Pediatric Respiratory Disorders
Bronchitis & Bronchiolitis
Comprehensive Nursing Education Notes
Introduction
Lower respiratory tract infections are common in childhood and can cause significant morbidity, especially in infants and young children. This guide focuses on two important respiratory conditions: Bronchitis and Bronchiolitis.
While these conditions have similar names and some overlapping symptoms, they affect different parts of the respiratory tract, have distinct pathophysiology, occur in different age groups, and require different nursing approaches.
Key Distinction:
Bronchitis primarily affects the larger airways (bronchi), while Bronchiolitis affects the smaller airways (bronchioles).

Respiratory System Review
Anatomy of the Pediatric Respiratory System
The pediatric respiratory system differs from adults in several important ways:
- Smaller airways – More easily obstructed by inflammation or mucus
- Immature immune system – More susceptible to infections
- Higher metabolic rate – Increased oxygen requirements
- Compliant chest wall – More likely to show retractions during respiratory distress
- Underdeveloped respiratory muscles – Fatigue more easily during respiratory effort
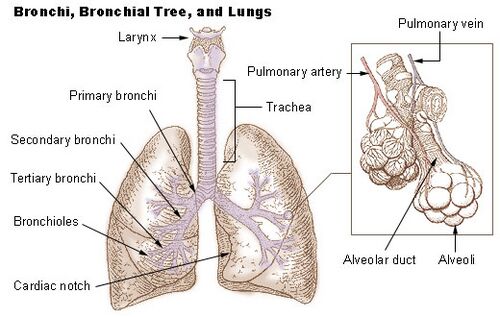
Key Structures Affected in These Conditions
| Structure | Function | In Bronchitis | In Bronchiolitis |
|---|---|---|---|
| Bronchi | Main air passages from trachea to lungs | Primary site of inflammation | May be affected |
| Bronchioles | Smaller airways, 1mm diameter or less | Minimally affected | Primary site of inflammation |
| Epithelial Cells | Line airways; contain cilia | Damaged, increased mucus | Necrosis, sloughing |
| Goblet Cells | Produce mucus | Hyperplasia | Less prominent |
Pediatric Bronchitis
Pathophysiology
Bronchitis is characterized by inflammation of the bronchi, the main passageways that carry air to the lungs. In children, this condition leads to:
- Inflammation of the bronchial mucosa
- Increased mucus production
- Epithelial cell damage and ciliary dysfunction
- Airway hyperresponsiveness
Etiology
Acute Bronchitis: (90-95% cases)
- Viral infections: Rhinovirus, RSV, influenza, parainfluenza
- Bacterial infections: Less common, may include Mycoplasma pneumoniae, Bordetella pertussis
Chronic Bronchitis: (Less common in children)
- Recurrent infections
- Environmental irritants (secondhand smoke, pollution)
- May be associated with asthma or cystic fibrosis
Clinical Presentation
Cardinal Signs & Symptoms:
- Persistent cough (productive or non-productive)
- Low-grade fever (usually < 38.5°C)
- Chest discomfort or soreness
- Fatigue and malaise
- Possible sputum production (clear, white, yellow, or green)
Physical Examination Findings:
- Crackles or coarse breath sounds on auscultation
- Prolonged expiratory phase
- Generally normal respiratory rate (may be increased if fever present)
- Normal oxygen saturation in most cases
Diagnostic Evaluation
Bronchitis is primarily a clinical diagnosis. Limited testing is needed in most cases.
Common Assessments:
- Thorough history and physical examination
- Vital signs assessment
- Respiratory assessment (rate, effort, auscultation)
Further Testing (If Indicated):
- Chest X-ray – Only if pneumonia suspected
- Pulse oximetry – If respiratory distress present
- Sputum culture – Rarely needed, considered if bacterial infection suspected
- Viral testing – Usually not necessary
Management
Important Note:
Antibiotics are generally NOT indicated for bronchitis in children, as most cases are viral in origin.
Supportive Management:
- Adequate hydration (oral fluids)
- Rest
- Antipyretics for fever (acetaminophen or ibuprofen)
- Humidity/cool mist to help loosen secretions
- Avoidance of smoke exposure
Symptom Management:
- Honey for cough in children >1 year (NOT for infants <1 year)
- Over-the-counter cough medications not recommended for children <4 years
- For older children, cough suppressants only at night if sleep is disturbed
When to Consider Antibiotics:
- Suspected Mycoplasma or Bordetella infection
- High fever persisting >3 days
- Purulent sputum with signs of bacterial infection
- Failure to improve after 7-10 days
Nursing Interventions
Assessment:
- Monitor respiratory status (rate, effort, oxygen saturation)
- Assess hydration status
- Monitor temperature and fever pattern
- Evaluate cough (frequency, character, productivity)
- Assess for signs of respiratory distress
Interventions:
- Encourage fluids to maintain hydration
- Position for optimal breathing (elevated head of bed)
- Administer medications as prescribed
- Provide cool mist humidifier
- Educate on proper handwashing
Parent Education:
- Expected course of illness (1-2 weeks)
- Home care instructions
- When to seek medical attention
- Prevention of spread to other family members
- Importance of avoiding smoke exposure
Mnemonic: “BRONCHITIS”
Remember key aspects of pediatric bronchitis assessment and management:
Prevention
- Proper hand hygiene
- Avoidance of known sick contacts
- Annual influenza vaccination
- Avoid exposure to tobacco smoke and air pollutants
- Proper nutrition and hydration to support immune function
- Prompt treatment of upper respiratory infections
Pediatric Bronchiolitis
Pathophysiology
Bronchiolitis involves inflammation of the bronchioles, the smallest airways in the respiratory tract. The disease process includes:
- Viral infection of epithelial cells in the bronchioles
- Necrosis and sloughing of infected epithelial cells
- Edema and infiltration of inflammatory cells
- Increased mucus production and cellular debris
- Airway obstruction, air trapping, and atelectasis
Etiology
Primary Causative Agents:
- Respiratory Syncytial Virus (RSV) – Responsible for 50-80% of cases
- Human Metapneumovirus
- Parainfluenza viruses
- Influenza viruses
- Adenovirus
- Rhinovirus
Epidemiology:
- Peak incidence: November to April in Northern Hemisphere
- Most common in infants 2-6 months of age
- Nearly all children infected with RSV by age 2
- Highly contagious – spread through respiratory droplets
Clinical Presentation
Initial Phase (Days 1-2):
- Rhinorrhea, nasal congestion
- Low-grade fever
- Decreased appetite
- Mild cough
Progressive Phase (Days 3-5):
- Increased respiratory effort
- Persistent cough
- Tachypnea
- Wheezing and/or crackles
- Retractions (subcostal, intercostal, suprasternal)
- Nasal flaring
- Irritability, poor feeding
- Possible apneic episodes (especially in young infants)
Physical Examination Findings:
- Tachypnea (elevated respiratory rate for age)
- Wheezing (often diffuse, bilateral)
- Crackles (fine, inspiratory)
- Prolonged expiratory phase
- Retractions
- Hyperinflation
- Possible hypoxemia (SpO₂ <95%)
Diagnostic Evaluation
Important Note:
Bronchiolitis is primarily a clinical diagnosis. Routine laboratory or radiographic studies are not recommended for diagnosis.
Core Assessments:
- Thorough history and physical examination
- Vital signs (respiratory rate, heart rate, temperature)
- Oxygen saturation via pulse oximetry
- Hydration status assessment
- Work of breathing assessment
Additional Testing (When Indicated):
- Viral testing (RSV, influenza) – May be useful for cohorting
- Chest X-ray – Only if severe disease, atypical presentation, or concern for complication
- Blood work – Not routinely indicated
- Blood gas – For severe respiratory distress
Evidence-Based Management
Evidence-Based Practice:
According to AAP guidelines, routine use of bronchodilators, corticosteroids, or antibiotics is NOT recommended for bronchiolitis.
Supportive Care (Primary Treatment):
- Nasal suctioning to clear secretions
- Adequate hydration (oral or IV if needed)
- Supplemental oxygen for hypoxemia (SpO₂ <90-92%)
- Frequent, small feedings if tolerated
- Fever management (acetaminophen or ibuprofen)
- Minimal handling/clustering care
Advanced Support (Severe Cases):
- High-flow nasal cannula (HFNC) oxygen therapy
- Continuous positive airway pressure (CPAP)
- Mechanical ventilation (rarely needed)
- ICU admission for severe respiratory distress or apnea
Medications (Limited Role):
- Bronchodilators – Not routinely recommended, may try as trial if strong bronchospasm
- Corticosteroids – Not recommended
- Antibiotics – Only for confirmed bacterial coinfection
- Hypertonic saline – May be beneficial for hospitalized infants
- Ribavirin – Very limited use, only for severe immunocompromised cases
Nursing Interventions
Assessment:
- Continuous respiratory assessment using bronchiolitis severity scale
- Monitoring of vital signs and oxygen saturation
- Assessment of hydration status (intake/output, weight, fontanelle)
- Monitor for signs of increasing distress or fatigue
- Assessment of feeding tolerance
Interventions:
- Nasal suctioning before feeds and as needed
- Elevate head of bed 30-45 degrees
- Administer supplemental oxygen as needed
- Ensure proper positioning for optimal breathing
- Support hydration (IV or enteral as appropriate)
- Cluster care to minimize oxygen consumption
- Implement isolation precautions
Parent Education:
- Disease process and expected course (7-14 days)
- Proper nasal suctioning technique
- Signs of respiratory distress requiring medical attention
- Feeding strategies for infants with respiratory distress
- Importance of hand hygiene and isolation measures
- Home oxygen therapy instructions (if applicable)
Bronchiolitis Severity Assessment Scale
Use this tool to assess severity and guide management decisions:
| Parameter | Mild (0) | Moderate (1) | Severe (2) |
|---|---|---|---|
| Respiratory Rate | Normal | Increased | Significantly increased |
| Retractions | None or minimal | Intercostal | Intercostal + subcostal + suprasternal |
| Air Entry | Normal | Decreased | Significantly decreased |
| Wheezing | None or end-expiratory | Entire expiration | Inspiration and expiration |
| Oxygen Saturation | ≥95% on room air | 90-94% on room air | <90% on room air |
| Feeding | Normal | Decreased | Not feeding |
Mild: Score 0-3
Consider outpatient management
Moderate: Score 4-8
Consider hospitalization
Severe: Score 9-12
Hospitalize, consider PICU
Mnemonic: “WHEEZES”
Key factors to assess and manage in bronchiolitis:
Prevention
General Preventive Measures:
- Strict hand hygiene
- Avoid contact with sick individuals
- Breastfeeding (provides protective antibodies)
- Avoid secondhand smoke exposure
- Proper respiratory hygiene/cough etiquette
- Cleaning and disinfecting surfaces
Specific RSV Prophylaxis – Palivizumab:
Monthly intramuscular injections during RSV season for high-risk infants:
- Premature infants born ≤29 weeks gestation and <12 months of age
- Infants with chronic lung disease of prematurity requiring medical therapy
- Infants with hemodynamically significant congenital heart disease
- Infants with severe immunodeficiency
- Children <2 years with neuromuscular disorders affecting respiratory function
Comparison: Bronchitis vs. Bronchiolitis
| Feature | Bronchitis | Bronchiolitis |
|---|---|---|
| Affected Airways | Larger airways (bronchi) | Smaller airways (bronchioles) |
| Age Group | All ages, less common in young infants | Primarily infants <12 months (peak 2-6 months) |
| Primary Etiology | Various viruses (rhinovirus, influenza), occasionally bacterial | RSV (50-80%), other respiratory viruses |
| Cardinal Symptoms | Persistent cough, possibly productive | Wheezing, increased work of breathing |
| Physical Exam Findings | Coarse breath sounds, occasional crackles | Wheezing, crackles, retractions, nasal flaring |
| Typical Duration | 7-10 days | 7-14 days (peak symptoms days 3-5) |
| Oxygen Requirement | Rarely needed | Common in moderate to severe cases |
| Hospitalization Rate | Low | High (1-3% of all infants) |
| Seasonal Pattern | Year-round, peaks winter | Strong winter/spring seasonality |
| Primary Management | Supportive care, rarely requires hospitalization | Supportive care, may require respiratory support |
Key Nursing Considerations
- Assess for age-appropriate respiratory rate and work of breathing
- Vital signs monitoring should include respiratory rate, heart rate, temperature, and oxygen saturation
- Younger patients (especially infants <3 months) with bronchiolitis are at higher risk for apnea and severe disease
- Bronchiolitis typically requires closer monitoring than bronchitis
- Dehydration is a common complication in both conditions, especially in young infants
- Use appropriate isolation precautions to prevent spread
- Family education is essential for both home management and prevention of future episodes
Red Flags Requiring Immediate Attention
- Respiratory rate >60 breaths/minute
- Severe retractions or grunting
- Cyanosis or oxygen saturation <90%
- Lethargy or altered mental status
- Apnea episodes
- Inability to feed or dehydration
- Deteriorating condition despite appropriate therapy
- High fever (>39°C) in infants <3 months
Respiratory Infections: Mind Map
/bronchiolitis-diagram.jpg)
Bronchitis Process Flow
Causative Agents
- Viral pathogens (90-95%)
- Bacterial infections (occasionally)
- Environmental irritants
Pathophysiology
- Irritation of bronchial epithelium
- Inflammation of larger airways
- Increased mucus production
- Ciliary dysfunction
Clinical Manifestations
- Persistent cough (productive or non-productive)
- Low-grade fever
- Chest discomfort
- Fatigue
- Coarse breath sounds
Management Approach
- Supportive care (hydration, rest)
- Symptom management
- Avoid unnecessary antibiotics
- Monitor for improvement (7-10 days)
- Parent education for home care
Bronchiolitis Process Flow
Causative Agents
- RSV (50-80% of cases)
- Human metapneumovirus
- Parainfluenza, Influenza
- Rhinovirus, Adenovirus
Pathophysiology
- Viral infection of bronchiolar epithelium
- Epithelial necrosis and sloughing
- Inflammatory cell infiltration
- Edema of bronchiolar wall
- Mucus plugging and debris
- Air trapping and atelectasis
Clinical Manifestations
- Rhinorrhea → cough → respiratory distress
- Wheezing and crackles
- Tachypnea and retractions
- Nasal flaring
- Feeding difficulties
- Hypoxemia
- Possible apnea (in young infants)
Management Approach
- Supportive care
- Nasal suctioning
- Oxygen supplementation if needed
- Careful fluid management
- Monitoring respiratory status
- Possible hospitalization for severe cases
- Respiratory support (HFNC, CPAP if indicated)
Evidence-Based Practice Guidelines
Bronchitis Guidelines
Key recommendations from the American Academy of Family Physicians (AAFP) and other societies:
- Diagnosis: Primarily clinical based on history and physical examination
- Antibiotics: Generally not recommended for uncomplicated acute bronchitis
- Imaging: Chest X-rays not routinely recommended unless pneumonia suspected
- Bronchodilators: Not routinely recommended unless wheezing or underlying reactive airway disease present
- Cough management: Consider honey for children >1 year of age; avoid cough medications in children <4 years
- Parent education: Emphasize expected duration of cough (up to 3 weeks)
Bronchiolitis Guidelines
Key recommendations from the American Academy of Pediatrics (AAP) Clinical Practice Guidelines:
- Diagnosis: Clinical diagnosis based on history and physical examination
- Testing: Routine viral testing not recommended
- Chest X-ray: Not routinely recommended
- Bronchodilators: Not recommended for routine use
- Corticosteroids: Not recommended
- Antibiotics: Not recommended unless bacterial infection confirmed
- Hypertonic saline: May be beneficial for hospitalized patients
- Suctioning: Nasal suctioning as needed for comfort
Nursing Care Recommendations
Evidence-based nursing interventions for both conditions:
Assessment
- Use validated assessment tools appropriate for condition and age
- Monitor vital signs, including respiratory rate and oxygen saturation
- Assess work of breathing using standardized criteria
- Regular hydration status evaluation
- Document symptom progression
Interventions
- Maintain adequate hydration
- Position for optimal breathing
- Cluster care to minimize energy expenditure
- Nasal suctioning as needed
- Maintain appropriate infection control practices
- Implement oxygen therapy as indicated
Case Studies for Clinical Application
Case Study: Bronchitis
Patient: 7-year-old male presenting with 4-day history of cough, low-grade fever, and mild chest discomfort. Previously healthy with no significant past medical history.
Assessment Findings:
- Temperature: 38.1°C
- Respiratory rate: 26 breaths/minute
- Heart rate: 98 beats/minute
- Oxygen saturation: 97% on room air
- Productive cough with clear sputum
- Coarse breath sounds on auscultation
- No retractions or nasal flaring
Nursing Diagnosis:
- Ineffective airway clearance related to increased mucus production
- Risk for dehydration related to fever and decreased oral intake
- Acute pain (chest discomfort) related to persistent coughing
Nursing Interventions:
- Administer antipyretics for fever as ordered
- Encourage increased fluid intake
- Educate on deep breathing exercises
- Provide honey (1-2 tsp) before bedtime for cough (appropriate for age >1 year)
- Educate family on expected course of illness
- Instruct on importance of hand hygiene
Expected Outcomes:
- Improved airway clearance within 3-5 days
- Maintained adequate hydration
- Reduced frequency of cough within 7 days
- Complete resolution of symptoms within 10-14 days
- Family demonstrates understanding of home care instructions
Case Study: Bronchiolitis
Patient: 4-month-old female presenting with 2-day history of rhinorrhea, cough, and increased work of breathing. Born at term with no significant past medical history.
Assessment Findings:
- Temperature: 38.3°C
- Respiratory rate: 58 breaths/minute
- Heart rate: 162 beats/minute
- Oxygen saturation: 92% on room air
- Moderate subcostal and intercostal retractions
- Diffuse wheezing on auscultation
- Nasal flaring
- Decreased feeding (taking only half of normal volume)
Nursing Diagnosis:
- Ineffective breathing pattern related to airway inflammation and obstruction
- Risk for dehydration related to increased respiratory rate and decreased oral intake
- Impaired gas exchange related to airway narrowing and mucus obstruction
- Risk for infection transmission related to contagious respiratory virus
Nursing Interventions:
- Administer supplemental oxygen to maintain SpO₂ >92%
- Perform nasal suctioning before feeds and as needed
- Position with head of bed elevated 30°
- Monitor vital signs and oxygen saturation every 2-4 hours
- Administer small, frequent feedings
- Maintain fluid balance with IV fluids if necessary
- Implement contact/droplet precautions
- Monitor for signs of respiratory fatigue or deterioration
Expected Outcomes:
- Maintained oxygen saturation >92%
- Decreased work of breathing within 48-72 hours
- Improved feeding within 3-5 days
- Adequate hydration maintained throughout illness
- No spread of infection to other patients
- Family demonstrates understanding of home care plan at discharge
Self-Assessment Questions
Test Your Knowledge
1. Which of the following is the most common causative agent of bronchiolitis in infants?
a) Rhinovirus
b) Respiratory Syncytial Virus (RSV)
c) Influenza virus
d) Mycoplasma pneumoniae
Hover for answer:
2. Which of the following is NOT typically indicated in the treatment of pediatric bronchitis?
a) Rest
b) Adequate hydration
c) Routine antibiotics
d) Antipyretics for fever
Hover for answer:
3. A 3-month-old infant with bronchiolitis has which of the following clinical findings that would indicate severe disease requiring hospitalization?
a) Respiratory rate of 35 breaths/minute
b) Oxygen saturation of 97% on room air
c) Mild intercostal retractions
d) Oxygen saturation of 89% on room air
Hover for answer:
4. Which anatomical structure is primarily affected in bronchitis?
a) Bronchioles
b) Alveoli
c) Bronchi
d) Trachea
Hover for answer:
5. Which nursing intervention is NOT appropriate for an infant with bronchiolitis?
a) Nasal suctioning before feeds
b) Honey for cough suppression
c) Elevation of the head of bed
d) Small, frequent feedings
Hover for answer:
6. Which of the following is a key distinguishing feature between bronchitis and bronchiolitis?
a) Presence of wheezing
b) Age of affected patients
c) Viral etiology
d) Need for antipyretics
Hover for answer:
References
- American Academy of Pediatrics. (2014). Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis. Pediatrics, 134(5), e1474-e1502.
- American Academy of Family Physicians. (2016). Diagnosis and Treatment of Acute Bronchitis. American Family Physician, 94(7), 560-565.
- Ralston, S. L., Lieberthal, A. S., Meissner, H. C., et al. (2014). Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis. Pediatrics, 134(5), e1474-e1502.
- The Royal Children’s Hospital Melbourne. (2022). Clinical Practice Guidelines: Bronchiolitis. Retrieved from https://www.rch.org.au/clinicalguide/guideline_index/Bronchiolitis/
- Cincinnati Children’s Hospital Medical Center. (2022). Evidence-based clinical practice guideline for medical management of bronchiolitis in infants less than 1 year of age presenting with a first time episode.
- Friedman, J. N., Rieder, M. J., & Walton, J. M. (2014). Bronchiolitis: Recommendations for diagnosis, monitoring and management of children one to 24 months of age. Paediatrics & Child Health, 19(9), 485-491.
- Kinkade, S., & Long, N. A. (2016). Acute Bronchitis. American Family Physician, 94(7), 560-565.
- Meissner, H. C. (2016). Viral Bronchiolitis in Children. The New England Journal of Medicine, 374(1), 62-72.
- Smith, D. K., Seales, S., & Budzik, C. (2017). Respiratory Syncytial Virus Bronchiolitis in Children. American Family Physician, 95(2), 94-99.
- Zorc, J. J., & Hall, C. B. (2010). Bronchiolitis: Recent Evidence on Diagnosis and Management. Pediatrics, 125(2), 342-349.
