Nursing Management in Common Childhood Respiratory Diseases
Evidence-based nursing care for pediatric patients with respiratory conditions
Purpose: These notes are designed to provide nursing students with comprehensive information about common childhood respiratory conditions, focusing on nursing assessment, interventions, and patient education.
Table of Contents
Acute Nasopharyngitis (Common Cold)
Definition & Pathophysiology
Acute nasopharyngitis, commonly known as the common cold, is an upper respiratory infection that affects the nasal passages and pharynx. It is characterized by inflammation of the mucous membranes lining the nasopharyngeal area.

Pathophysiology involves:
- Viral infection of the nasal epithelium
- Inflammatory response causing vasodilation and increased vascular permeability
- Increased mucus production from goblet cells
- Edema of the nasal mucosa
- Stimulation of nerve endings causing sneezing and cough reflexes
Etiology & Risk Factors
Causes:
- Viral pathogens (over 200 different viruses):
- Rhinovirus (most common – responsible for 30-50% of colds)
- Coronavirus
- Respiratory syncytial virus (RSV)
- Adenovirus
- Parainfluenza virus
- Metapneumovirus
Risk Factors:
- Age: Young children (especially those in daycare settings)
- Seasonal variations: More common in fall and winter
- Weakened immune system
- Close contact with infected individuals
- Poor hand hygiene
- Environmental factors: Cold, dry air
| Viral vs. Bacterial Nasopharyngitis | |
|---|---|
| Feature | Characteristics |
| Viral (90-95% of cases) |
|
| Bacterial (5-10% of cases) |
|
Clinical Manifestations
- Nasal symptoms: Congestion, rhinorrhea, sneezing
- Throat symptoms: Sore throat, irritation, scratchiness
- Systemic symptoms: Low-grade fever, malaise, fatigue
- Other symptoms: Headache, mild body aches, watery eyes
Mnemonic: “COLD”
Nursing Assessment
Physical Assessment:
- Respiratory assessment:
- Respiratory rate, pattern, and depth
- Work of breathing
- Nasal flaring or use of accessory muscles (rare in simple nasopharyngitis)
- ENT assessment:
- Inspect nasal passages for inflammation, discharge
- Inspect throat for erythema
- Palpate lymph nodes (may be slightly enlarged)
- Vital signs: Temperature, heart rate, respiratory rate
Diagnostic Evaluation:
Diagnosis is primarily clinical. Laboratory tests are rarely needed unless complications are suspected.
- Rapid viral tests (if needed to rule out influenza or COVID-19)
- Throat culture (if bacterial infection is suspected)
Nursing Diagnosis:
- Ineffective breathing pattern related to nasal congestion
- Ineffective airway clearance related to increased mucus production
- Hyperthermia related to inflammatory response
- Acute pain related to inflammation of nasal passages and pharynx
- Risk for fluid volume deficit related to increased body temperature and decreased oral intake
- Risk for impaired comfort related to nasal congestion and rhinorrhea
Nursing Interventions
Respiratory Management:
- Positioning: Place the child in a semi-Fowler’s position using pillows to facilitate lung expansion
- Humidification: Provide cool mist humidification to liquefy secretions
- Nasal hygiene: Gentle suction of nasal secretions, particularly in infants who are obligate nose breathers
Hydration Management:
- Fluid intake: Encourage increased fluid intake to thin secretions
- Warm liquids: Offer warm clear fluids (e.g., warm water with honey for children >1 year)
- Monitor: Assess for signs of dehydration (decreased urine output, dry mucous membranes)
Comfort Measures:
- Temperature management: Administer antipyretics as prescribed (acetaminophen or ibuprofen)
- Rest: Encourage adequate rest and sleep
- Nasal decongestants: Normal saline nasal drops/spray to reduce congestion
Key Point: Avoid over-the-counter cold medications in children under 6 years due to risk of side effects and limited evidence of benefit. Caution is advised for children 6-12 years old.
Medical Management:
Treatment is primarily supportive as most cases are viral in origin and self-limiting.
- Antipyretics/analgesics: Acetaminophen, ibuprofen (avoid aspirin in children due to risk of Reye’s syndrome)
- Nasal saline: For congestion relief
- Antibiotics: Not indicated for viral nasopharyngitis; only considered if bacterial infection is confirmed
Patient & Family Education
Home Management Strategies:
- Demonstrate proper technique for nasal suctioning in infants
- Teach parents how to recognize signs of respiratory distress that require medical attention
- Instruct on proper administration of medications
- Advise on adequate fluid intake and nutritional support
- Discuss comfort measures such as humidification and positioning
Prevention Education:
- Hand hygiene: Proper handwashing technique for both child and family members
- Respiratory hygiene: Covering coughs and sneezes with tissues or elbow
- Avoiding sharing personal items with infected individuals
- Cleaning and disinfecting frequently touched surfaces
When to Seek Medical Attention:
Instruct parents to seek immediate medical care if the child develops:
- Difficulty breathing or rapid breathing
- Blue color around the lips or face
- High fever (above 39°C or 102.2°F) that doesn’t respond to antipyretics
- Signs of dehydration (decreased urination, dry mouth, no tears when crying)
- Excessive drowsiness or difficulty waking
- Symptoms lasting longer than 10 days or worsening after 5-7 days
Mind Map: Acute Nasopharyngitis
Tonsillitis
Definition & Pathophysiology
Tonsillitis is an inflammation of the palatine tonsils, which are lymphoid tissue masses located on either side of the oropharynx. As part of Waldeyer’s ring of lymphoid tissue, the tonsils play an important role in the immune system by producing antibodies against inhaled or ingested pathogens.
Pathophysiology involves:
- Infection of tonsillar tissue by viral or bacterial pathogens
- Inflammatory response leading to hyperemia, edema, and exudate formation
- Infiltration by neutrophils and other inflammatory cells
- Enlargement of tonsils due to inflammation and cellular infiltration
- Local pain from inflammation and nerve stimulation
- Potential systemic response including fever and malaise
Etiology & Risk Factors
Causes:
- Viral pathogens (70-80% of cases):
- Adenovirus
- Epstein-Barr virus (EBV)
- Influenza virus
- Parainfluenza virus
- Herpes simplex virus
- Bacterial pathogens (20-30% of cases):
- Group A beta-hemolytic streptococcus (GABHS) – most common bacterial cause
- Staphylococcus aureus
- Haemophilus influenzae
- Streptococcus pneumoniae
- Mycoplasma pneumoniae
Risk Factors:
- Age: Most common in children 5-15 years old
- Frequent exposure to pathogens (school, daycare)
- History of recurrent upper respiratory infections
- Crowded living conditions
- Seasonal variations: More common in winter and early spring
- Contact with infected individuals
| Viral vs. Streptococcal Tonsillitis | |
|---|---|
| Feature | Characteristics |
| Viral Tonsillitis |
|
| Streptococcal Tonsillitis |
|
Clinical Manifestations
- Local symptoms:
- Sore throat (odynophagia)
- Painful swallowing (dysphagia)
- Red, swollen tonsils (with or without exudates)
- Halitosis (bad breath)
- Referred ear pain
- Systemic symptoms:
- Fever (often higher in bacterial infection)
- Headache
- Malaise and fatigue
- Anorexia
- Nausea/vomiting (especially in younger children)
- Abdominal pain (particularly in streptococcal tonsillitis)
Mnemonic: “TONSIL”
Nursing Assessment
Physical Assessment:
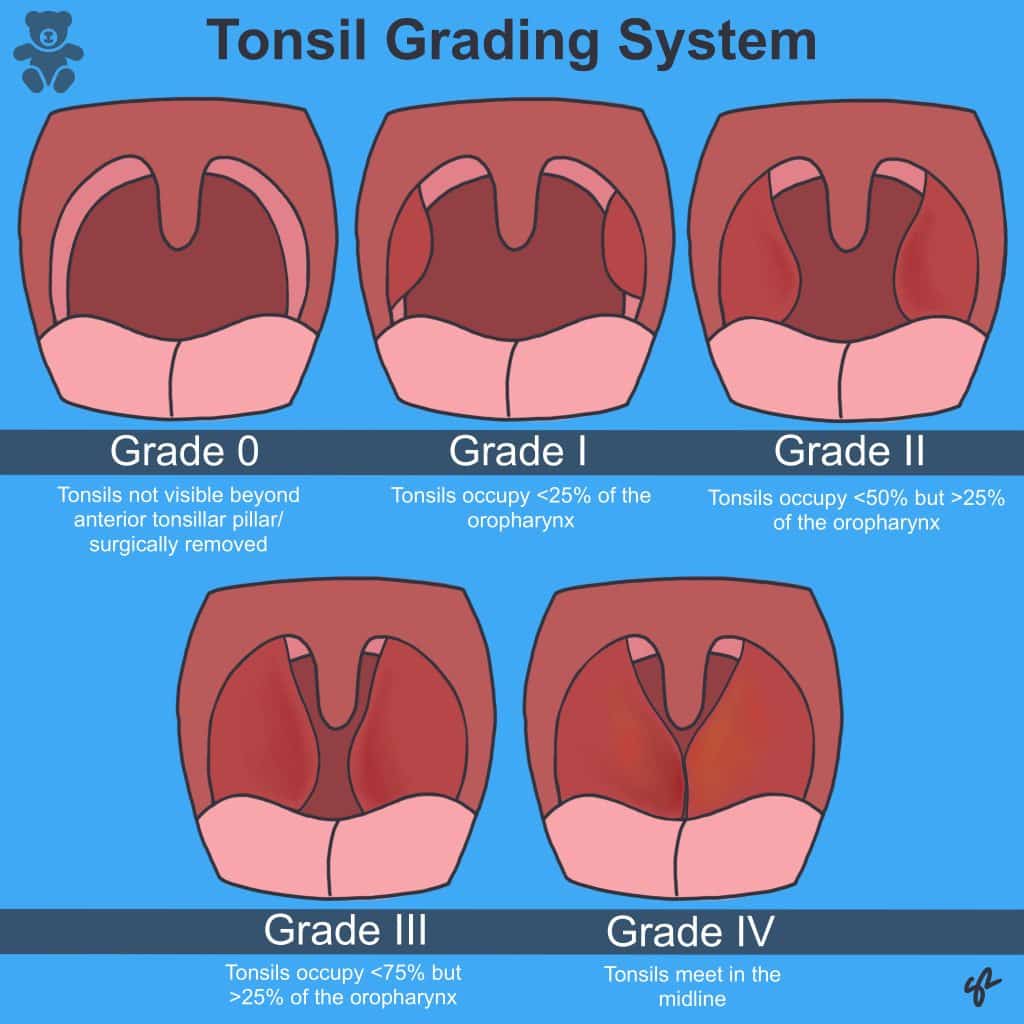
- Oropharyngeal examination:
- Tonsil size and appearance (using tonsil grading scale 1-4)
- Presence of exudates or membrane
- Palatal petechiae or erythema
- Lymph node assessment:
- Palpate for enlarged, tender cervical lymph nodes
- Respiratory assessment:
- Assess for signs of airway obstruction in cases of severe tonsillar enlargement
- Monitor respiratory rate, pattern, and effort
- Vital signs: Temperature, heart rate, respiratory rate, blood pressure
- Hydration status: Assess for signs of dehydration due to painful swallowing
Diagnostic Evaluation:
- Rapid strep test: Quick detection of group A streptococcus
- Throat culture: Gold standard for diagnosing streptococcal infection
- Complete blood count (CBC): May show leukocytosis in bacterial infection
- Monospot test: If infectious mononucleosis is suspected
Nursing Diagnosis:
- Acute pain related to inflammation of tonsillar tissue and pharynx
- Ineffective airway clearance related to enlarged tonsils
- Risk for ineffective breathing pattern related to potential airway obstruction
- Imbalanced nutrition: less than body requirements related to odynophagia
- Risk for deficient fluid volume related to decreased oral intake and fever
- Hyperthermia related to infectious process
Nursing Interventions
Airway Management:
- Position the child in an upright or semi-Fowler’s position to maximize airway patency
- Monitor for signs of respiratory distress or increasing obstruction
- Have emergency equipment readily available if severe tonsillar enlargement is present
Pain and Fever Management:
- Administer analgesics as prescribed (acetaminophen, ibuprofen)
- Offer warm salt water gargles for children old enough to gargle (over 6 years)
- Provide throat lozenges for children over 4 years (to avoid choking hazard)
- Consider ice chips or cold popsicles to numb the throat and provide hydration
Hydration and Nutrition:
- Encourage frequent small sips of cool liquids
- Offer soft, non-irritating foods that are easy to swallow (applesauce, yogurt, smoothies)
- Avoid acidic, spicy, or rough-textured foods that may irritate the throat
- Monitor intake and output to ensure adequate hydration
Medical Management:
- Viral tonsillitis: Supportive care (hydration, rest, antipyretics)
- Bacterial tonsillitis:
- Antibiotics – typically penicillin, amoxicillin, or macrolides for penicillin-allergic patients
- Complete 10-day course to prevent complications like rheumatic fever
- Antipyretics and analgesics for symptom relief
- Recurrent tonsillitis: May require tonsillectomy based on specific criteria:
- 7+ episodes in one year
- 5+ episodes per year for two consecutive years
- 3+ episodes per year for three consecutive years
- Airway obstruction causing sleep apnea
- Peritonsillar abscess
Key Point: Antibiotic therapy is only indicated for confirmed bacterial infections. Unnecessary antibiotic use for viral tonsillitis contributes to antibiotic resistance and exposes children to potential adverse effects.
Patient & Family Education
Home Management:
- Proper administration of prescribed medications, especially completing the full course of antibiotics
- Importance of adequate hydration despite pain with swallowing
- Pain management techniques including gargling, cold foods, and proper dosing of analgesics
- Rest and activity limitations during acute illness
Prevention of Spread:
- Hand hygiene and proper respiratory etiquette
- Avoiding sharing utensils, cups, or personal items
- When to return to school or daycare (generally 24 hours after starting antibiotics for streptococcal tonsillitis)
Post-Tonsillectomy Care (if applicable):
- Pain management expectations (pain often peaks 5-7 days post-surgery)
- Dietary progression (from clear liquids to soft foods)
- Activity restrictions
- Monitoring for complications (bleeding, dehydration, fever)
When to Seek Medical Attention:
Instruct parents to seek immediate medical care if the child develops:
- Difficulty breathing or noisy breathing (stridor)
- Inability to swallow saliva or severe drooling
- Severe throat pain that prevents drinking
- Signs of dehydration
- High fever that doesn’t respond to antipyretics
- Symptoms that worsen despite treatment
- Rash (may indicate scarlet fever with streptococcal infection)
- Post-tonsillectomy: Any bleeding, vomiting bright red blood, or severe pain
Mind Map: Tonsillitis
Croup (Laryngotracheobronchitis)
Definition & Pathophysiology
Croup, also known as laryngotracheobronchitis, is an upper airway infection characterized by inflammation and narrowing of the subglottic region of the trachea. It typically affects children between 6 months and 3 years of age and is notable for its distinctive barking cough.

Pathophysiology involves:
- Viral infection of the respiratory epithelium
- Inflammation and edema of the subglottic region
- Narrowing of the airway, particularly at the level of the cricoid cartilage (the narrowest part of a child’s airway)
- Increased work of breathing due to airway obstruction
- Production of the characteristic barking cough due to airflow through the narrowed, inflamed airway
Key Anatomical Consideration: Children are more susceptible to significant airway obstruction from croup because their airways are smaller in diameter and more compliant (soft) than adult airways. The subglottic region in children is the narrowest part of the airway, making them vulnerable to significant obstruction with even minimal edema.
Etiology & Risk Factors
Causes:
- Viral pathogens (most common):
- Parainfluenza virus types 1, 2, and 3 (most common – 75% of cases)
- Respiratory syncytial virus (RSV)
- Adenovirus
- Influenza A and B
- Human metapneumovirus
- Coronavirus
Risk Factors:
- Age: Peak incidence between 6 months and 3 years (range can be 3 months to 6 years)
- Season: Most common in late fall and early winter
- Male gender: Boys are affected 1.4 times more frequently than girls
- History of previous croup episodes (tendency for recurrence)
- Family history of croup
- Exposure to cigarette smoke
- Underlying airway abnormalities
Clinical Manifestations
- Prodromal phase:
- Mild upper respiratory symptoms (rhinorrhea, mild cough)
- Low-grade fever
- Typically lasts 1-2 days before croup symptoms develop
- Classic symptoms:
- Barking cough (seal-like) – hallmark symptom
- Inspiratory stridor (high-pitched noise during inhalation)
- Hoarseness
- Respiratory distress of varying severity
- Symptoms often worsen at night
Mnemonic: “BARK”
Severity Assessment: Westley Croup Severity Score
| Parameter | 0 points | 1 point | 2 points | 3 points | 4 points | 5 points |
|---|---|---|---|---|---|---|
| Stridor | None | When agitated | At rest | – | – | – |
| Retractions | None | Mild | Moderate | Severe | – | – |
| Air entry | Normal | Decreased | Markedly decreased | – | – | – |
| Cyanosis | None | – | – | – | With agitation | At rest |
| Level of consciousness | Normal | – | – | – | – | Altered |
Score interpretation:
- ≤2: Mild croup
- 3-5: Moderate croup
- 6-11: Severe croup
- ≥12: Impending respiratory failure
Nursing Assessment
Physical Assessment:
- Respiratory assessment:
- Respiratory rate, pattern, and depth
- Work of breathing (retractions, nasal flaring, accessory muscle use)
- Presence and severity of stridor
- Air entry assessment
- Oxygen saturation: Using pulse oximetry
- Vital signs: Temperature, heart rate, respiratory rate, blood pressure
- Mental status: Level of consciousness, agitation, lethargy
- Signs of dehydration: Due to increased work of breathing and possibly decreased intake
Diagnostic Evaluation:
Diagnosis is primarily clinical, based on the characteristic barking cough and stridor. Additional tests may include:
- Lateral neck X-ray: May show the “steeple sign” (narrowing of the subglottic airway)
- Pulse oximetry: To monitor oxygenation status
- Viral testing: Usually not necessary for typical cases
Important Note: Invasive procedures like throat examination with a tongue depressor should be avoided in children with suspected croup as they may precipitate laryngospasm and worsen airway obstruction.
Nursing Diagnosis:
- Ineffective breathing pattern related to airway inflammation and edema
- Ineffective airway clearance related to tracheal edema
- Risk for impaired gas exchange related to upper airway obstruction
- Anxiety (child and parent) related to respiratory distress
- Risk for deficient fluid volume related to increased respiratory effort and decreased intake
- Disturbed sleep pattern related to nocturnal worsening of symptoms
Nursing Interventions
Respiratory Management:
- Maintain calm environment: Agitation worsens stridor and respiratory distress
- Positioning: Allow child to assume position of comfort, usually upright or in parent’s arms
- Humidified air: Provide cool mist humidification (though evidence for this is limited)
- Oxygen therapy: If hypoxemia is present (SpO2 <92%)
- Monitor: Continuous respiratory assessment, particularly for signs of worsening distress
Anxiety Reduction:
- Encourage parental presence and participation in care
- Maintain calm, reassuring approach
- Minimize unnecessary interventions that may upset the child
- Explain procedures to parents and child (as age-appropriate)
Hydration Management:
- Encourage oral fluids if tolerated
- Monitor hydration status
- Intravenous fluids may be necessary in moderate to severe cases with significant respiratory distress
Medical Management:
- Corticosteroids:
- Dexamethasone: Single oral dose (0.6 mg/kg, maximum 16 mg) is the standard of care for all severities of croup
- Acts to reduce airway inflammation and edema
- Onset of action in 2-3 hours, duration of effect up to 72 hours
- Nebulized epinephrine (for moderate to severe croup):
- Racemic epinephrine or L-epinephrine via nebulization
- Provides rapid, temporary relief (30-120 minutes) through vasoconstriction and reduced mucosal edema
- Patients require observation for at least 2-3 hours after administration due to possible rebound effect
- Antipyretics: For fever management (acetaminophen or ibuprofen)
- Antibiotics: Not indicated for viral croup
Nursing Alert: Children receiving nebulized epinephrine require close monitoring for:
- Tachycardia and other side effects (tremors, pallor, agitation)
- Rebound stridor as medication effect wears off
- Signs of worsening respiratory distress
Patient & Family Education
Home Management:
- Comfort measures:
- Exposure to cool, humidified air (cool mist humidifier, opening freezer door)
- Sitting in a steamy bathroom (run hot shower)
- Maintaining calm environment
- Encouraging fluids
- Medication administration:
- Proper dosing of prescribed medications
- Importance of giving full dose of oral steroids if prescribed
- Sleep considerations:
- Elevation of head of bed
- Humidifier use during sleep
- Explain that symptoms often worsen at night
Prevention:
- Hand hygiene
- Avoidance of known sick contacts
- Environmental tobacco smoke avoidance
When to Seek Medical Attention:
Instruct parents to seek immediate medical care if the child develops:
- Increased work of breathing (severe retractions, rapid breathing)
- Stridor at rest that gets louder
- Difficulty speaking or drooling
- Blue or dusky color around the lips or face (cyanosis)
- Decreased level of consciousness or marked agitation
- Signs of dehydration
- Symptoms that worsen despite home management
Course and Prognosis:
- Most children improve within 3-7 days
- The barking cough may persist for up to a week
- Explain that symptoms may worsen at night for 2-3 nights
- Some children are prone to recurrent episodes of croup
Mind Map: Croup (Laryngotracheobronchitis)
Comparison of Pediatric Respiratory Conditions
| Features | Acute Nasopharyngitis | Tonsillitis | Croup |
|---|---|---|---|
| Primary age group | All pediatric ages | 5-15 years | 6 months to 3 years |
| Main pathogens | Rhinovirus, Coronavirus | Viral (70-80%): Adenovirus, EBV Bacterial (20-30%): Group A strep |
Parainfluenza virus (75%), RSV, Influenza |
| Hallmark symptoms | Nasal congestion, rhinorrhea, sneezing | Sore throat, swollen tonsils with or without exudate, dysphagia | Barking cough, inspiratory stridor, hoarseness |
| Fever pattern | Low-grade (<38.5°C) | Variable; higher (>38.5°C) in bacterial infection | Low-grade to moderate |
| Primary assessment focus | Nasal passages, respiratory comfort | Oropharynx, cervical lymph nodes | Respiratory status, stridor, work of breathing |
| Key nursing interventions |
|
|
|
| Medical management | Supportive care; antipyretics | Supportive care for viral; antibiotics for bacterial | Dexamethasone; nebulized epinephrine for moderate-severe |
| Typical duration | 7-10 days | 5-7 days (viral); 24-48 hours after antibiotics (bacterial) | 3-7 days; symptoms worse at night |
| Primary complications | Otitis media, sinusitis | Peritonsillar abscess, dehydration, rheumatic fever (untreated strep) | Respiratory failure, hypoxemia, dehydration |
| Key parental education |
|
|
|
Summary of Nursing Care Principles
Common principles across all three pediatric respiratory conditions include:
- Respiratory monitoring: Regular assessment of respiratory status is essential for early detection of deterioration.
- Hydration: Ensuring adequate fluid intake is critical as respiratory distress and fever increase fluid requirements.
- Comfort measures: Age-appropriate interventions to reduce discomfort and anxiety.
- Fever management: Appropriate use of antipyretics to reduce temperature and improve comfort.
- Parent education: Clear guidance on home management, medication administration, and warning signs requiring medical attention.
- Psychosocial support: Addressing anxiety in both child and parents, particularly with respiratory distress.
- Prevention strategies: Education on hand hygiene and other preventive measures to reduce transmission.
Key Nursing Insight: While these respiratory conditions share some similarities, they each require specific assessment focus and management strategies. The nurse’s ability to differentiate between these conditions and recognize warning signs of deterioration is crucial for optimal pediatric patient outcomes.
References
- Nurseslabs. (2024). Acute Nasopharyngitis Nursing Care Planning and Management. Retrieved from https://nurseslabs.com/acute-nasopharyngitis/
- Nurseslabs. (2024). Tonsillitis and Adenoiditis Nursing Care Management. Retrieved from https://nurseslabs.com/tonsillitis-adenoiditis/
- Nurseslabs. (2024). Croup Syndrome Nursing Care Planning and Management. Retrieved from https://nurseslabs.com/croup-syndrome/
- Nurse.com. (2024). Pediatric Croup: Nursing Diagnosis & Interventions. Retrieved from https://www.nurse.com/clinical-guides/pediatric-croup/
- Feleszko, W., Marengo, R., Vieira, A. S., et al. (2019). Immunity-targeted approaches to the management of chronic and recurrent upper respiratory tract disorders in children. Clinical Otolaryngology, 44(4), 502-510.
- Paul, S. P., Wilkinson, R., & Routley, C. (2014). Management of respiratory tract infections in children. Nursing: Research and Reviews, 4, 135-148.
- Abdou, A., & Lakha, A. (2024). Nursing intervention for children 0-5 years needing intensive care for respiratory infection. Theseus.fi.
- Mayo Clinic. (2023). Croup – Symptoms & causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/croup/symptoms-causes/syc-20350348
- Cleveland Clinic. (2023). Tonsillitis: Symptoms, Causes & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/8277-croup
- UpToDate. (2024). Patient education: Croup in infants and children (Beyond the Basics). Retrieved from https://www.uptodate.com/contents/croup-in-infants-and-children-beyond-the-basics
