infants, there are a few contraindications:
- Infant with galactosemia (inability to metabolize galactose)
- Maternal active untreated tuberculosis
- Maternal HIV infection in settings where artificial feeding is acceptable, feasible, affordable, sustainable, and safe
- Certain medications that are incompatible with breastfeeding
- Maternal use of illicit drugs
Practical Tips for Successful Exclusive Breastfeeding
Feeding Frequency
Newborns typically feed 8-12 times in 24 hours. Feed on demand when baby shows hunger cues rather than on a strict schedule.
Duration of Feeds
Allow baby to finish the first breast completely before offering the second breast. This ensures baby gets hindmilk, which is rich in fat.
Maternal Nutrition
Breastfeeding mothers need about 330-400 extra calories daily, adequate fluid intake, and continued prenatal vitamins.
Signs of Adequate Intake
Monitor wet diapers (6+ per day), bowel movements, weight gain, and overall contentment after feeds.
Mnemonic: “NURSE” – Supporting Exclusive Breastfeeding
N – Nighttime feedings maintained (important for milk supply)
U – Understand hunger cues (feeding on demand)
R – Rest when baby rests (maternal self-care)
S – Skin-to-skin contact (promotes bonding and milk production)
E – Encourage support from family and healthcare providers
While breastfeeding is preferred, there are situations where supplementary or artificial feeding becomes necessary. Supplementary feeding refers to providing additional nutrition alongside breastfeeding, while artificial feeding typically refers to formula feeding.
Indications for Supplementary/Artificial Feeding
- Medical contraindications to breastfeeding
- Insufficient milk supply despite interventions
- Adoption or surrogacy
- Maternal choice
- Maternal illness or medication incompatible with breastfeeding
- Infant with poor weight gain despite optimal breastfeeding
- Multiple births where exclusive breastfeeding may be challenging
Types of Infant Formula
| Type | Composition | Indications | Considerations |
|---|---|---|---|
| Cow’s Milk-Based Formula | Modified cow’s milk protein, lactose, vegetable oils, vitamins, minerals | Standard formula for most healthy infants | Most closely resembles breast milk nutritionally |
| Soy-Based Formula | Soy protein isolate, corn syrup, vegetable oils, vitamins, minerals | Galactosemia, lactose intolerance, milk protein allergy, vegan families | Not recommended for preterm infants; concerns about phytoestrogens |
| Protein Hydrolysate Formula | Partially or extensively hydrolyzed proteins | Milk protein allergy or intolerance, GI disorders | More expensive; bitter taste |
| Amino Acid-Based Formula | Free amino acids, no intact proteins | Severe allergies, multiple food allergies | Most expensive; used when other formulas fail |
| Specialized Preterm Formula | Higher caloric density, protein, calcium, phosphorus | Preterm infants or infants with growth failure | Usually 22-24 kcal/oz compared to standard 20 kcal/oz |
Important Safety Considerations
- Always use clean water and equipment when preparing formula
- Follow manufacturer’s instructions for preparation exactly
- Discard unused prepared formula after 24 hours if refrigerated
- Discard formula left at room temperature after 2 hours
- Never microwave formula – heat in warm water bath instead
- Always test temperature before feeding
Formula Feeding Techniques
Paced Bottle Feeding
Hold baby in semi-upright position, hold bottle horizontally, allow baby to draw nipple in, take breaks to mimic breastfeeding pattern
Side-Lying Position
Similar to breastfeeding side-lying position, promotes bonding and eye contact
Cradle Holding
Mimics breastfeeding position, supports bonding
Upright Position
Helpful for babies with reflux, keeps baby’s head above stomach
Formula Feeding Guidelines by Age
| Age | Amount per Feeding | Frequency | Daily Total (approx.) |
|---|---|---|---|
| 0-1 month | 2-3 oz (60-90 ml) | Every 2-3 hours | 16-24 oz (480-720 ml) |
| 1-2 months | 3-4 oz (90-120 ml) | Every 3-4 hours | 20-28 oz (600-850 ml) |
| 2-4 months | 4-5 oz (120-150 ml) | Every 3-4 hours | 24-32 oz (720-960 ml) |
| 4-6 months | 5-6 oz (150-180 ml) | Every 4-5 hours | 28-32 oz (850-960 ml) |
| 6-12 months | 6-8 oz (180-240 ml) | Every 4-5 hours | 24-32 oz (720-960 ml) |
Mnemonic: “FEEDS” – Safe Formula Preparation
F – Follow instructions exactly for water-to-powder ratio
E – Equipment must be properly sterilized
E – Expiration date must be checked
D – Discard unused formula according to safety guidelines
S – Store prepared formula in refrigerator for no more than 24 hours
Supplementary Feeding Methods
Cup Feeding
Using a small cup to feed expressed breast milk or formula. Good for short-term use and avoiding nipple confusion.
Finger Feeding
Using a tube attached to a clean finger. Useful for babies who have trouble latching.
Supplemental Nursing System (SNS)
Thin tube placed alongside nipple, allowing baby to receive supplement while stimulating breast.
Syringe or Dropper
For small volume supplements. Can be used while baby is at breast or separately.
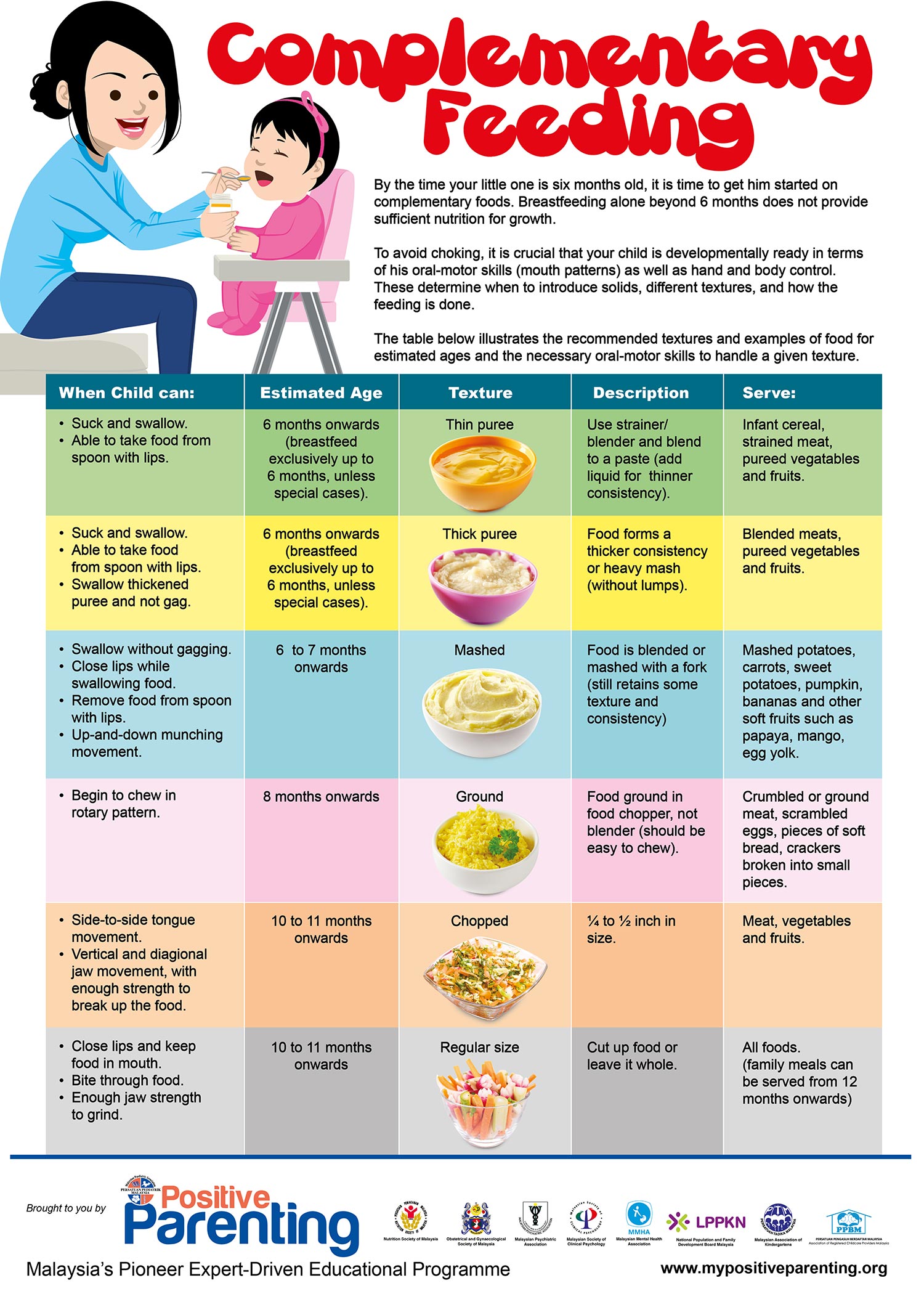
Weaning is the process of gradually introducing solid foods to an infant’s diet while reducing milk feeds. This important transition typically begins around 6 months of age when an infant is developmentally ready.
Signs of Readiness for Weaning
- Able to sit up with minimal support
- Good head and neck control
- Lost tongue-thrust reflex (no longer automatically pushes food out)
- Shows interest in food when others are eating
- Reaches for food and brings objects to mouth
- Opens mouth when offered food
Weaning Timeline
First Foods Introduction
- Single ingredient purées or soft finger foods
- Iron-rich foods (fortified cereals, puréed meat)
- Vegetables and fruits
- One new food every 3-5 days to monitor for allergies
- 1-2 small meals per day alongside milk feeds
Expanding Variety
- Thicker purées and mashed foods
- Soft lumps and textures
- Finger foods that dissolve easily
- Wider variety of tastes and flavors
- 2-3 meals per day alongside milk feeds
Increasing Textures
- More lumpy textures and soft table foods
- Minced or finely chopped foods
- Self-feeding with fingers encouraged
- Introduction of cup for water
- 3 meals and 1-2 snacks per day
Family Foods
- Modified family foods
- Three meals and 2-3 snacks daily
- Introduction of whole cow’s milk (if appropriate)
- Breastfeeding can continue as desired
- Self-feeding with utensils encouraged
Traditional Weaning Approach
Starts with smooth purées and gradually introduces textures:
- Stage 1: Smooth purées (single ingredients)
- Stage 2: Thicker purées with soft lumps
- Stage 3: Mashed foods with more texture
- Stage 4: Chopped foods and soft finger foods
Benefits include controlled introduction of textures and potential reduced choking risk.
Baby-Led Weaning (BLW) Approach
Skips purées and allows baby to self-feed appropriate finger foods:
- Soft, finger-sized pieces of food
- Baby controls what and how much they eat
- Focus on exploration and self-feeding
- Family meals from the beginning
Benefits include development of motor skills, self-regulation, and exposure to textures.
First Foods by Nutrient Need
| Nutrient Need | Recommended Foods | Preparation Tips |
|---|---|---|
| Iron | Iron-fortified infant cereal, puréed meat, poultry, fish, legumes | Cook thoroughly, purée to appropriate texture |
| Zinc | Meat, fortified cereals, legumes | Offer with vitamin C foods to enhance absorption |
| Protein | Puréed meat, poultry, fish, tofu, well-cooked eggs, beans | Ensure adequate cooking, watch for allergic reactions |
| Healthy Fats | Avocado, olive oil, butter, full-fat yogurt (after 6 months) | Small amounts added to purées |
| Vitamins/Minerals | Various fruits and vegetables | Offer a rainbow of colors for nutritional variety |
Foods to Avoid in the First Year
- Honey (risk of infant botulism)
- Cow’s milk as a main drink (before 12 months)
- Added salt and sugar
- Choking hazards (whole nuts, grapes, hot dogs, popcorn, raw carrots)
- Highly processed foods
- Caffeinated or sugary drinks
- Unpasteurized foods
Mnemonic: “SOLID” – Safe Weaning Practices
S – Start with iron-rich foods
O – One new food at a time (wait 3-5 days between new foods)
L – Look for signs of allergies or intolerances
I – Introduce variety of textures and flavors
D – Don’t force feed; respect baby’s hunger and fullness cues
Cultural Considerations in Weaning
Weaning practices vary significantly across cultures, influenced by tradition, available foods, and cultural beliefs about infant development and nutrition.
Asian Traditions
Often feature rice porridge (congee), soft rice with vegetables, and mild spices introduced gradually.
Mediterranean Approach
Emphasis on olive oil, yogurt, vegetables, and herbs introduced early for taste development.
African Practices
May include cereal porridges, mashed plantains, sweet potato, and gradual introduction to family meals.
Key Points in Infant Nutrition
Breastfeeding
- Exclusive for 6 months, continued for 2+ years
- Perfect nutrition, adapts to infant’s needs
- Provides immunity and optimal development
- Beneficial for both mother and baby
Formula Feeding
- Valid alternative when breastfeeding not possible
- Choose appropriate formula type
- Follow safe preparation guidelines
- Practice responsive feeding techniques
Weaning
- Start around 6 months when developmentally ready
- Begin with iron-rich foods
- Gradually introduce variety and textures
- Respect hunger/fullness cues
Nutritional Monitoring
- Regular growth assessments
- Watch for developmental milestones
- Monitor for signs of deficiencies
- Adjust nutrition as needed
Common Nutritional Concerns and Solutions
| Concern | Potential Causes | Nursing Interventions |
|---|---|---|
| Poor Weight Gain | Insufficient intake, absorption issues, increased energy needs | Assess feeding technique, increase frequency or concentration, evaluate for medical issues |
| Iron Deficiency | Insufficient iron-rich foods, excessive milk intake, poor absorption | Introduce iron-rich foods, limit milk to appropriate amounts, consider supplements if recommended |
| Food Allergies | Immune reaction to specific proteins | Introduce one new food at a time, watch for reactions, consult healthcare provider if suspected |
| Constipation | Insufficient fluid, fiber or changing diet | Ensure adequate fluid intake, offer high-fiber foods, check formula preparation |
| Feeding Resistance | Developmental phase, texture sensitivity, pressure to eat | Maintain positive feeding environment, avoid pressure, continue offering variety |
Mnemonic: “CHILD” – Principles of Optimal Infant Nutrition
C – Complete nutrition (appropriate for developmental stage)
H – Hunger and fullness cues (responsive feeding)
I – Individual needs (personalized approach)
L – Loving environment (positive feeding relationship)
D – Developmentally appropriate progression
Final Nursing Considerations
- Support informed parental decision-making
- Provide evidence-based information without judgment
- Consider family circumstances, culture, and preferences
- Regular assessment and adjustment of nutritional plans
- Collaborative approach with healthcare team
- Document nutrition assessments and interventions
